Epidemiology / Etiology
1-2% of all spinal injuries
Bimodal distribution
- mid 20s: high energy trauma
- over 80s: low energy mechanism
Falls / MVA / Diving into shallow water
Landell's Classification
Type 1. Isolated lateral mass fracture
- axial compression and lateral flexion
Type 2. Posterior AND anterior arch fractures (Jefferson)
- axial compression
- +/- transverse atlantal ligament injury
Type 3. Posterior OR anterior arch fracture
- axial compression with hyperextension (posterior arch)
- axial compression with hyperflexion (anterior arch)

Associated injuries
High rate of concomitant spine fractures
Ylonen et al World Neurosurg 2021
- combination of X-ray, CT, MRI of 47 patients with C1 fracture
- 89% incidence of concomitant cervical spine fractures
- 76% incidence of concomitant C2 #
Associated symptoms
Vertebral artery injury
- nausea, vomiting, tinnitus, impaired vision, and drop attacks
Collet-Sicard syndrome
- posttraumatic lesion to the lower 4 cranial nerves (IX–XII)
Atlas burst fracture / Jefferson Fracture
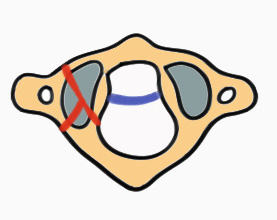
Stability
Stable
- transverse atlantal ligament (TAL) intact
Unstable
- transverse atlantal ligament (TAL) disrupted
- bony avulsions
- intra-ligamentous disruptions
X-ray
1. Lateral mass displacement (LMD)
Open mouth odontoid view
- sum of lateral mass displacement
- increased LMD suggests TAL injury
Kopparapu et al J Neurosurg Spine 2022
- Rule of Spence: LMD > 6.9 mm predicts TAL injury, instability and need for surgery
- developed in 1970's
- inaccurate in predicting TAL injury
- LMD > 8 mm seen in 90% of patients with transverse ligament injury

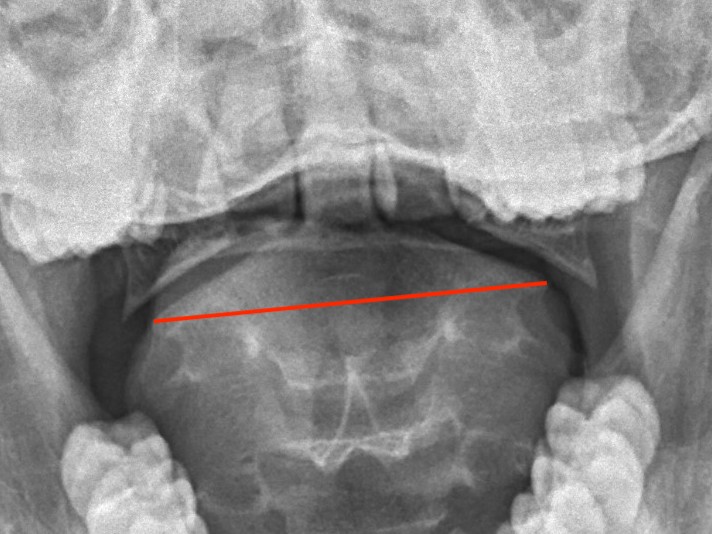
Lateral mass displacement

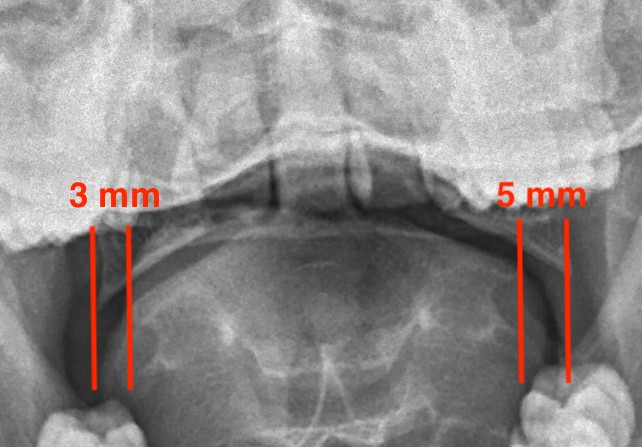
Increased lateral mass displacement of 8 mm
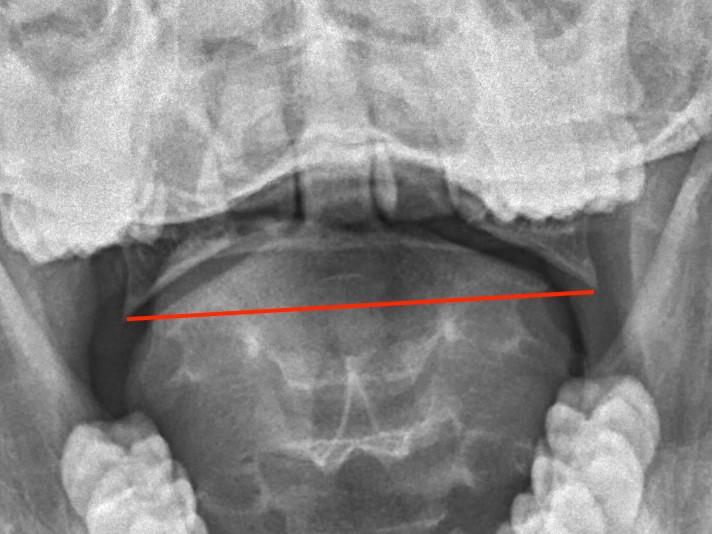
2. C1/C2 ratio
- C1/C2 ratio > 1.1 80% sensitive of TAL injury
- C1/C2 ratio > 1.15 100% specific of TAL injury
3. Atlantodens interval (ADI)
> 3 mm ADI suggests TAL injury

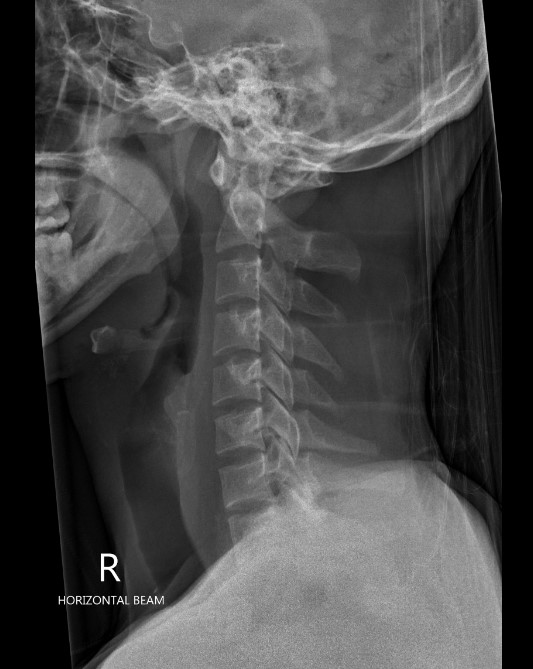
Lateral radiographs demonstrating increased ADI
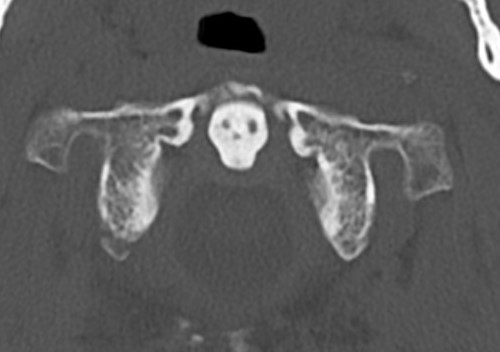
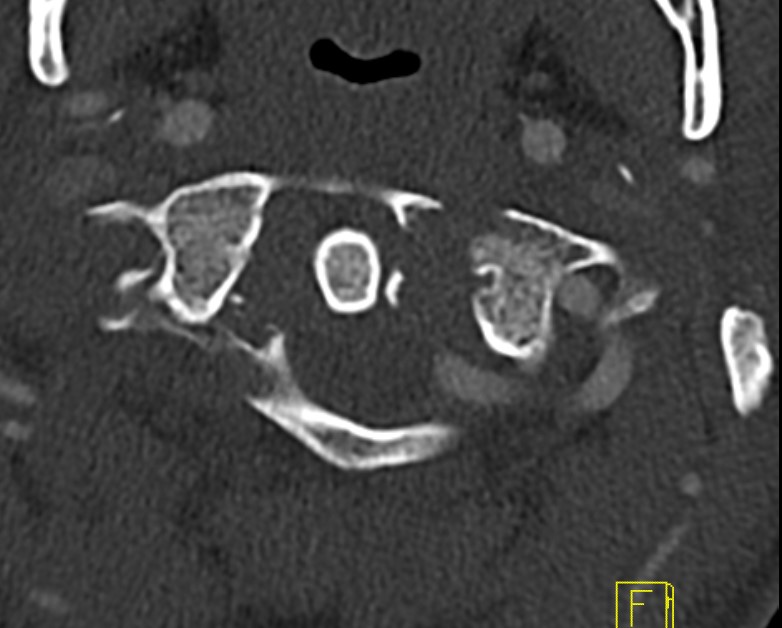
CT
Better defines displacement, ADI, LMD and bony avulsions of the transverse ligament
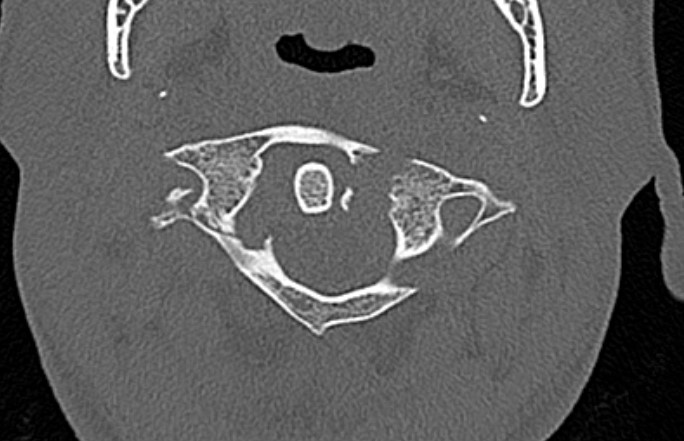
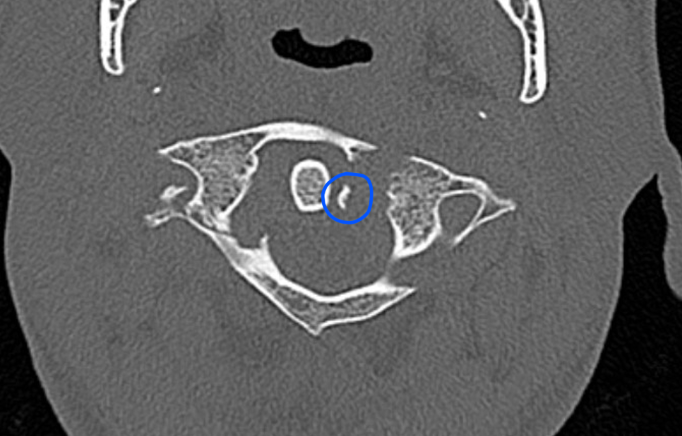
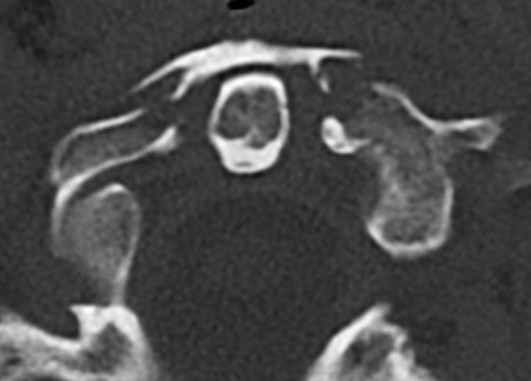
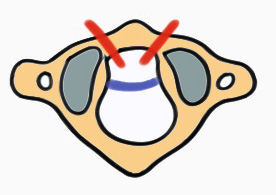
CT axial slices "Jefferson" (burst) fracture with bony avulsion (blue) of the transverse ligament


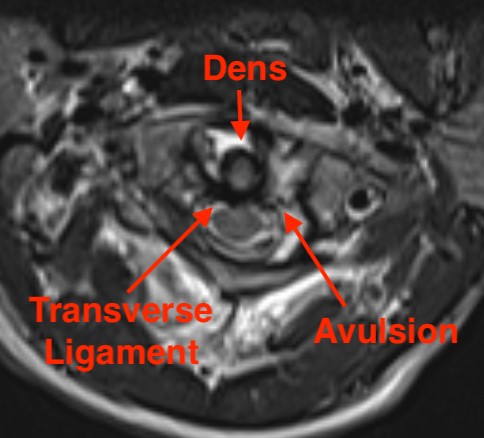
MRI
Assess ligamentous injury, specifically transverse ligament
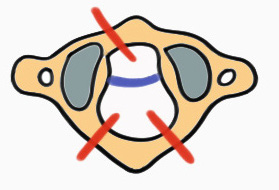
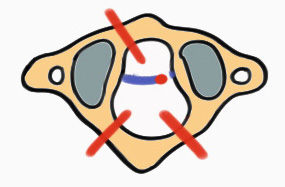
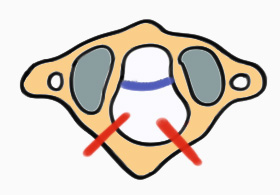
Dickman et al Neurosurgery 1996
- type I: intra-substance TAL tears
- type II: fractures or avulsions of the TAL from the tubercle of the lateral mass of the atlas
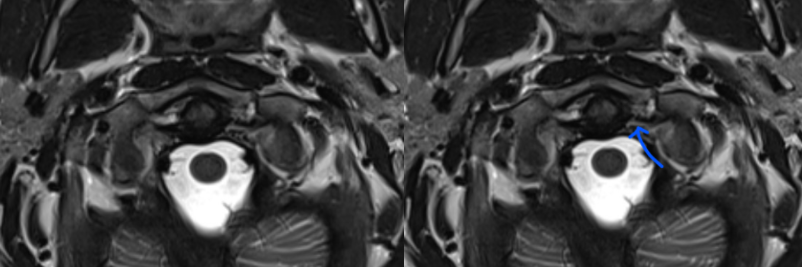
MRI demonstrating intra-ligamentous injury (blue arrow)
MRI demonstrating avulsion of the TAL on the left side
Stability
Indications of instability
- transverse ligament avulsed / disrupted on CT / MRI
- LMD > 7 mm
- ADI > 3-5 mm
- Peg fracture
Management
Non-operative Management
Indication
Stable fractures
- anterior / posterior arch fractures
- Jefferson with intact TAL
Unstable fractures
- ? increased union rates and better outcomes with operative management
Operative versus Nonoperative for unstable atlas fractures
- 24 unstable atlas fractures
- 13 treated with C1/C2 fixation - 100% fusion
- 11 treated with halo-vest - 73% fusion
- reduced pain and improved outcomes with surgery
- 53 unstable atlas fractures
- 32/53 ORIF - 100% union
- 21 treated with halo-vest - 71% union, continued increased LMD
- those treated with halo-vest had worse neck pain and outcome scores
Options
Collar
Halo thoracic brace

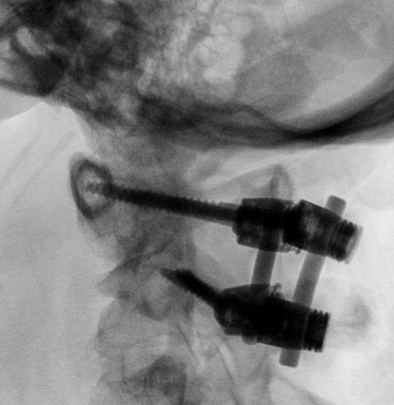
Post reduction halo xray


Flexion and extension views demonstrating stable Jefferson fracture post halo treatment
Operative Management
Indication
1. Unstable C1 fractures
2. Non-union / ongoing instability after non-operative treatment
Options
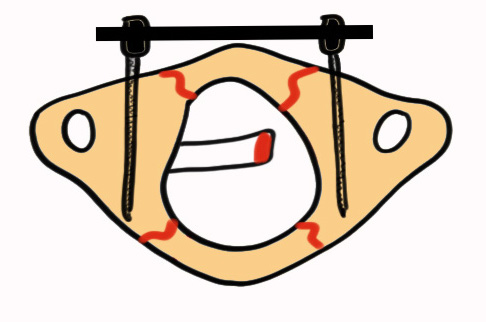
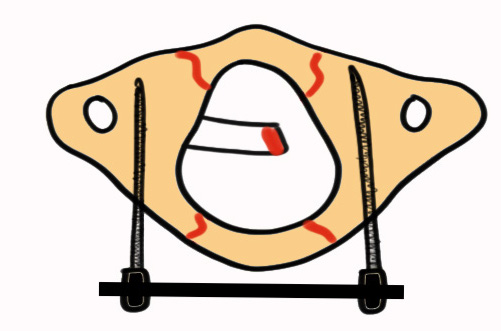
C1 ORIF
C1/2 fusion
C1 ORIF
Advantage
- preserves C1/C2 motion
Posterior / anterior approach
- bicortical lateral mass screws
- reduction
- bridge plate / rod construct
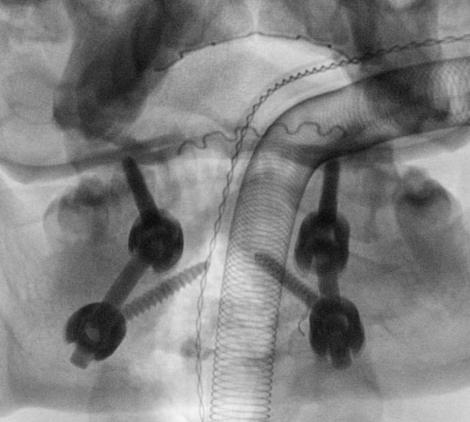
C1/C2 fusion
Technique
Goel Harms
- C1 lateral mass screw
- C2 pedicle screw monocortical to reduce risk of vertebral artery injury
- preoperative CT angiogram important
- must avoid medial penetration of canal
Surgical technique PDF C1 C2 fusion
Vumedi technique Goel-Harms C1/C2 fusion
Results
C1 ORIF
- 22 patients
- posterior approach and lateral mass screw / plate construct
- 100% union on CT at 9 months
- 20 patients with anterior / trans-oral approach
- lateral mass screw / plate construct
- 100% bony union at 6 months
C1 ORIF vs C1/2 Fusion
Yan et al J Neurosurg Spine 2022
- RCT (n=73) ORIF vs C1-2 fusion
- ORIF shorter operative time, reduced blood loss, less radiation, shorter hospital stay, cheaper (all p<0.001)
- improved outcomes and ROM in ORIF group