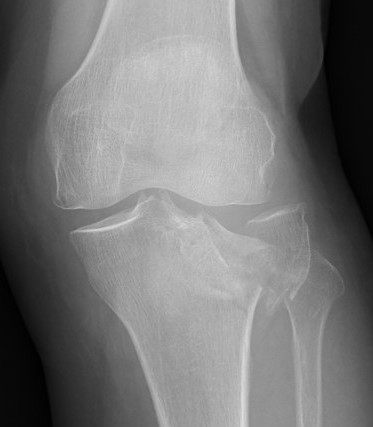
Schatzker Classification
I. Lateral Spilt
- seen in young patient
- lateral meniscus can be incarcerated in fracture
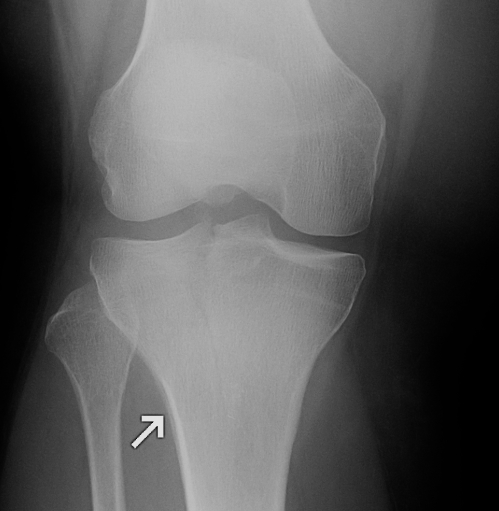


II. Lateral Split Depression
- often seen in young patients with high energy injuries
- vary in severity
III. Lateral Depression
- central depression usually seen in elderly
- have to create lateral cortical window in order to elevate fragment


IV. Medial plateau & intercondylar eminence
- high velocity injury associated with ACL / LCL / CPN injury
- can be low injury / osteoporotic and often unreconstructable


V. Bi-condylar + intact metaphysis
- unstable
- requires ORIF

![]()
VI. Bi-condylar + metaphyseal fracture
- fracture separating metaphysis from diaphysis
- highest incidence of vascular injury


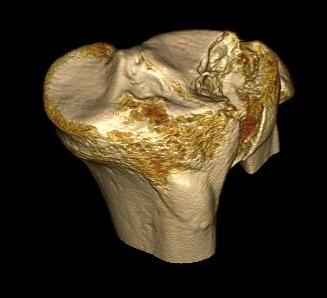
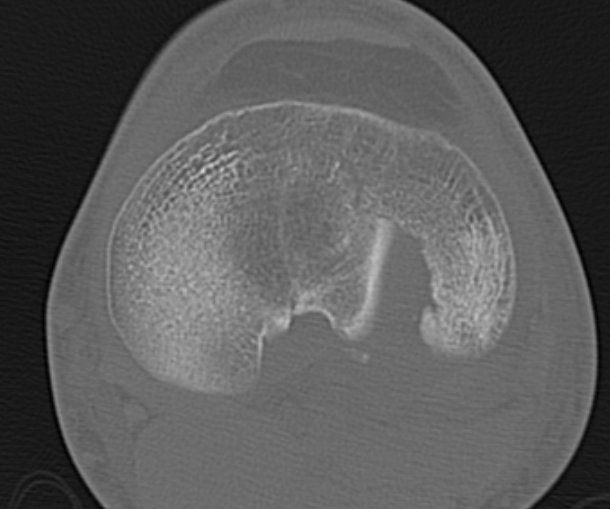
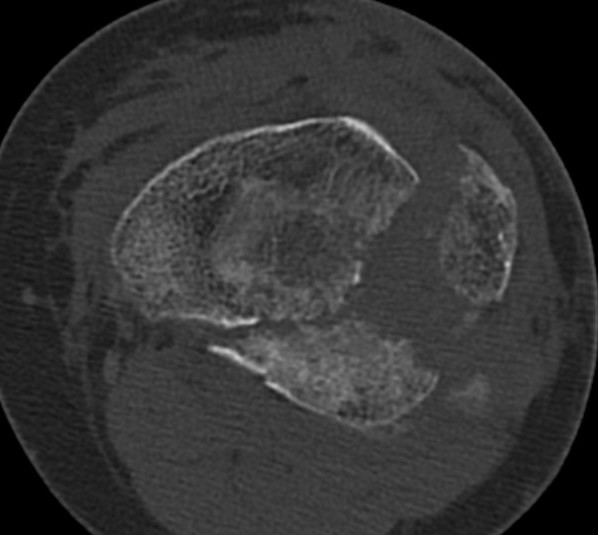
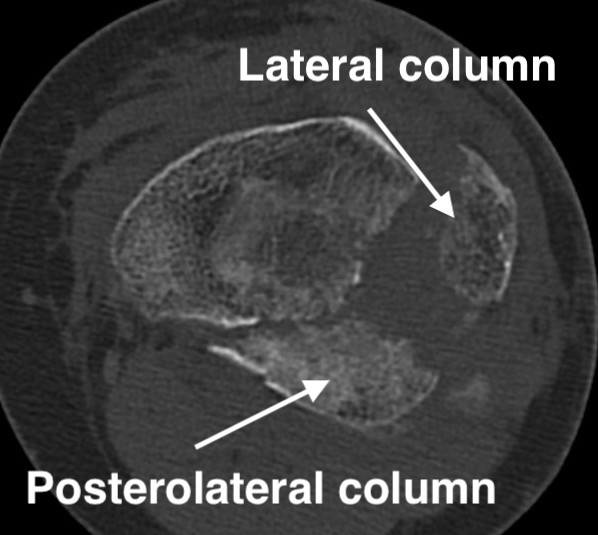
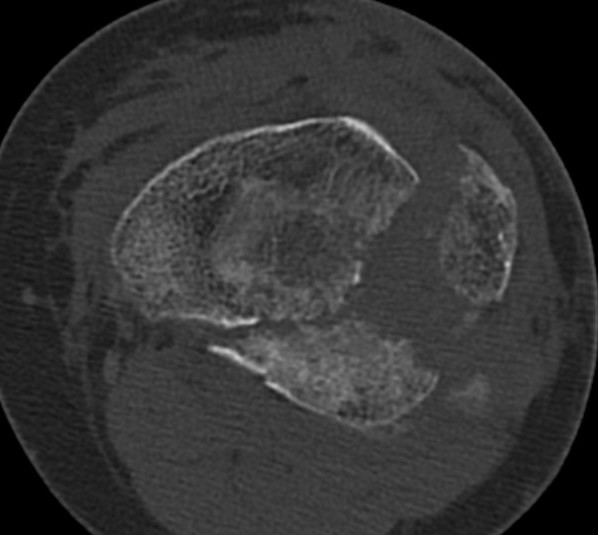
3 column concept of tibial plateau fractures
Luo et al. Orthop Trauma 2010
- introduces the 3 column concept
- medial column / lateral column / posterior column
- posterior column can be splint into medial and lateral fragments (posterolateral / posteromedial)
- imporant as any surgery must address these fragments
- typically require additional posteromedial or posterolateral approaches
https://pubmed.ncbi.nlm.nih.gov/20881634/
Epidemiology
Most common is Type II split depression
- 80%
Type IV medial condyle
- 10 - 20%
Type V, VI bicondylar
- 10 - 20%
Age
- young people splits / wedges
- older people joint depression
Anatomy
Medial plateau larger than lateral
- medial is concave in sagittal plane (golf tee)
- lateral is convex & more proximal (golf ball)
Creates 3o of varus proximal tibia
- important to be created in any reconstructive tibial plateau surgery
Normal posterior slope
- 10o

Lateral plateau is covered by meniscus
- tolerates incongruity better than medial plateau
Pathology
Lateral plateau more commonly fractures
- medial plateau more resistant to fracture
- due to its larger surface and increased weight bearing
- thicker stronger subchondral bone
- any fracture of medial plateau indicates high energy
- high incidence of soft tissue complications & poor outcomes
Associated Injures
Meniscal injury
Stahl et al. J Orthop Trauma 2015
- 602 patients
- 30% had a lateral meniscus tear requiring intervention
- 45% in split depression Type II
https://pubmed.ncbi.nlm.nih.gov/25635356/
Ligament injury
Gardner et al. J Orthop Trauma 2005
- MRI of 103 patients with tibial plateau booked for surgery
- 57% complete tear of ACL
- 28% complete tear of PCL
- 29% complete tear of LCL
- 32% complete tear of MCL
https://pubmed.ncbi.nlm.nih.gov/15677922/
Tomas-Hernandez et al. Injury 2016
- case series of patients with anteromedial tibial plateua fractures
- these patients have posterolateral corner ligament injuries
https://pubmed.ncbi.nlm.nih.gov/27692105/
Compartment syndrome
Increased incidence in high energy injuries
- Type V and VI bicondylar fractures
- Type IV medial fracture dislcations
Gamulin et al. BMC Musculoskeletal Disorders 2017
- 28/265 (10%) tibial plateua fractures had compartment syndrome
- more common in higher grade tibial plateau fractures
- more comon in young patients
https://pubmed.ncbi.nlm.nih.gov/28720096/
Popliteal artery damage
CPN
Factors affecting outcome
1. Severity of intial injury
2. Residual Articular step
3. Alignment
4. Meniscus
5. Instability
Blokker et al. CORR 1984
- >5 mm step 0% good or excellent results
- <5 mm 75% good or excellent results
- < 2 mm 85% good or excellent results
https://pubmed.ncbi.nlm.nih.gov/6546361/
Biz et al. Orthop Surg 2019
- worse outcomes with more severe injuries
- daily pain associated with residual articular step and malalignment
https://pubmed.ncbi.nlm.nih.gov/31755217/
Honkonen et al. J Orthop Trauma 1995
- meniscectomy during ORIF resulted in 74% osteoarthritis
- if meniscus intact or repaired, 37% osteoarthritis
https://pubmed.ncbi.nlm.nih.gov/7562147/
Management
Examination
NV examination
Soft tissue examination
- Tscherne / closed soft tissue injury classification
- Gustillo / open soft tissue injury classification
Exclude compartment syndrome
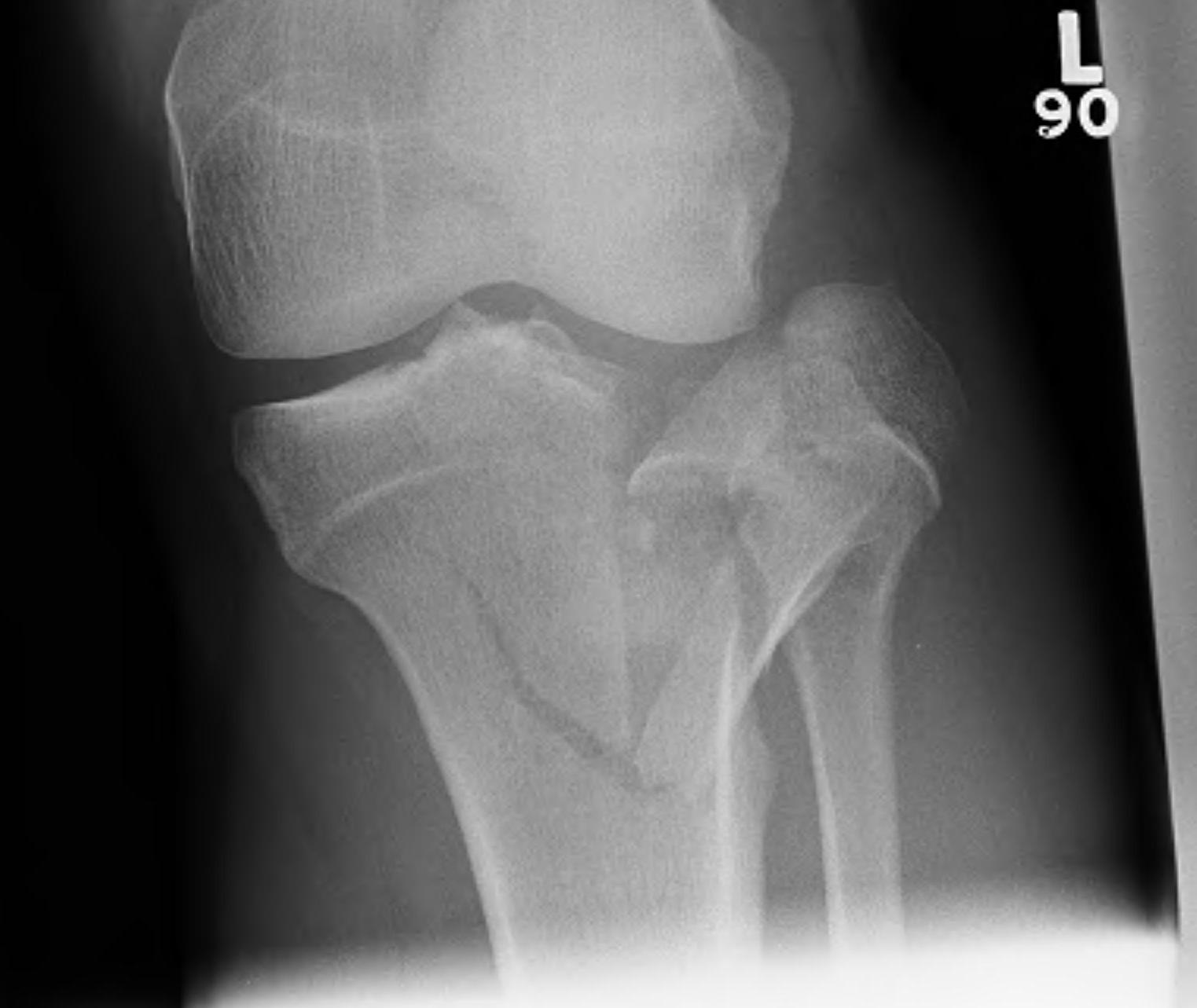
CT scan
Assess joint line
- predetermine fracture pattern before fixation
- will pick up medial condyle / bicondyle / metaphyseal fractures not seen on xray
Temporary Spanning External Fixation
Indications
- open fracture
- complex pattern / shortening / malalignment
- poor soft tissues / extreme swelling
Advantages
- pulls out to length with ligamentotaxis
- allows soft tissues to settle / swelling resolves
- subsequent surgery easier and safer
Construction
- 2 x 5 mm half pins anterior / anterolateral femur
- 2 x 5mm half pins anterior tibia far from incision
- apply under flouroscopy guidance / reduce / apply traction
- 2 x anterior rods
- slight flexion
AO Foundation Surgical Technique
Definitive Management
Indications for surgery
1. Step > 2mm
2. Malalignment
Type I
Percutaneous fixation
- beware trapped lateral meniscus
- consider arthroscopic inspection initially
- difficult to see because of haematoma
- also risk of compartment syndrome so need careful fluid management

Type II Split Depression

Timing
- blisters epithelialised
- skin wrinkled
- 2-3 weeks
Set up
- prone on radiolucent table
- knee flexed over bolster or triangle
- tourniquet, antibiotics
- remove frame, scrub leg and apply sterile dressings to pin sites to remove from operative field
- some surgeons leave frame on to aid reconstructive surgery
- may need to use femoral distractor
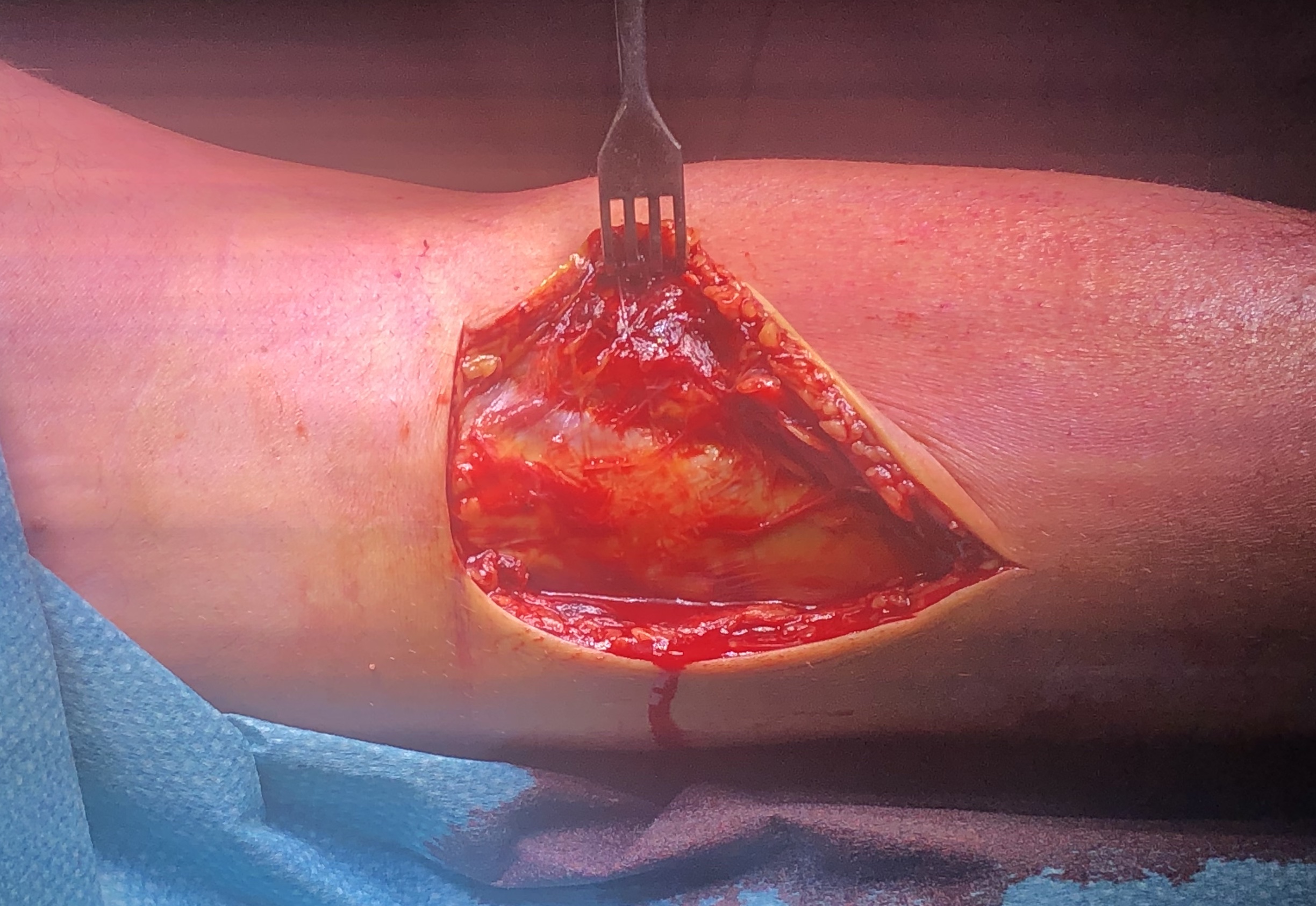
Approach
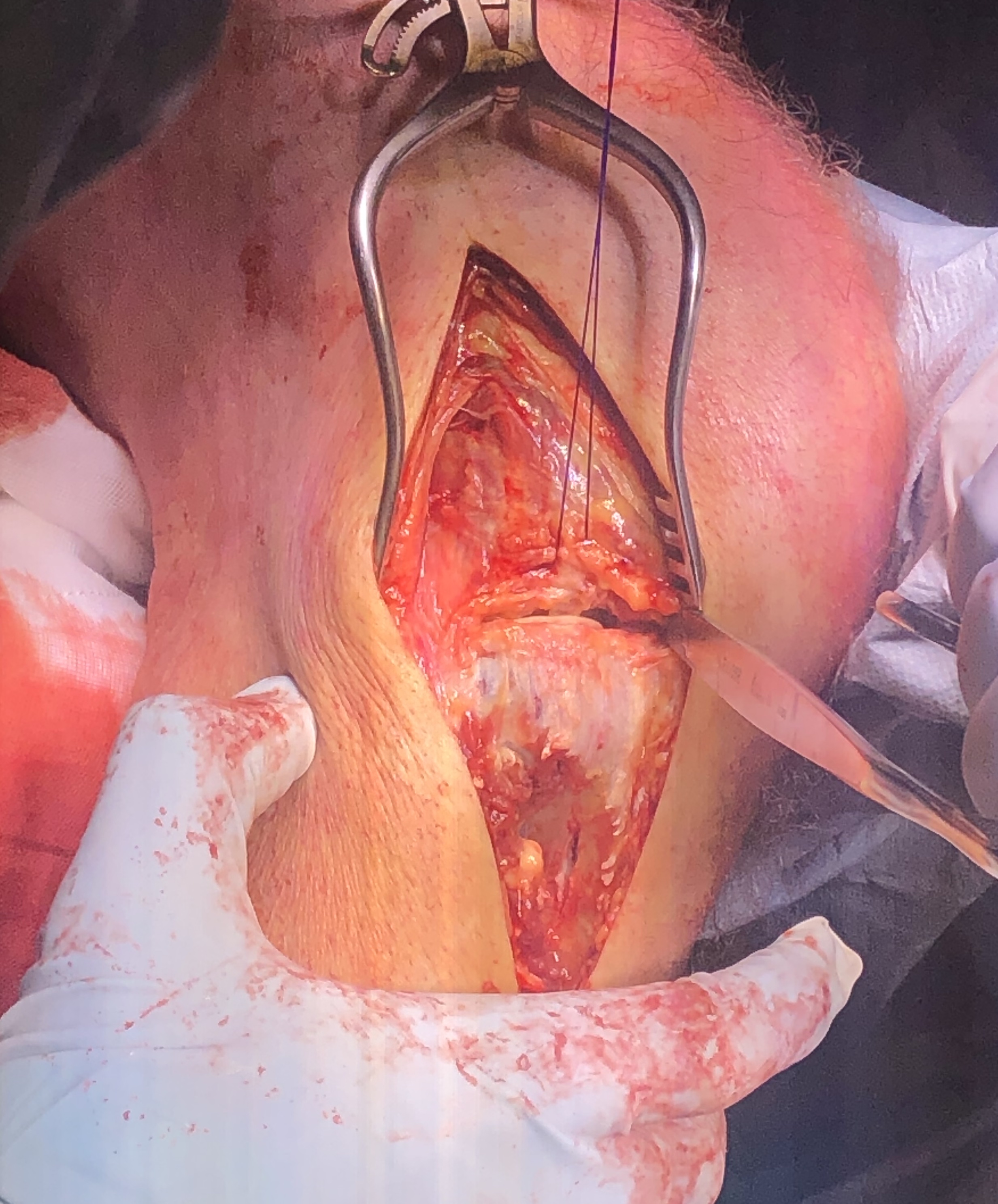
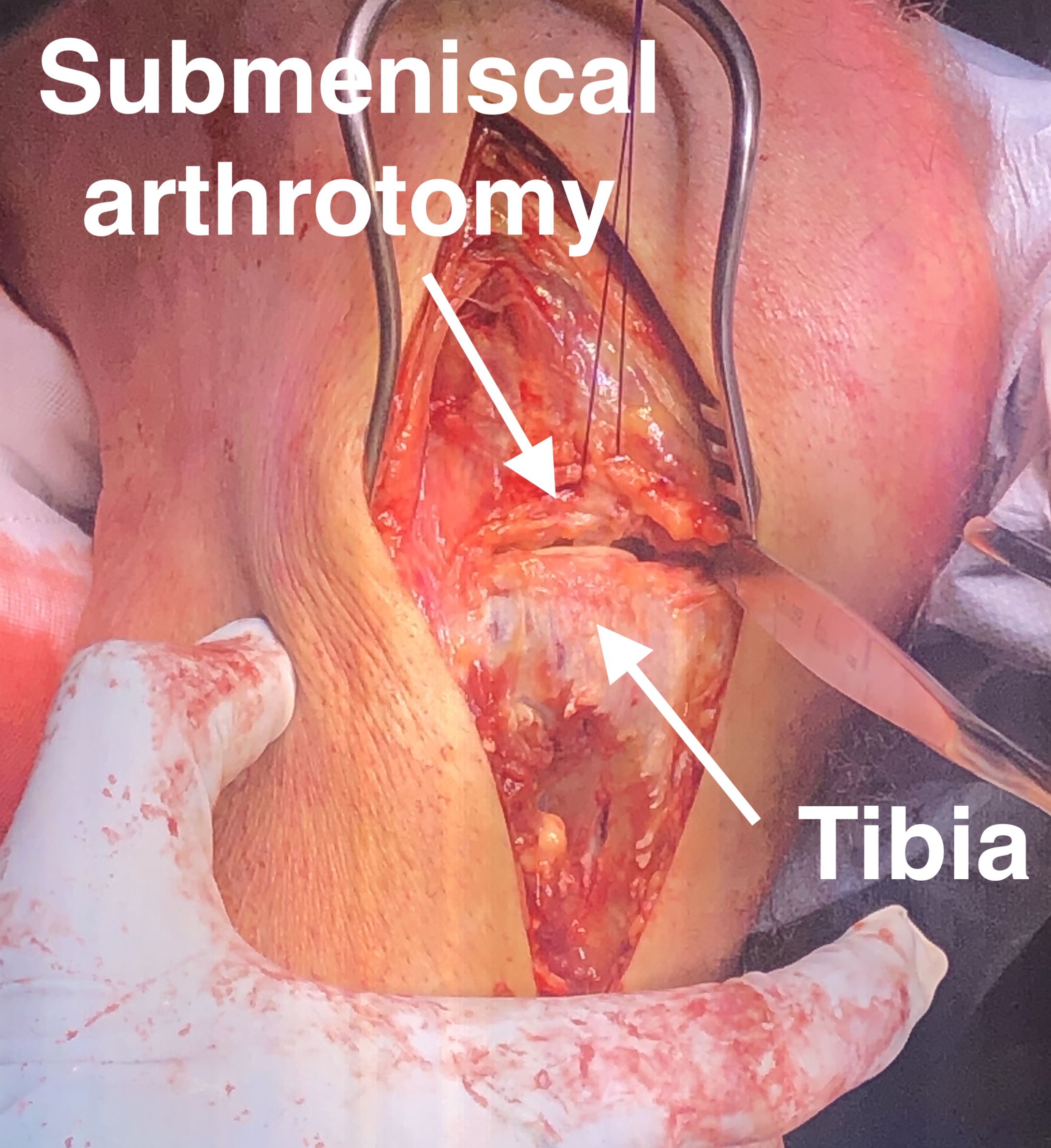
Anterolateral approach
- lateral longitudinal incision
- split ITB proximally
- open anterior fascia distally and elevate tibialis anterior from tibia
- perform submeniscal arthrotomy by incising capsule and coronary ligament from proximal tibia
- elevate capsule / ligament / and lateral meniscus via 1 vicryl stay sutures
- inspect joint and lateral meniscus via varus force
- can use femoral distractor
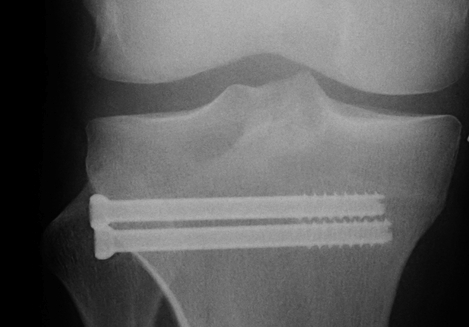
Technique
- elevate and restore joint line
- compress with bone reduction forcep
- stabilise joint line with 2 x 6.5 mm cannulated partially threaded screws
- check fluoroscopy
- restore alignment via application anatomically contoured 4.5 mm locking plate
- often use BG or substitutes under depression fractures laterally
Stability
- must assess at end of operation
Type III Depression




Technique
Anterolateral approach
- visualise joint line
- create cortical window
- elevate fracture
- support with bone graft (autograft / allograft / bone substitute)
Type IV Medial Condyle
Technique
Medial approach
- make incision 1 cm from posterior edge of tibia
- release and reflect MCL posteriorly
- partially release pes anserinus / reflect inferiorly
- T plate
- can slide under the pes

Type V Bicondylar
Options
1. Medial and Lateral plating
2. Circular Fixator
Canadian Orthopedic Trauma Society JBJS Am 2006
- RCT of ORIF (two plates) with circular external fixation in 83 knees
- comparable fracture reduction in both
- no difference in outcomes
- reduced blood loss / hospital stay / infection / reoperation with external fixation
- 7/40 (18%) of patients undergoing ORIF had an infection
https://pubmed.ncbi.nlm.nih.gov/17142411/
Zhao et al. Int J Surg 2017
- meta-analysis of external fixation v ORIF for complex tibial plateua fractures
- no difference in DVT/PE, outcomes, deep infection between two groups
- external fixation does have an overall higher rate of infections due to pin site infections
https://pubmed.ncbi.nlm.nih.gov/28089798/
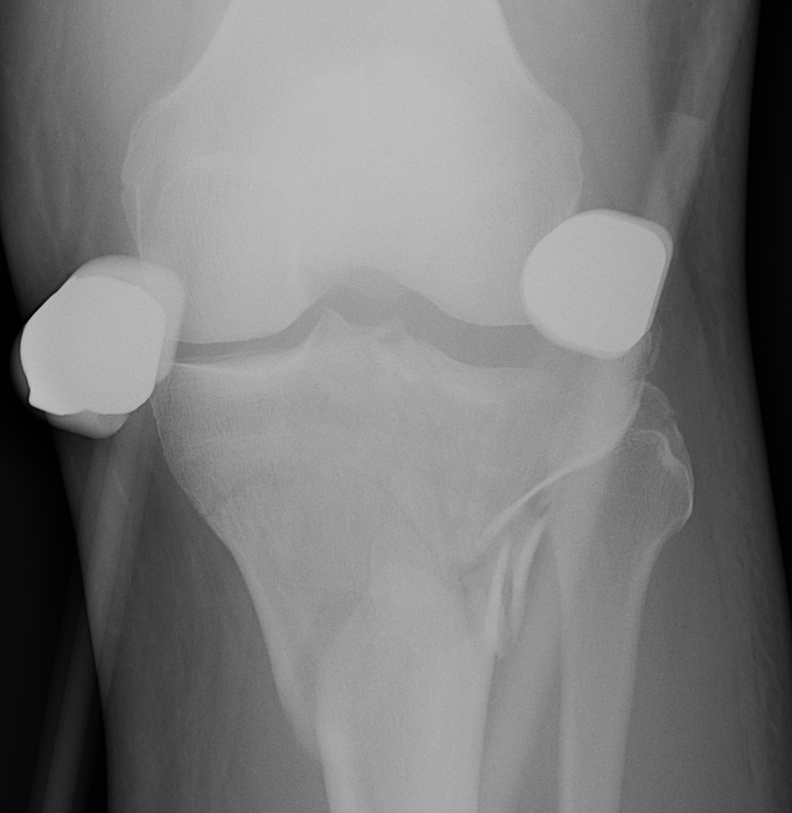
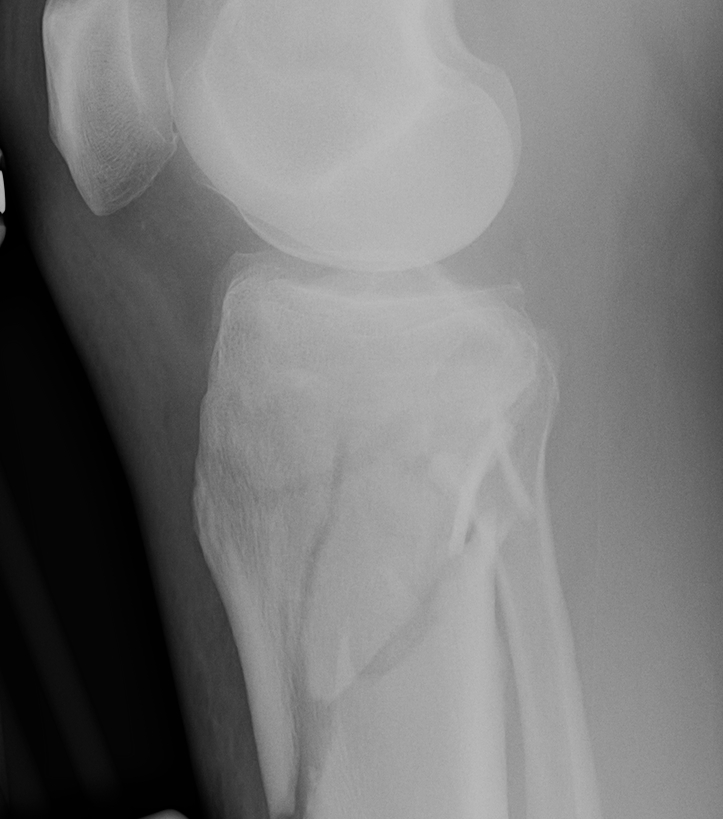
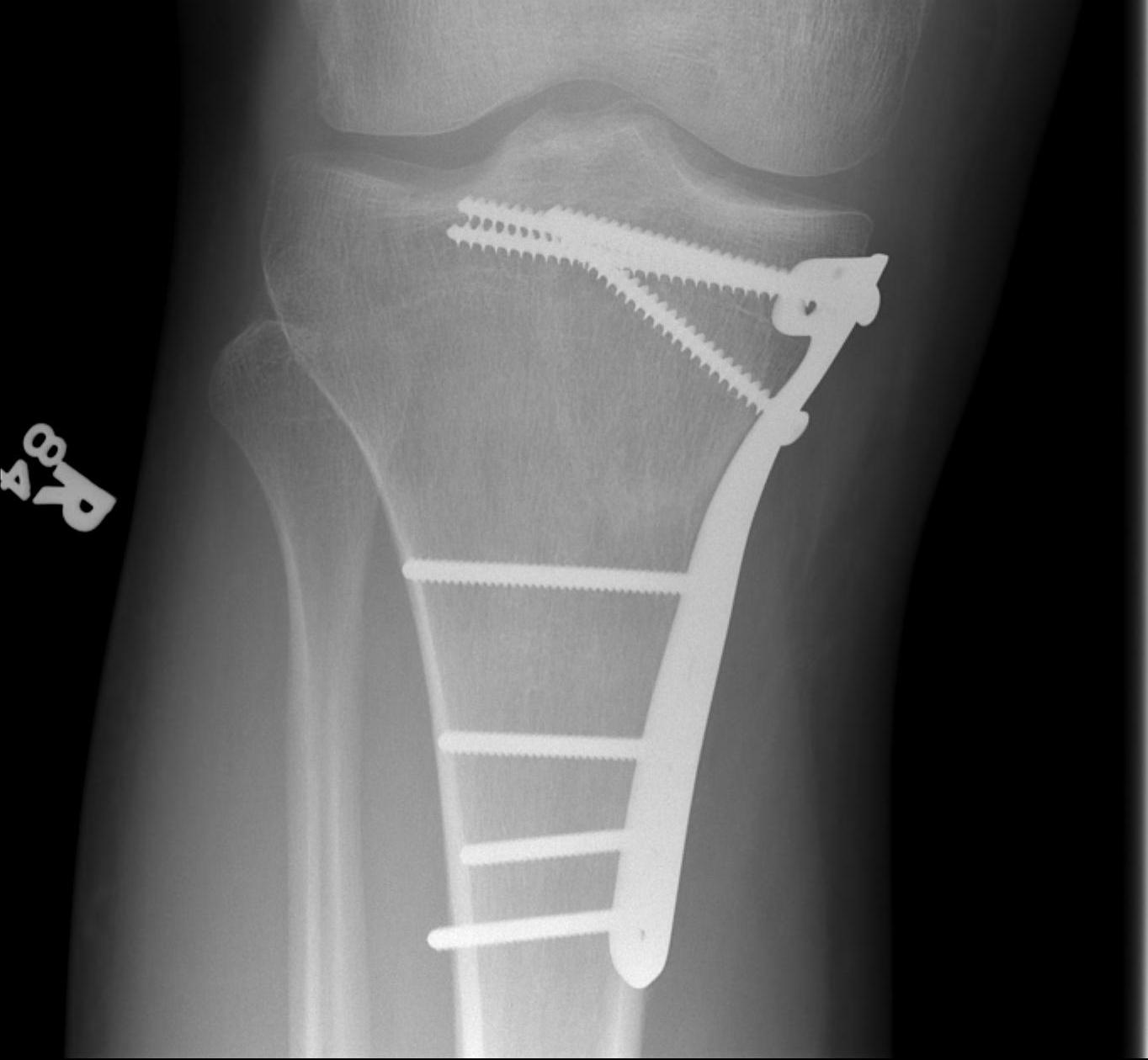
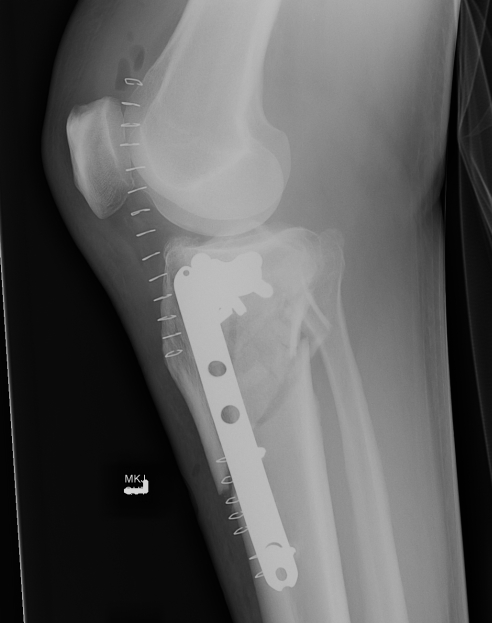
1. Medial and Lateral Plating
Technique
- depends on which of the three columns affected
- anterolateral approach for lateral column
- posteromedial appraoch for medial / posterior column
![]()
![]()
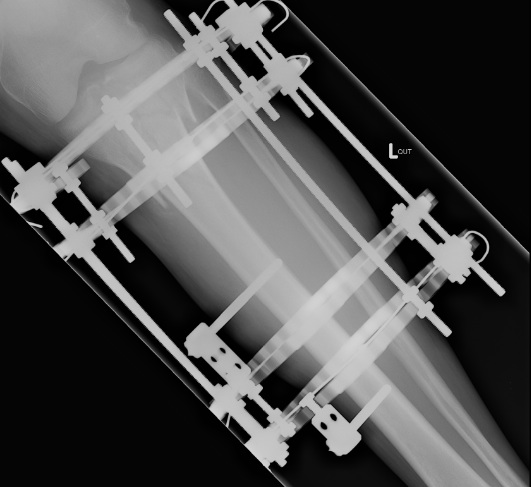
2. Circular external Fixation
Indications
- poor soft tissues
- compound wound
Technique
- hybrid fixation
- wire fixation proximally
- pin fixation distally
- use olive wires to compress fracture fragments
- place wires 14mm from joint surface to avoid placing intra-articular
Type VI Bicondylar with Metaphyseal Fracture
Technique
- long locking plate minimally invasive with locking jig / MIPO
- proximal lag screws
- ensure correct alignment
- often use small medial buttress plate



Posterolateral Tibial Plateau Fractures
Definition
- fracture in posterior half of lateral tibial plateau
- very difficult to access with standard anterolateral approach





Options
1. Trans-fibular neck osteotomy + anterolateral approach
2. Posterolateral approach + anterolateral approach
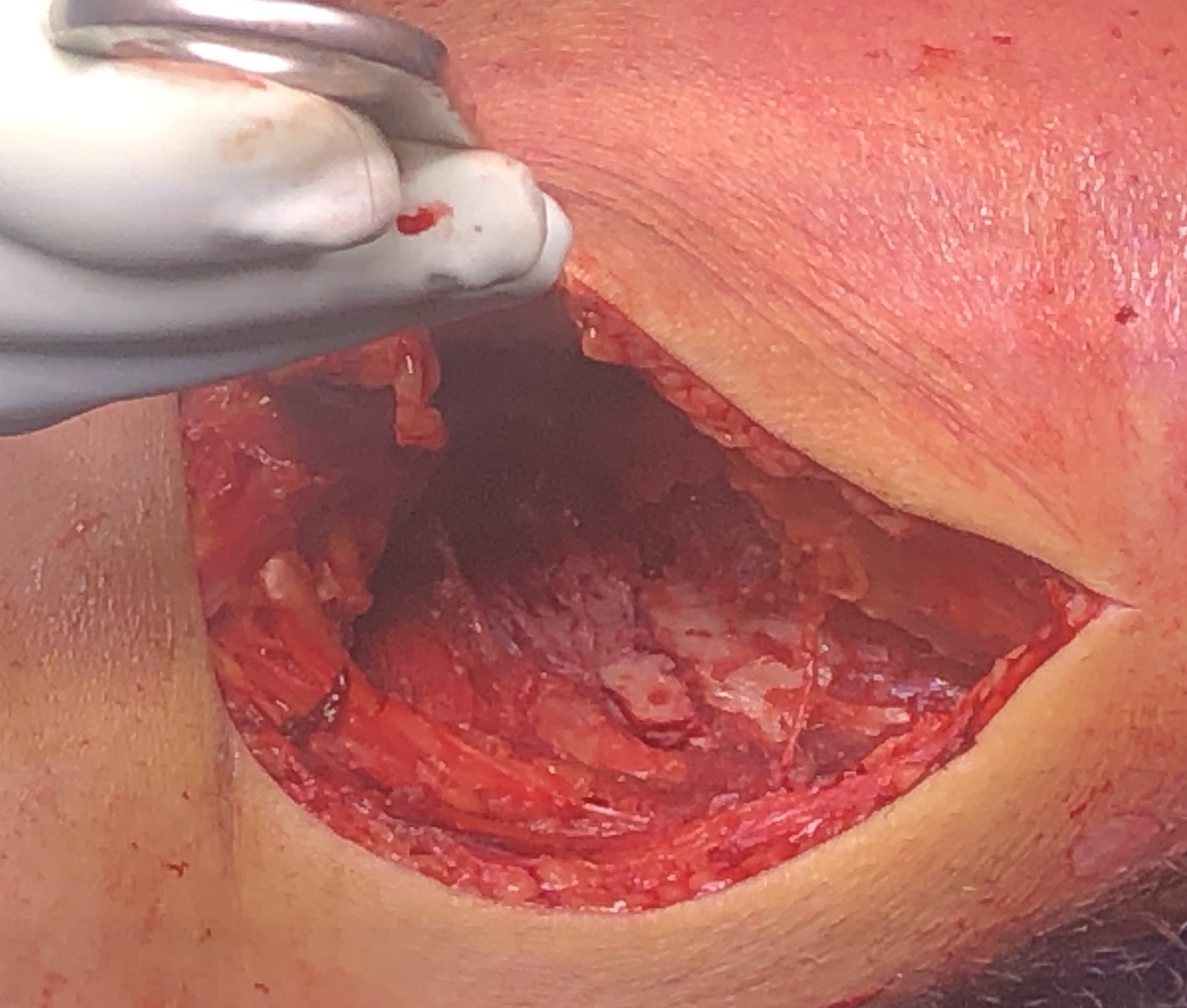
1. Transfibular osteotomy
- incision based on fibular
- divide ITB
- expose CPN under biceps femoris
- release CPN completely from fibular neck and protect
- maintain ligamentous attachments to fibular head
- predrill fibula for later intra-medullary screw
- chevron osteotomy at fibular neck
- reflect fibular head posteriorly and superiorly on biceps / LCL attachments
- place posterolateral buttress plate
- expose anterolateral tibia and place standard anterolateral plate as needed
- stabilize tibio-fibular joint with screws from fibular into tibia / fibular screw
Pires et al. Injury 2016 Article PDF
https://www.otcbrazil.com.br/wp-content/uploads/2017/10/Transfibular-Injury-publicado.pdf
2. Posterolateral approach
- single incision
- identify, release and protect the CPN
- posterolateral window is below CPN
- gastrocnemius posteriorly, tibia and popliteus anteriorly
- ligate inferior geniculate artery on the popliteus
- may need to partially release popliteus tendon and repair later
- place buttress plate posteriorly
- make standard anterolateral window for anterolateral plate
Vumedi video
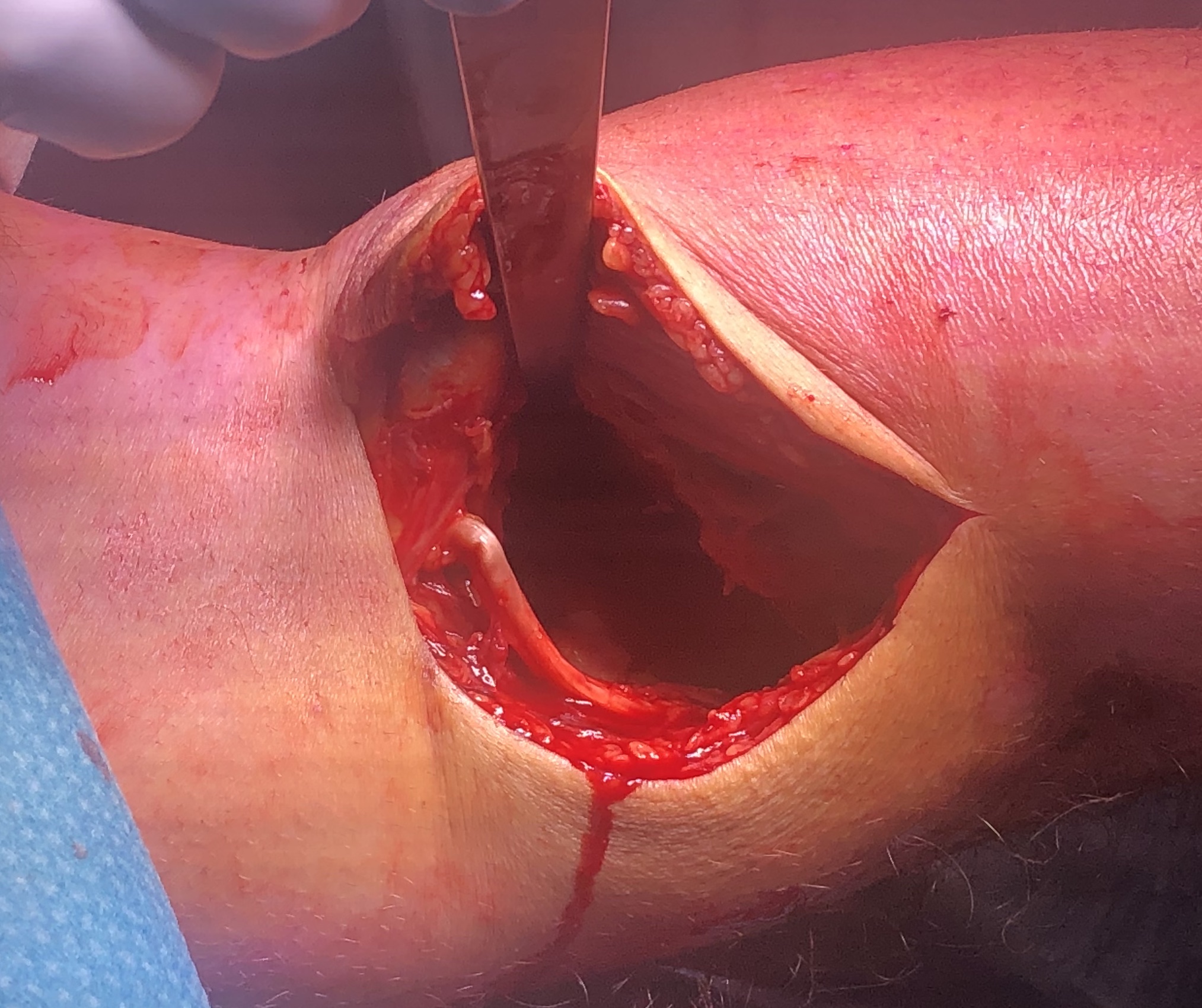
Posteromedial Tibial Plateau Fractures



Posteromedial approach and buttress plate
- Burks modified posterior approach
- put leg over triangle, can let let flop out to get to medial side
- incision based upon posteromedial tibia
- interval between semimembranosus and medial head of gastrocnemius
- medial head of gastrocnemius retracted laterally
- hamstring tendons retracted medially
- place blunt homann gently across back of tibia to expose fracture
- subperiosteal release of the popliteus muscle
- place posterior anti-glide buttress plate
Vumedi video
https://www.vumedi.com/video/orif-of-bicondylar-tibial-plateau-fractures/
Vumedi video
Arthroscopy assisted Tibial Plateau ORIF
Advantages
- direct visualisation of joint surface restoration
Indications
- Type III depression
Contra-indications
- Type IV / V / VI
- risk of compartment syndrome
- ROM < 110o
Technique
Athroscopy Techniques PDF and videos
https://www.arthroscopytechniques.org/article/S2212-6287(19)30028-3/fulltext
Rehabilitation
Hinged Brace
NWB 8 weeks
Complications
Infection
Shao et al. Int J Surg 2017
- systematic review infection rate 9.9%
- risk factors open fractures, compartment syndrome, longer operative times, smoking, external fixation
https://pubmed.ncbi.nlm.nih.gov/28385655/
Osteoarthritis
Wasserstein et al. JBJS Am 2014
- incidence of TKR 10 years post injury of 7.8% compared to 1.8% in matched cohort
- more likely with older patients and more severe fractures
https://pubmed.ncbi.nlm.nih.gov/24430414/
Collapse / Malunion


Option
1. Distal femoral varus osteotomy and fresh osteochondral allograft




Abolghasemian et al. JBJS Am 2019
- long term follow up of fresh osteochondral allograft transplantation
- large post traumatic osteochondral defects > 3 cm diameter and > 1 cm in depth
- graft survivorship was 90% at 5 years, 79% at 10 years, 64% at 15 years, and 47% at 20 years
https://pubmed.ncbi.nlm.nih.gov/31220027/
2. TKR


Scott et al. Bone Joint J 2015
- 31 patients with tibial plateau fracture requiring TKR at a mean of 24 months
- matched to a cohort of primary OA undergoing TKR
- increased rate of wound complications and stiffness in tibial plateau cohort
- otherwise, no significant difference in postoperative outcomes between the two groups
https://pubmed.ncbi.nlm.nih.gov/25820894/
