Conditions
Atlanto-axial subluxation (AAS) - ADI > 3 mm
Vertical subluxation (VS) / Basilar Invagination - Ranawat < 13 mm
Subaxial subluxation (SAS) - irreducible translation > 2 mm



Atlanto-axial subluxation Vertical subluxation Subaxial subluxation
Epidemiology
AAS 65%
VS 15 - 20%
SAS 20 - 25%
Symptoms
Neck pain
Occipital headaches - compression of occipital nerves
Neck / mastoid / ear / facial pain - compression of C2 nerve root
Instability symptoms
Brainstem compression symptoms - tinnitus, vertigo, visual disturbance, diplopia
Myelopathy
Acute spinal cord injury
Associations
Seropositive disease
Severe long standing disease
Natural History
- 140 patients with RA initially without cervical spine involvement
- followed for 5 years
- 44% developed cervical instability
- severe instability in 13%
- AAS in 32.1%
- VS in 11.4%
- SAS in 16.4%
Natural History with Biologics
Neo-RACo study
- 10 year study using infliximab in early RA
- cervical spine involvement only 4.7%
Lebouille-Veldman et al J Neurosurg Spine 2023
- 10 year follow up of 272 patients in BeST trial (optimal treatment including biologics)
- AAS 24%, VS 0%, SAS 22%
- 40% of patients develop at least mild cervical spine deformity
Screening
Cervical spine flexion / extension xray mandatory in all patients pre-operatively
Atlanto - Axial subluxation (AAI / AAS)
Aetiology
A. Attrition of transverse ligament
B. Erosion of peg
Epidemiology
Most common of RA cervical deformities - occurs in up to 50% of patients
May cause myelopathy symptoms - www.boneschool.com/myelopathy
Xray
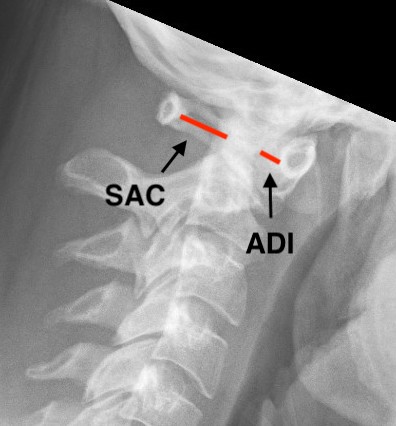
Atlanto-dens interval (ADI)
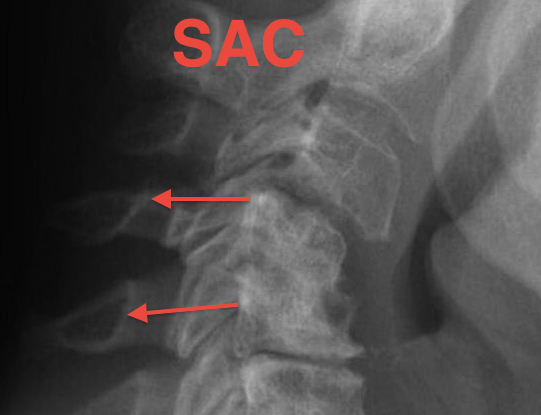
Space available for Cord (SAC) / posterior atlanto-dens interval (PADI)
Diagnosis
1. AADI (anterior atlantodental interval) > 3 mm


2. Instabilty
A. Instability : > 3 mm difference in flexion / extension views
B. Severe instability: > 7 mm difference


Instability 3 mm


Severe instability
3. PADI (posterior atlantodental interval / SAC (space available for cord))
- > 14 mm 94% predictive no neural deficit
- < 14 mm 97% predictive neural compression
Management
Nonoperative management
- 40 patients with RA, myelopathy, and atlantoaxial fixed instability
- 19 treated with occipito-cervical fusion, 21 treated nonoperatively
- operative group: 68% neurological improvement, 37% 10 year survival
- nonoperative group: 100% bedridden in 3 years, 0% 8 year survival
Algorithm
1. PADI >14mm -> observe
2. PADI < 14mm MRI
3. Cervicomedullary angle <135° / SAC < 13 - fusion
Options
1. C1/2 fusion
- instability reducible
- no neurology / no decompression needed
2. Occipito-cervical fusion
- instability irreducible
- neurological symptoms
- decompression of lamina C1 required
C1/C2 fusion
AO Surgery Reference C1/C2 fusion
Options
1. Transarticular screws (Magerl)
2. C1 lateral mass / C2 pedicle screws (Goel-Harms)
+/- Brooks interlaminar wire with posterior bone graft


Gallie-Brooks fusion

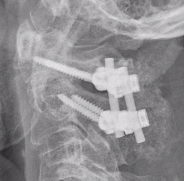
C1 lateral mass / C2 pedicle screws (Goel Harms)

Transarticular / Magerl screws from: Koepke et al Nature Reports
Results
Ryu et al World Neurosurg 2017
- 58 patients with RA and AAS
- treated with either transarticular screws or C1/C2 screws
- no difference in fusion rates / clinical outcomes / complications
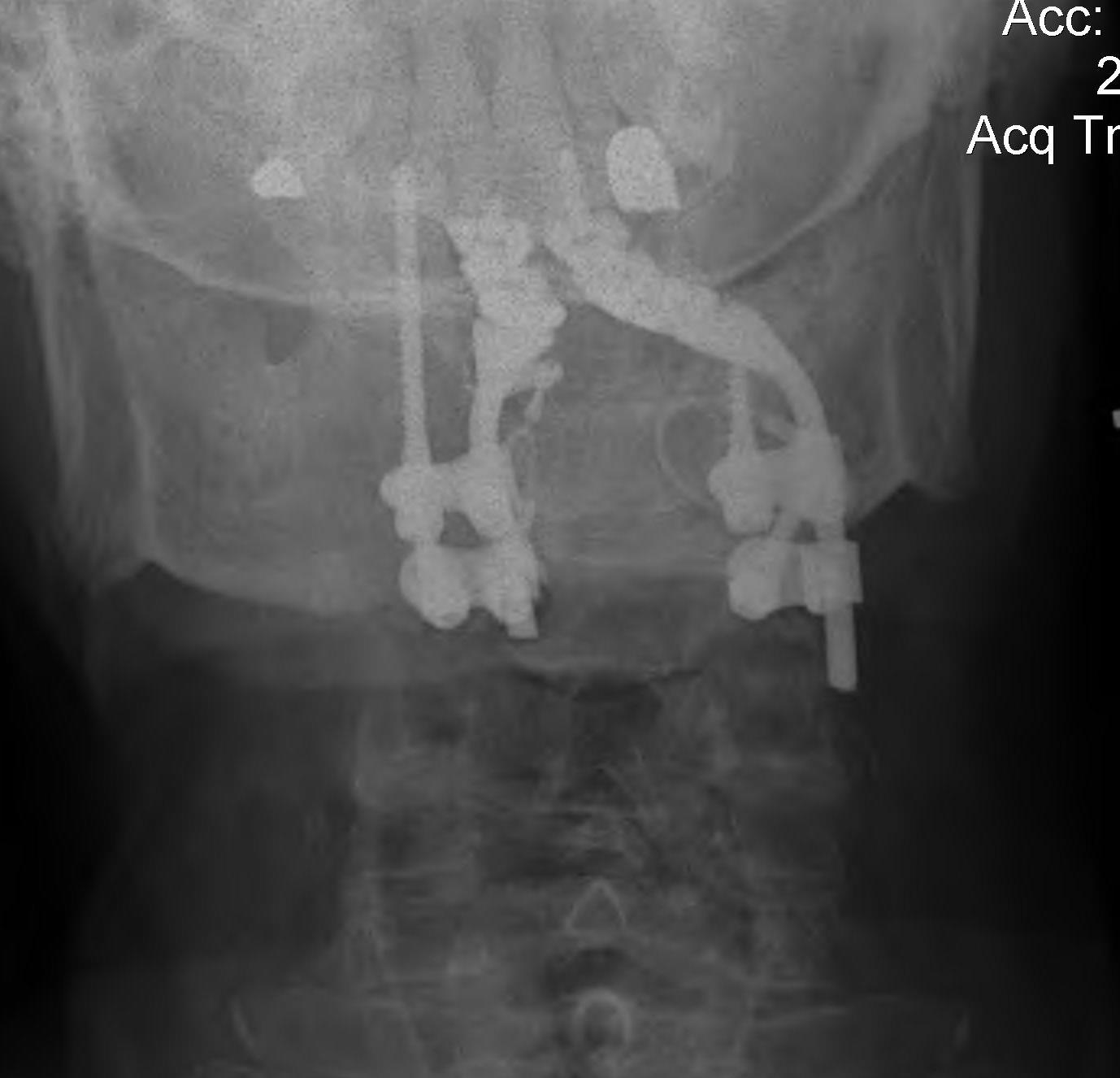
Occipito-cervical fusion

Basilar invagination / Vertical subluxation

Definition
Superior migration of the odontoid into foramen magnum
Pathology
Due to erosion of lateral masses of atlas and occipital condyles
- can lead to compression of brain stem
- risk of myelopathy / sudden death
- associated with severe peripheral disease
Diagnosis
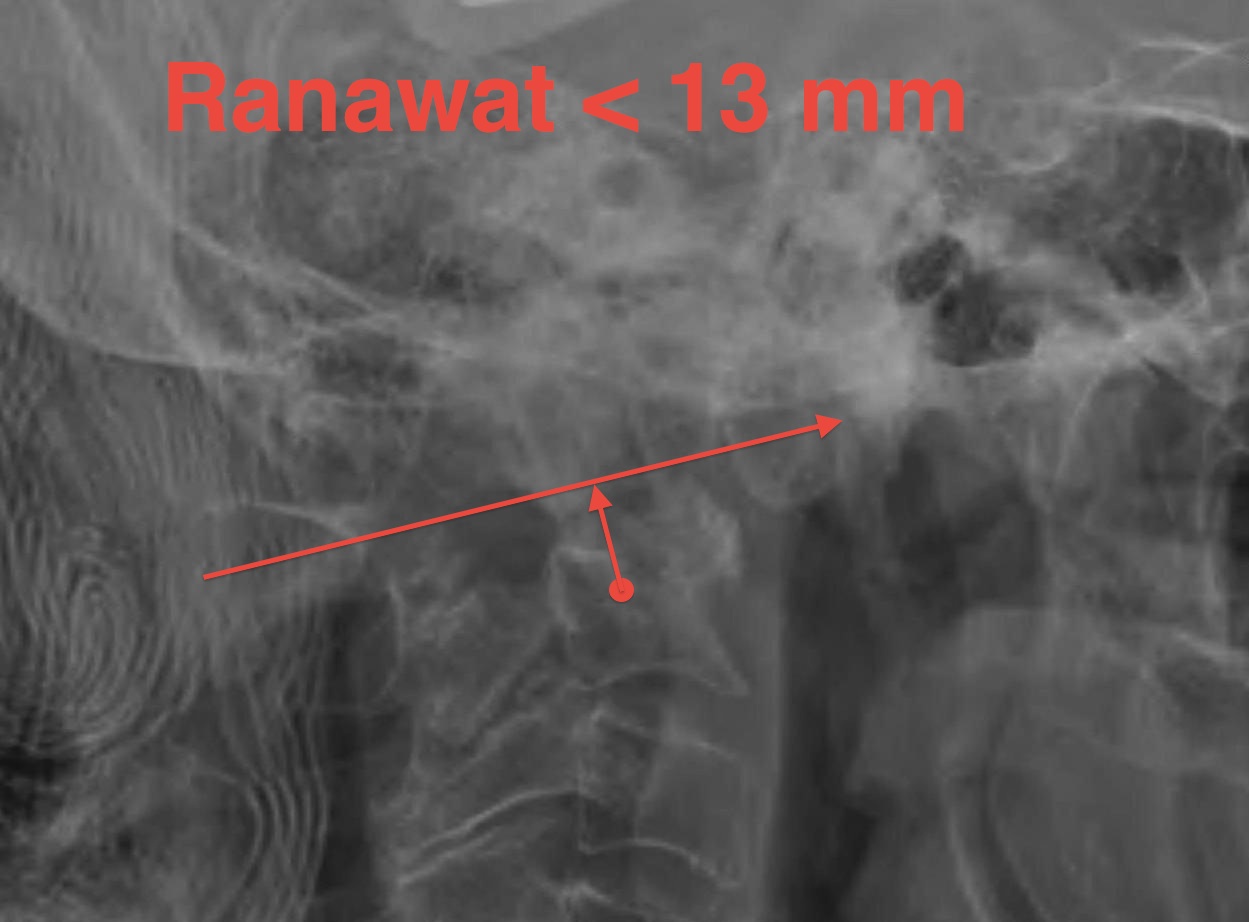
Ranawat measurement < 13 mm
- line between anterior and posterior arch C1
- centre of pedicle of C2

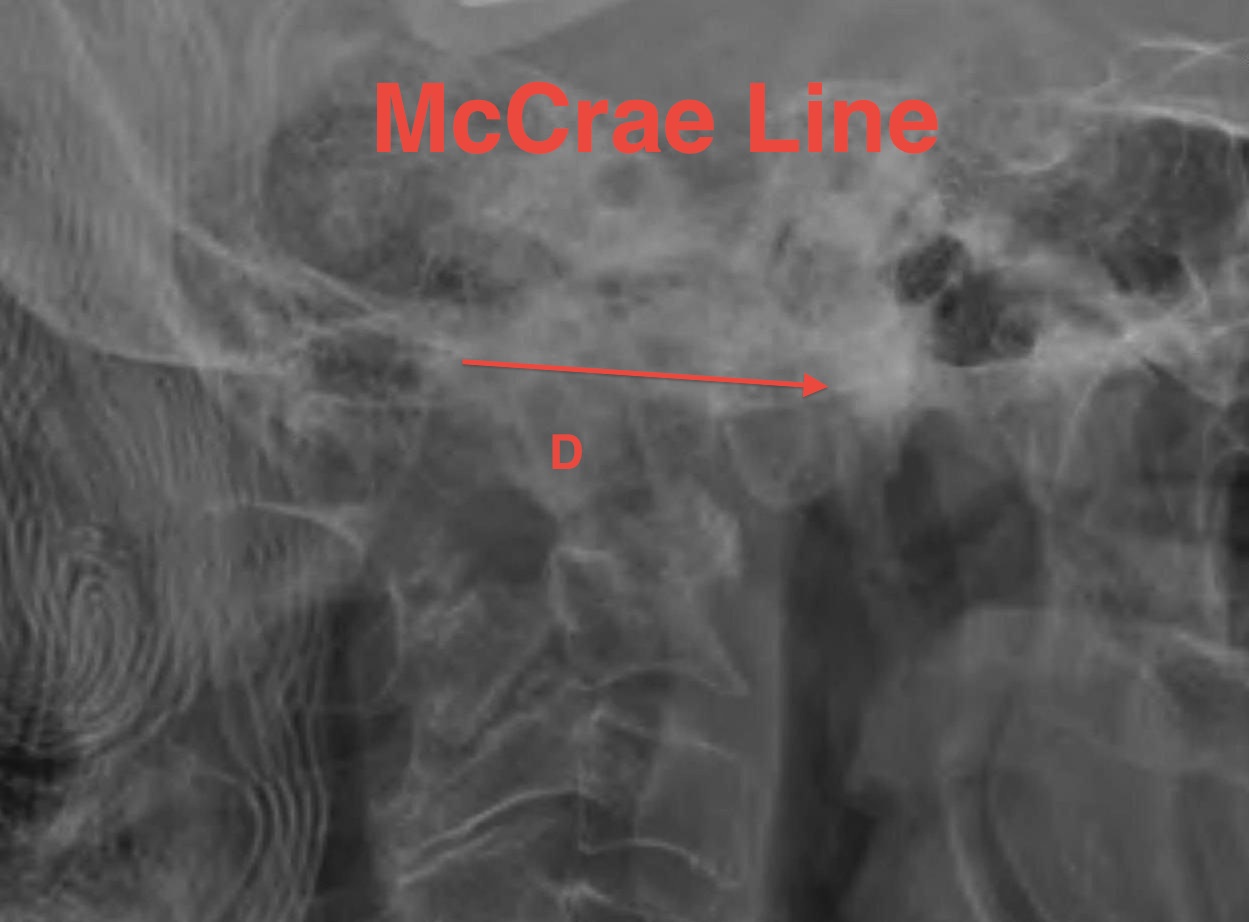
McCrae
- line of foramen magnum
- tip of odontoid should not protrude above this line

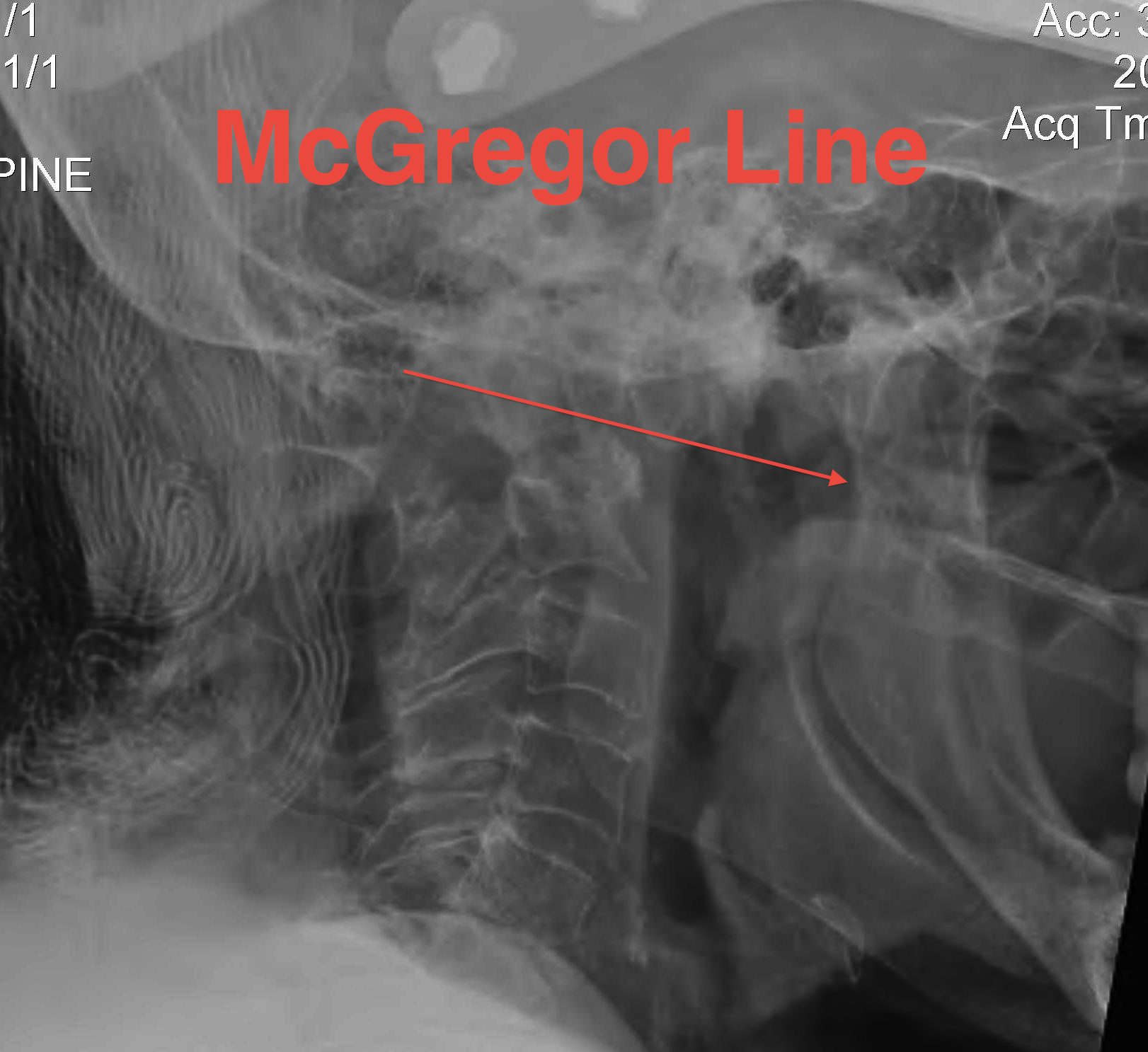
McGregor line > 4.5 mm
- line hard palate to posterior occiput
- if tip of dens > 4.5 mm above this line = vertical settling
- severe > 8 men or > 10 women
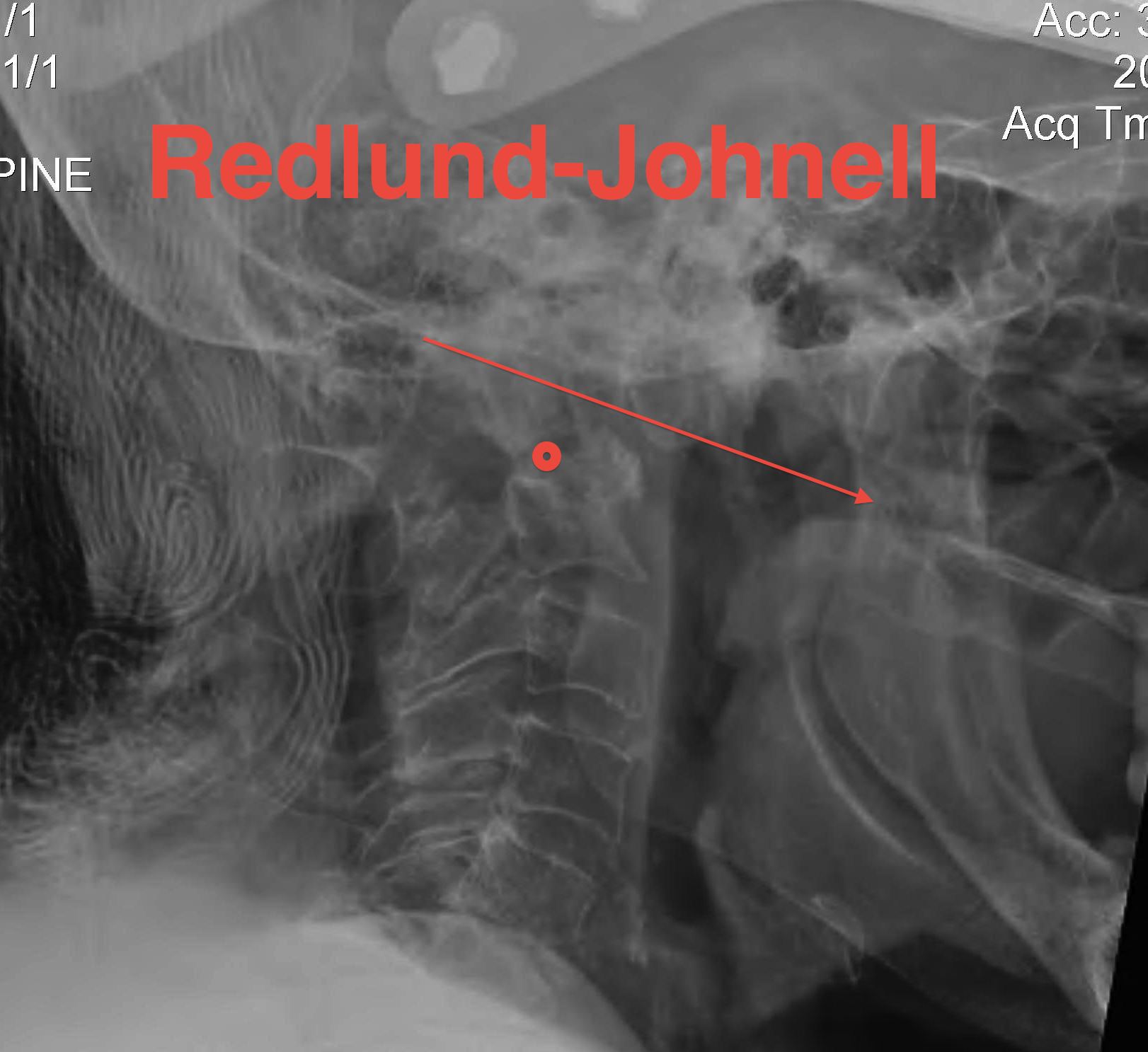
Redlund-Johnell measurement
- assesses entire occiput to C2 complex
- base of dens to McGregor line
- men < 34mm / women <29 mm = abnormal
CT

Coronal and sagittal CT of basilar invagination
MRI
Cervico-medullary angle < 135 degrees
- the line parallel to ventral side of medulla oblongata
- the line parallel to the ventral side of the upper cervical cord
- normal angle is 135-175°
- <135° consistent with vertical settling and correlated with myelopathy
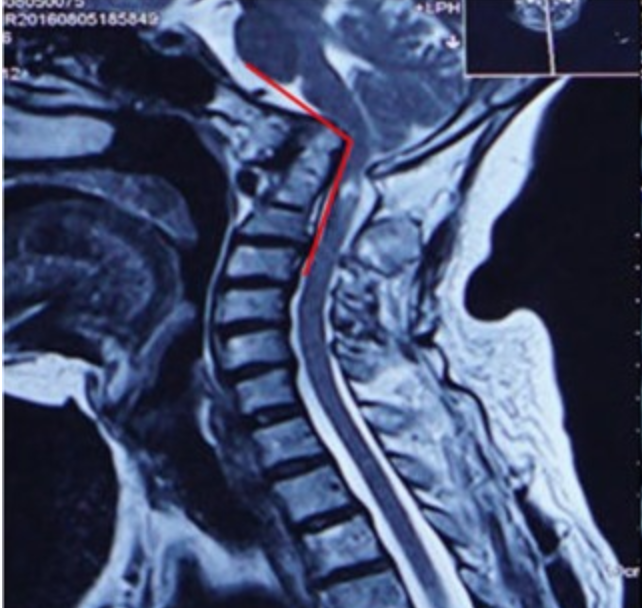
From: Guo et al Sci Rep 2019. http://creativecommons.org/licenses/by/4.0/.
Management
Algorithm
1. No symptoms & no cord compression on MRI - observe
2. Cord compression
- occiput to C2 fusion
- +/- C1 laminectomy
- +/- odontoidectomy

Results
Dasenbrock et al Neurosurgery 2012
- 15 patients with RA and basilar invagination
- posterior stabilization and endoscopic odontoidectomy
- myelopathy improved in all patients
McDowall et al J Craniovert Junction Spine 2021
- Swedish registry
- review of 176 patients with RA undergoing cervical stabilizaton
- 48 (27%) with basilar invagination
- improvement in pain
- early improvement in neurology, returning to baseline at 5 years
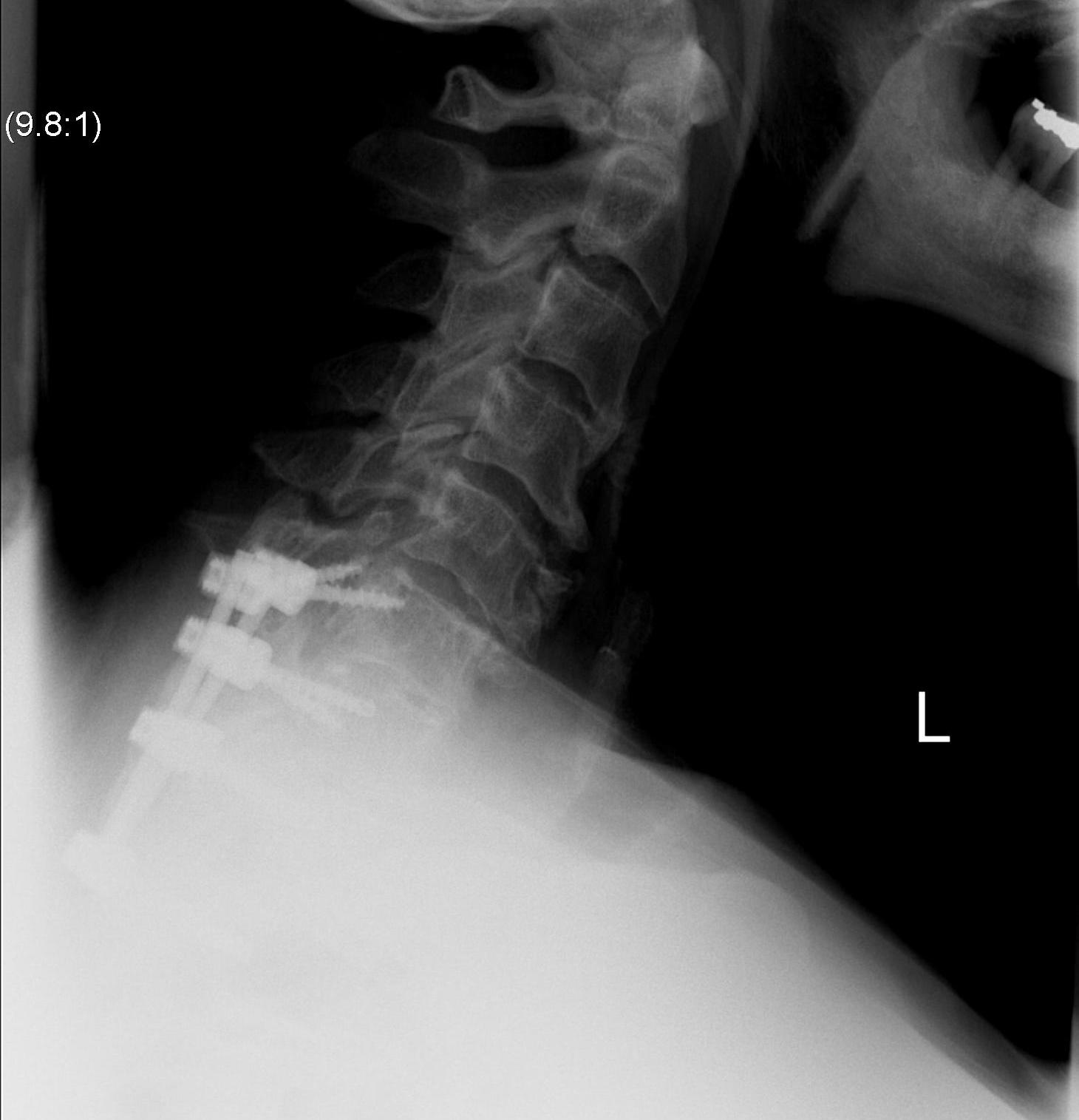
Subaxial Subluxation (SAS)
Definition
Anterior subluxation of one vertebral body on another
Results in spinal stenosis
Diagnosis
A. Instability on Flexion / Extension views
- > 3mm
- > 11o


Anterior subluxation of C3 on C4
B. Space available for cord / SAC
- subaxial canal diameter on lateral
- < 13 mm high incidence neurology
Pathology
Facet erosions / ligament incompetence
May see at multiple levels with stepladder type deformity & kyphosis
Can occur beneath previous cervical fusions including C1/C2
MRI

Management
Indications for surgery
- SAC < 13 mm
- stenosis symptoms
- instability
Options
ACDF
Posterior laminectomy and fusion
Anterior decompression and fusion

Posterior laminectomy and fusion
May need long fusion to prevent SAS above and below

Results
McDowall et al J Craniovert Junction Spine 2021
- Swedish registry
- review of 176 patients with RA undergoing cervical stabilizaton
- 19 (11%) with SAS
- improvement in pain
- highest risk of death within 5 years after surgery (11/19, 58%).
