Indication
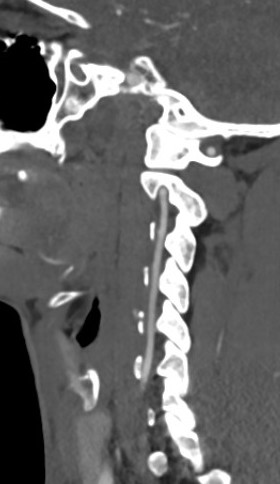
Anterior approach to subaxial spine
C3 - T1
Conditions
Trauma
Radiculopathy
Myelopathy
Infection
Tumour
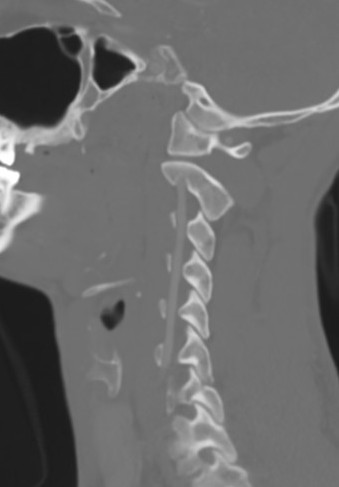
Position
Head
- Supine in tongs
- taped on head board with head taped
- neck slightly extended
Shoulders can be taped down for access to lower cervical spine
Reverse Trendelenberg 30°
- reduce venous bleeding
Turn head away from side of incision
Landmarks
Fluoroscopy for levels
Landmarks
- Hyoid cartilage C3/4
- Thyroid cartilage C4/5
- Cricoid cartilage C6
- Carotid tuberble C6
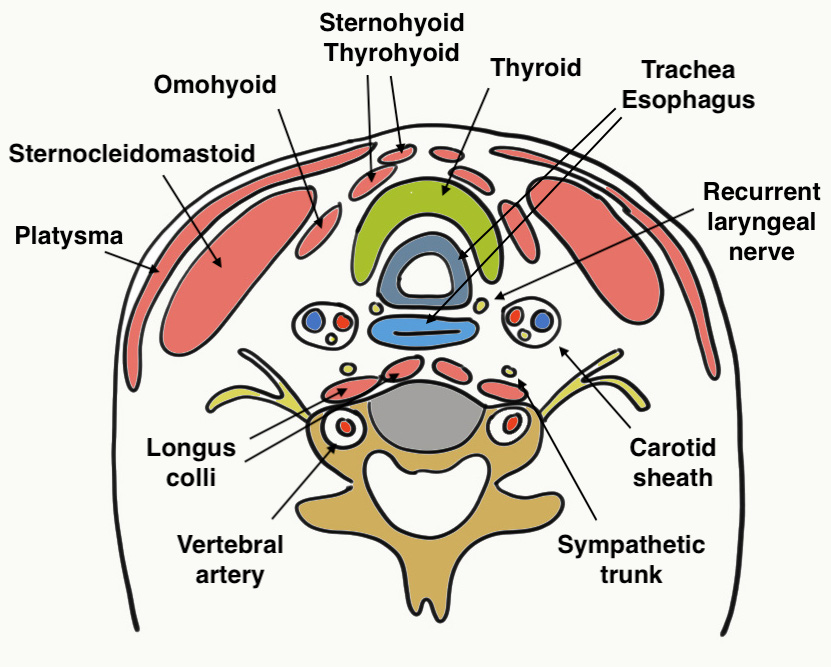
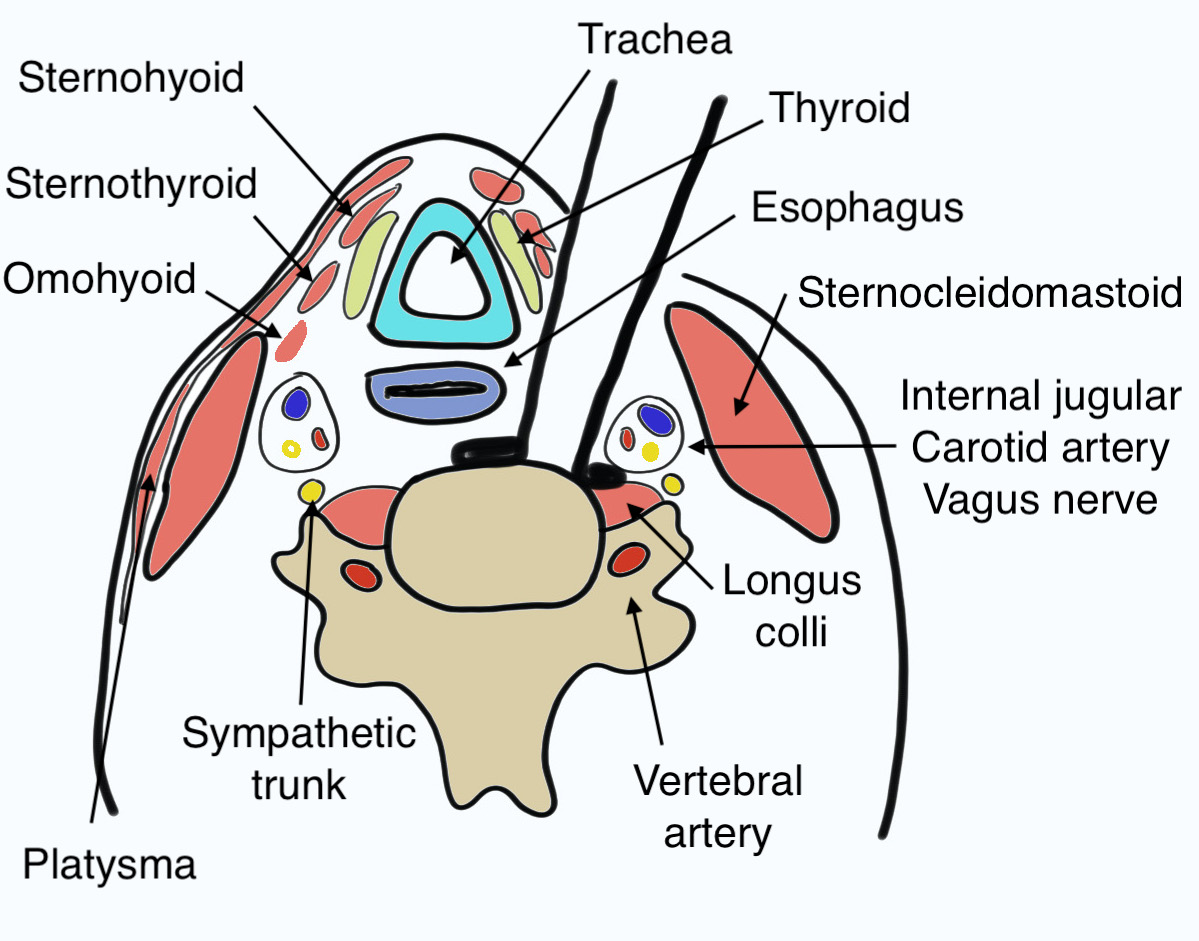
3 Fascial layers
1. Deep cervical fascia
- under the subcutaneous fat
- invests neck like collar
- clavicle / sternum / spine scapula - mandible / base of skull
- invests sternocleidomastoid (SCM) & trapezius
- have to incise so can retract SCM
- platysma and external jugular vein superficial to deep cervical fascia
2. Pretracheal fascia
- anterior neck only
- covers thyroid / tracheal / oesophagus
- deep to the strap muscles
- extends from hyoid into chest
- fuses laterally with carotid sheath
- have to divide to retract carotid sheath laterally
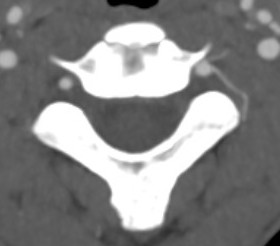
3. Prevertebral fascia
- base of skull to T3
- invests longus colli and sympathetics
- covers ALL
- divide to separate longus colli muscles to approach vertebral bodies and discs
Technique
AO Surgery Reference Anterior Approach Subaxial Spine
Transverse incision
- midline to medial border of SCM
Divide platysma
Incise deep cervical fascia
- just anterior to anterior border of SCM
- retract SCM laterally
- retract strap muscles (sternohyoid / sternothyroid) medially with trachea and oesophagus
Palpate and identify carotid sheath and divide pretracheal fascia medially
- retract carotid sheath laterally with SCM
- occasionally have to ligate superior thyroid artery
Expose Longus colli muscles anteriorly over ALL
- sympathetic chain lies on the Longus colli, just lateral to the vertebrae
- dissect between muscles in the midline
- retractors under longus colli
- expose cervical vertebrae
Confirm level with fluoroscopy
Which Side?
Most surgeons approach from the left
- the course of the Recurrent laryngeal nerve (RLN) is more predictable on left
Right sided approach
- used sometimes for C7/T1 to avoid thoracic duct
Structures at Risk
Vertebral artery
Esophagus
Superficial laryngeal nerve
Recurrent laryngeal nerve
Cervical sympathetic trunk
Vertebral artery
Anatomy
Origin from subclavian arteries
- anterior to C7 transverse process
- enter at C6 and travel in transverse foramina
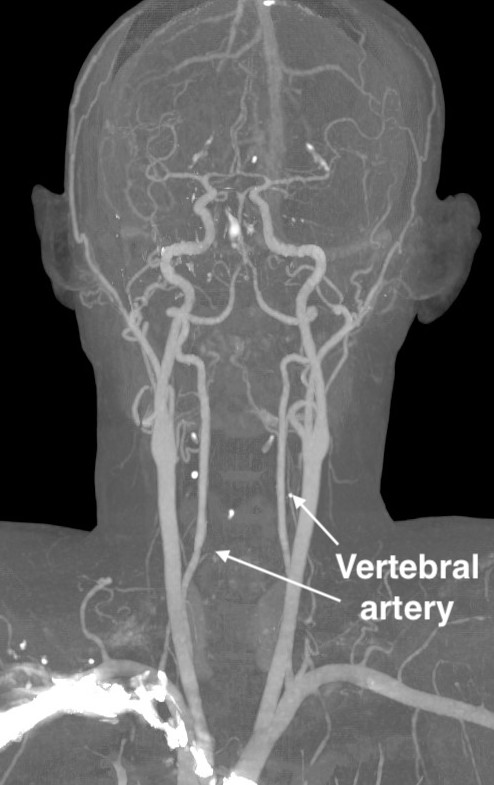

Consequence of injury
Stroke / neurological deficit
Hemorrhage
Pseudoaneurysm and late hemorrhage
Incidence
Obermuller et al Acta Neruochirurgica 2015
- 992 cases
- 0.3% incidence vertebral artery injury
- all three cases stented and repaired
- no neurological deficit
Protection
Stay medial to uncovertebral joints
Management
Control hemorrhage
Vascular surgery
Repair +/- stent
Esophagus
Dysphagia
Symptoms range from difficulty swallowing to aspiration
- systematic review of 73 ACDF studies
- overall dysphagia rate 19%
- associated with prolonged surgery / multilevel surgery / revision surgery / female sex
- reduced with use of zero profile plates
- 310 ACDF patients followed for 2 years
- incidence at 1 month 54%
- incidence at 1 year 15%
- incidence at 2 years 14%
Perforation
Zhong et al J Clin Neurosci 2013
- incidence 5/1097 (0.5%)
Halani et al J Neurosurg Spine 2016
- systematic review of 165 patients sustaining esophageal perforation
- most in trauma setting
- caused by hardware failure or erosion most commonly, direct injury less common
- presented with dysphagia / fever / neck swelling / wound leakage
- diagnosed with contrast studies / CT / MRI
- treated by primary repair or modified muscle flap
- mortality 6/153 (3%) - pneumonitis / mediastinitis / sepsis
Recurrent Laryngeal Nerve
Consequence of injury
Ipsilateral paralysis of the vocal cord
Hoarseness
Anatomy
Left side
- arises at the level of the aortic arch
- ascends between trachea and esophagus
- doesn't slope across the wound
Right side
- given off the vagus at the level of the subclavian artery
- slopes from lateral to medial across lower part of wound to reach the oesophagus / trachea interval
- crosses the surgical approach in 50% of cases
- usually at C6/7 with inferior thyroid artery
- may be at C5/6
Incidence
Kilburg et al J Neurosurg Spine 2006
- 8/278 (1.9%) had RLN injury with right sided approach
- 3/140 (2.1%) had RLN injury with left sided approach
Risk factors
Erwood et al J Neurosurg Spine 2016
- meta-analysis of incidence of RLN injury after revision surgery
- 14%
- reduced injury to RLN with reduced endotracheal cuff pressure
Superior Laryngeal Nerve
Consequence of injury
Dysphagia
Hoarseness
Anatomy
Superior laryngeal nerve runs with superior thyroid artery at C3/4
Cervical sympathetic trunk
Anatomy
Runs on the longus colli muscles
Consequence of injury
Horner syndrome
- ipsilateral ptosis
- ipsilateral meiosis
- anhidrosis
Incidence
Lubelski et al World Neurosurg 2020
- systematic review of 21 studies
- incidence of 0.6%
- 60% completely resolved at 1 year
