Anatomy
Terminal branch of the posterior cord
- lateral to radial nerve
- behind axillary artery
- runs over inferolateral border of SSC
- enters quadrangular space
Quadrangular space
- SSC superiorly anterior
- T major inferior
- T minor superiorly posterior
- long head triceps and humerus
Divides into anterior and posterior branches
Anterior branch
- curves around SNOH
- deep to deltoid
- 4-7 cm inferior to corner acromion
- supplies anterior and middle portions deltoid
Posterior branch
- supplies T minor and posterior deltoid
- sensory branch
3 distinct fascicles
- T minor
- deltoid (supero-lateral)
- superior lateral cutaneous branch
Aetiology
1. Traumatic
2. Iatrogenic
3. Quadrilateral Space Syndrome
4. Brachial Neuritis
5. SOL
1. Traumatic
A. Shoulder Dislocation
- 10-20% incidence post dislocation
Blom et al Acta Chir Scand 1970
- 9 complete and 15 partial lesions
- all recovered within 1 - 2 years
Gumina JBJS Br 1997
- high rate in elderly > 40 (50%)
- all recovered by 3 years
- high rate of RC (20%)
B. Proximal Humeral fracture
C. Brachial Plexus injury
- rarely isolated
- in conjunction with other injuries
- upper trunk
D. Blunt trauma to deltoid
2. Surgery
A. Deltoid-Splitting approach
- lies 5cm lateral to anterolateral corner of acromion
B. Deltopectoral approach
- undue care at inferior level of SSC
3. Quadrilateral space syndrome
Mechanism
- Compression in position ER and abduction
Symptoms
- get pain and paraesthesia in shoulder
- can have chronic dull ache
Signs
- usually no deltoid atrophy or sensory changes
Investigation
EMG
- normal
Angiogram
- shows compression of posterior humeral circumflex artery with less than 60o abduction
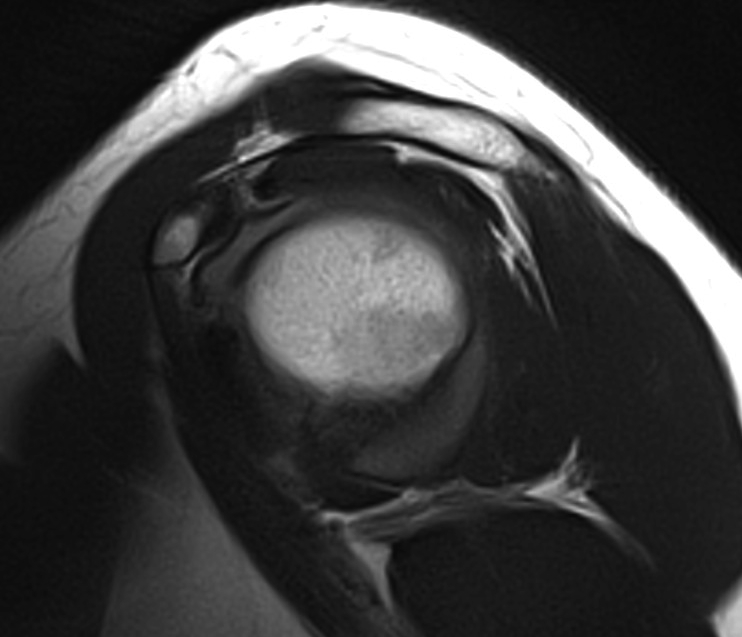
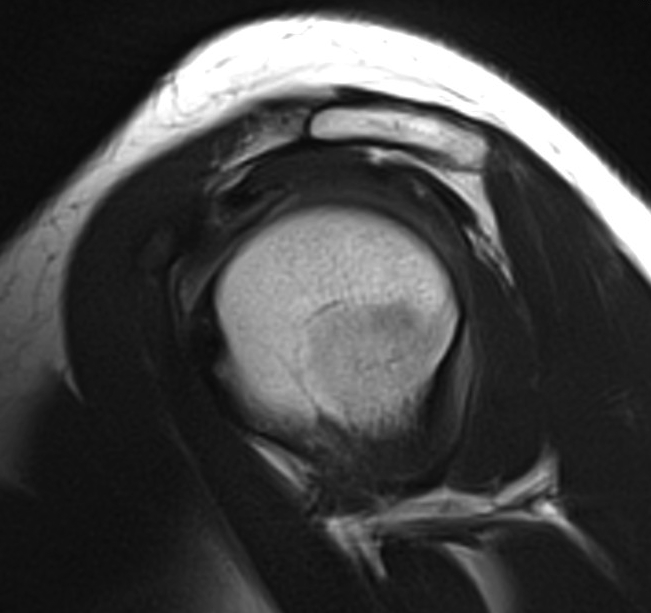
MRI
- may shows changes in deltoid and Tm
Mangement
- usually just observation
- occasionally need to decompress scar tissue or fibrous band
4. Parsonage-Turner Syndrome
Brachial neuritis
- spontaneous development severe shoulder pain
- then develop loss of motor function
- usually also LTN, SS nerve, but occasionally isolated
Management
- can treat with steroids
- usually good prognosis
5. Nerve compression from mass effect
Cause
- aneurysm, tumour
History
No history trauma
- suspect mass effect / quadrilateral space syndrome / brachial neuritis
Pain then loss of function
- suspect brachial neuritis
History dislocation
Examination

Wasting Deltoid
Weakness of shoulder abduction
Numbness in Regimental patch
- variable
DDx
1. Upper trunk injury / root injury (C5/6)
- will also have injuries to
A. SS nerve
- IS / SS
- remember dislocation may cause RC tear
B. Subscapularis
C. Biceps
2. Posterior cord injury
- will also have injuries to
A. Radial nerve
- triceps, WE, FE, thumb extension
B. Thoracodorsal
- Lat Dorsi
C. Upper and lower subscapular
- SSC
NCS / EMG
Diagnose higher lesion
- reference point for recovery
MRI
Mass lesions
Atrophy of T minor
Assess RC
Operative Management
Indications
- no clinical or NCS / EMG sign of recovery at 6/12
- open wounds / stab wounds
Timing
Best results
- reinnervation must occur before one year
- otherwise get degeneration of NMJ
- i.e. surgery must occur by 9 months
Options
No muscle transfer for deltoid
- nerve repair
- neurolysis
- nerve grafting
- nerve transfer
1. Neurolysis
Indications
- if nerve intact but encased in scar or compressed by fibrous bands
Technique
- identify nerve
- use nerve stimulator intra-operatively
- stimulation of nerve will cause muscle contraction if intact
- uncommon
2. Neurorrhaphy
Indication
- laceration
Technique
- direct repair of laceration
- if in first few weeks
3. Nerve grafting
Indications
- neuroma usually at or in quadrilateral space
2 Incision Technique
Sural nerve graft
- anastomose anteriorly, then pass through
- anastomose posteriorly
Lateral decubitus
- access anterior and posterior shoulder
- allows sural nerve harvest
Deltopectoral approach
- release half or all of P major (leave cuff for repair)
- must release conjoint tendon and P minor
- do so 1cm from origin
- expose axillary, radial and MCN
- use nerve stimulator to ensure nerve not working
- identify and protect axillary artery and vein
- if deltoid active, neurolysis
Identify neuroma
- if deep
- posterior approach to shoulder
Posterior vertical incision
- lateral border acromion to posterior axillary crease
- mobilise inferior border deltoid superiorly
- find nerve as exits quadrilateral space
- identify deltoid fascicle using nerve stimulator
Results
Allnot Int Orthop 1991
- 23/25 isolated sural nerve grafting achieved M4 or M5 strength
4. Neurotisation / Nerve transfer
Concept
- use branch of radial nerve
- transfer into motor branch axillary
- single incision
Technique
- posterior longitudinal approach to arm
- find AXN under wasted deltoid, exiting above T Major
- identify anterior branch of AXN going into muscle
- ensure not branch to T minor or sensory branch
- develop interval between long and lateral heads
- find radial nerve in groove between medial and lateral heads
- will be exiting below T Major between long and humerus
- harvest branch to long or medial head triceps
- long may be better as has two sources nerve supply and less functional impairment
- check with nerve stimulator
- repair with 9.0 nylon under microscope
Results
Leechavengvongs et al J Hand Surg Am 2003
- all 7 patients had M4 power
- 5 excellent and 2 good results
- no demonstrable loss of elbow extension power
