Epidemiology
2 groups
1. Elderly
- low velocity injury
- osteoporotic
- need to start bisphosphonates
2. Young patients
- high velocity injury
Anatomy
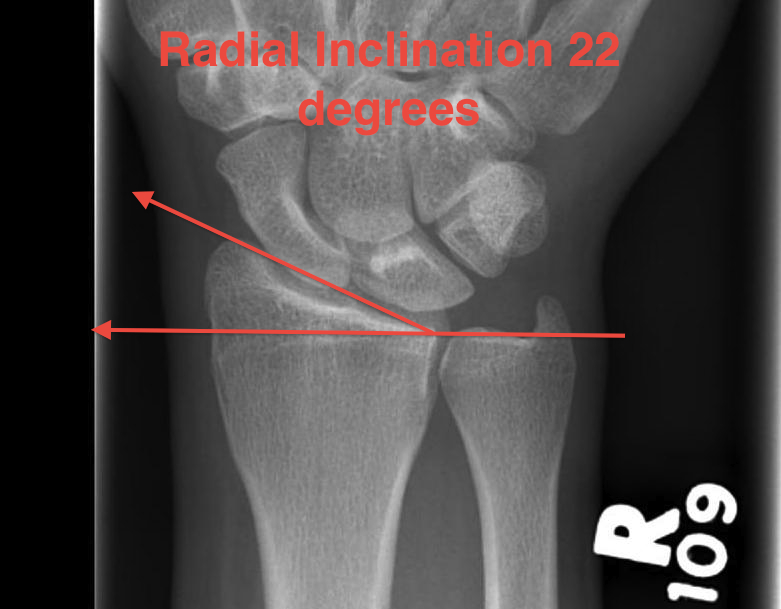
Distal Radius Angles
- radial volar tilt 11°
- radial inclination 22°
- radius is 11 mm longer than ulna
- ulna variance 2mm positive on average


3 independent articular surfaces
1. Scaphoid facet
2. Lunate facet
3. Sigmoid notch
Base of ulna styloid
- insertion point TFCC
- insertion point ulno-carpal ligaments
- crucial for stability DRUJ
3 Columns
1. Lateral radial
2. Medial radial
- dorsal medial radial
- volar medial radial
3. Ulna column
- ulna styloid and TFCC
Volar radius
- subject to compressive forces
- thicker and stronger
Dorsal radius
- subject to tensile forces
- thinner and cancellous
Associated Injuries
- TFCC tears
- SL ligament
- LT ligament
Fracture Patterns
Frykman Classification
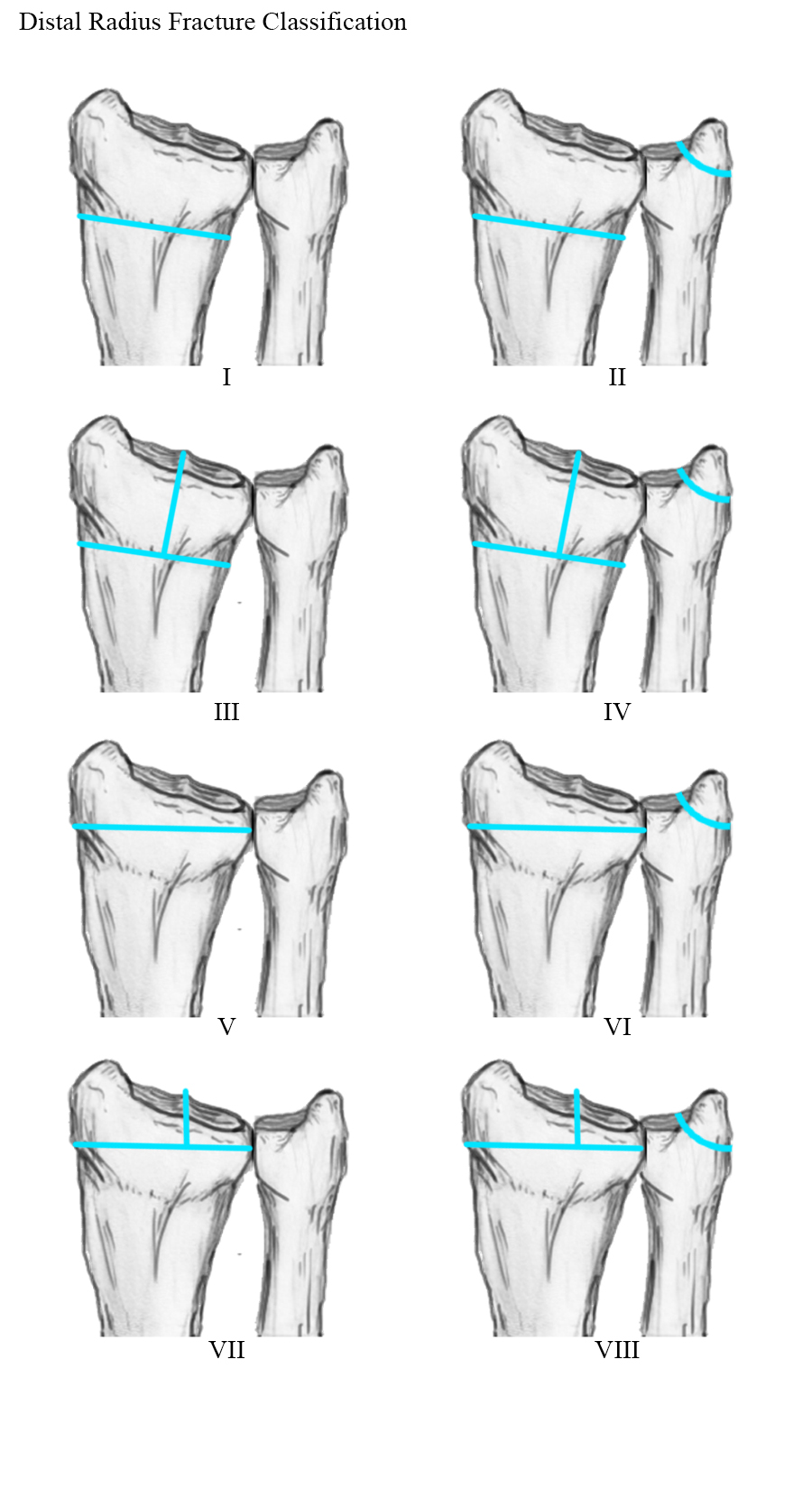
Radial Styloid and Lunate Fragments

Dorsal ulna / volar ulna




Eponyms
Colle's Fracture
- distal radial fracture with dorsal displacement

Smith's Fracture
- distal radial fracture with volar displacement
- need long arm cast in supination

Volar Barton's
- volar intra-articular fragment
- inherently unstable
- usually need volar buttress plate



Dorsal / Reverse Barton's
- dorsal intra-articular fragment


Chauffeur's Fracture
- radial styloid fracture
- ORIF displaced > 2mm (K wires / partially threaded screws / radial styloid plate)
- ensure not missing perilunate dislocations




Management
Initial
All fractures should be reduced initially and reassessed
- conscious sedation
- 2 minutes of traction / reduction of deformity
- backslab / elevation in gallows
- re-xray


CT for further evaluation of articular congruency
Indications for surgery
Absolute
- open fracture
- acute severe CTS
Relative
- failure to obtain and maintain adequate reduction
- instability
- articular incongruency
- likely unstable / dorsal comminution

Unacceptable reduction
1. Distal radial Step > 2mm
- leads to RC OA radiographically
- not proven to lead to dysfunction


2. Articular incongruency sigmoid notch / DRUJ > 2 mm


3. Radial shortening > 5 mm
- leads to ulnocarpal abutment
4. Radial inclination < 15o
5. Sagittal tilt
- > 15o dorsal
- > 20o volar
- +/- marked dorsal comminution
7. Risk carpal subluxation
- Barton's fracture / dorsal Barton's
8. Ulna styloid
- no indication to treat unless unstable DRUJ
Options
K wires
Volar / Dorsal plates
External Fixation
Results
Operative v Nonoperative
Arora et al JBJS Am 2011
- RCT
- MUA & cast v plate fixation in > 65 year olds with displaced fractures
- no significant difference in functional outcome at one year
- improved grip strength in operative group, and better xray measurements but increased complications
K wire v Plates
Marcheix et al J Hand Surg Eur Vol 2010
- RCT of pins v fixed angle plate in dorsally displaced unstable fractures in patients > 50
- extra and intra-articular
- fewer loss of reduction and better functional scores at 6 months with fixed angle plates
Rozental et al JBJS Am 2009
- RCT of ORIF v K wire in 45 patients
- ORIF better functional scores early
- similar outcomes at one year
Plates v External Fixation
Abramo et al Acta Orthop 2009
- RCT of 50 patients unstable comminuted distal radial fractures
- at one year better ROM and fewer malunions in group treated with trimed plate
- no difference in subjective outcome
Leung JBJS Am 2008
- RCT of pins / external fixator v locking plates for intra-articular fractures
- significantly better outcome in locking plate group
Grewal et al J Hand Surg 2011
- RCT ORIF v external fixation
- ORIF better function early
- similar outcomes at one year
Surgical Techniques
1. Percutaneous K Wire




Indications
- extra-articular unstable fractures
- young people without osteoporosis
- minimal comminution
Technique of Colles / Extra-articular fracture / Dorsal displacement
GA
- reduction of fracture
- check under II
Radial K wire
- distal to proximal
- insert percutaneously to bone
- can make small incision / blunt dissect to protect branches SRN
- Kapandji technique or simply cross fracture site
- engage other cortex
- 1.6 or 2 mm K wire
Dorsal K wire Kapandji technique
- percutaneous
- insert by hand into fracture site
- tilt to reduce dorsal displacement of distal fragment
- drive into proximal radius and engage volar cortex
2. ORIF with locking plates


Advantages
- accurate restoration of intra-articular anatomy
- stable fixation
- early mobilisation
Equipment
Locking plates
- volar / radial styloid / dorsal plates
- screws act as fixed angle devices
- screws variable angle

Fragment specific sets
- pin fixators / paper clips
- good for dorso-ulna fragments
- variable angle screws
Technique
Volar / Henry approach
- can extend into CTD if required
- floor of FCR
- divide fascia
- radial artery laterally
- palmar cutaneous branch median nerve medial side FCR
- elevate pronator quadratus from radial to ulna
- release BR if required
- do not incise volar capsule (cut RSC / RL and other important ligaments)
- doing so can lead to volar RC instability
Reduce fragments
- pull out to length / correct angulation
- temporarily stabilise with K wires
- check alignment
- apply volar plate
- check orientation of distal screws with K wire to ensure not in joint
- on lateral, raise hand 30o to view joint
- screw fixation in scaphoid and lunate fragments
- long screws to engage dorsal cortex (24 - 26mm)
- radial styloid plate if required
Volar ulna approach indications
- perform CTD
- use interval between long flexors and FCU to access DRUJ and volar-ulna radius
Dorsal approach
- if unstable dorso-ulna fragment
- midline incision
- open 3rd compartment
- open 4th and sharply dissect radially
- may wish to close ER under tendons to protect from plate
Post op
- POP backslab for 10 days
- early ROM if stable
3. External Fixation + / - Supplemental K wires

Indications
- compound fractures
- severe unreconstructable injuries
- very osteoporotic bone
Technique
- 2 x half pins dorsal radius (4mm)
- 2 x half pins IF / MF metacarpal (3 mm)
Complications
1. Tendon problems
- most common problem
A. FPL ruptures
B. FCR tenosynovites
C. Dorsal extensor tendon involvement from protruding screw or from dorsal plates
2. Stiffness
Can continue for up to 18 months
- difficulty regaining full supination / pronation
3. Median nerve dysfunction
4. CRPS 2
- excessive traction on median nerve / long surgery
4. Radial artery pseuodoaneurysm
