Definition
A GH dislocation which has been missed for a significant period of time
- time period is arbitary
- > 3-6 weeks
Pathology
Humerus soft and osteoporotic
Significant soft tissue contractures
1. Anterior / subcoracoid dislocation
Beware
- scarring to NV structures
- RC tears including SSC, especially > 40
- anterior glenoid wear / can have significant bone loss
- large engaging Hill Sachs / humeral head defects
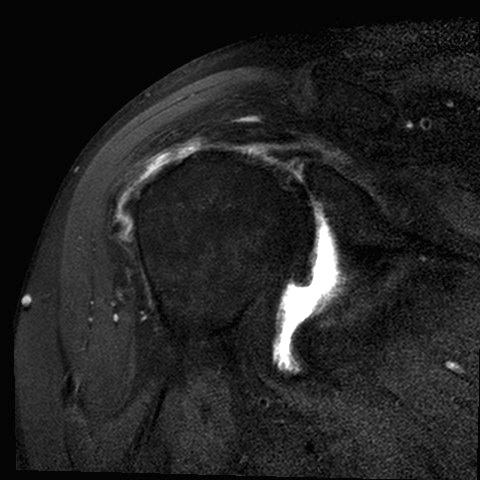
2. Posterior dislocation
- posterior glenoid wear
- reverse Hill Sach's / large anteromedial defects
Epidemiology
Anterior 41%
Posterior 59%
Aetiology
Multi trauma
Seizures
Poor patient mental function
History
Limitation ROM
History multi trauma / seizures
Previous treatment
- often have had inadequate X-rays
- extensive physiotherapy / injections
Examination
Usually some asymmetry
Some reduction ROM
Palpate humeral head anteriorly / posteriorly
X-rays
Scapular AP view
Scapular lateral
Axillary lateral
CT
Aids diagnosis and preoperative planning
Management
Non Operative
Indications
- elderly
- minimal functional limitation
- significant medical issues
Only operate if significant clinical problems
- anterior more difficult than posterior to solve
Operative
Closed reduction
Issues
1. Timing
- has been successful up to 6-8 weeks
- most successful outcomes in literature < 4 weeks
2. Humeral head impression
- if this is locked on glenoid, closed reduction is contraindicated
3. May be unstable afterwards
- need further open procedure
- need careful postoperative monitoring
- regular xray surveillance
Chronic Anterior Dislocation
1. Large Humeral Head Defect
Hill Sach's
- posterolateral defect
- manage according to size
Defect < 40%
A. Elevate and Bone graft defect
- < 4 weeks in young patient
- adequate bone, salvageable cartilage
- posterior approach
- split deltoid / L shaped Infraspinatous tenotomy
B. Advance Infraspinatous +/- GT
- posterior approach
- < 20% IS alone
- if larger must also take GT
Defect > 40%
A. Allograft
- young patient
- pre-op CT to estimate humeral head size
- appropriate sized femoral / humeral head
B. Prosthesis
- often significant OA with long standing dislocation
- anterior glenoid deficiency
- older patient
- increase retroversion of humeral component
- may need to address anterior glenoid deficiency
2. Glenoid Deficiencies
Indicated when > 20-25% anterior glenoid eroded
Bristow / Latarjet
Glenoid Reconstruction
- humeral head
- iliac crest


3. Soft tissue deficiencies
Always combine with anterior labral repair +/- inferior capsular shift
4. Rotator cuff tears
Significant issue
- if massive cuff tear, may lead to chronic instability
- very difficult to treat
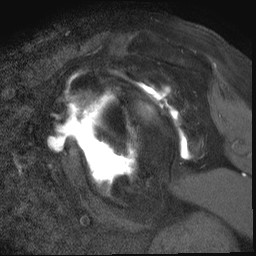
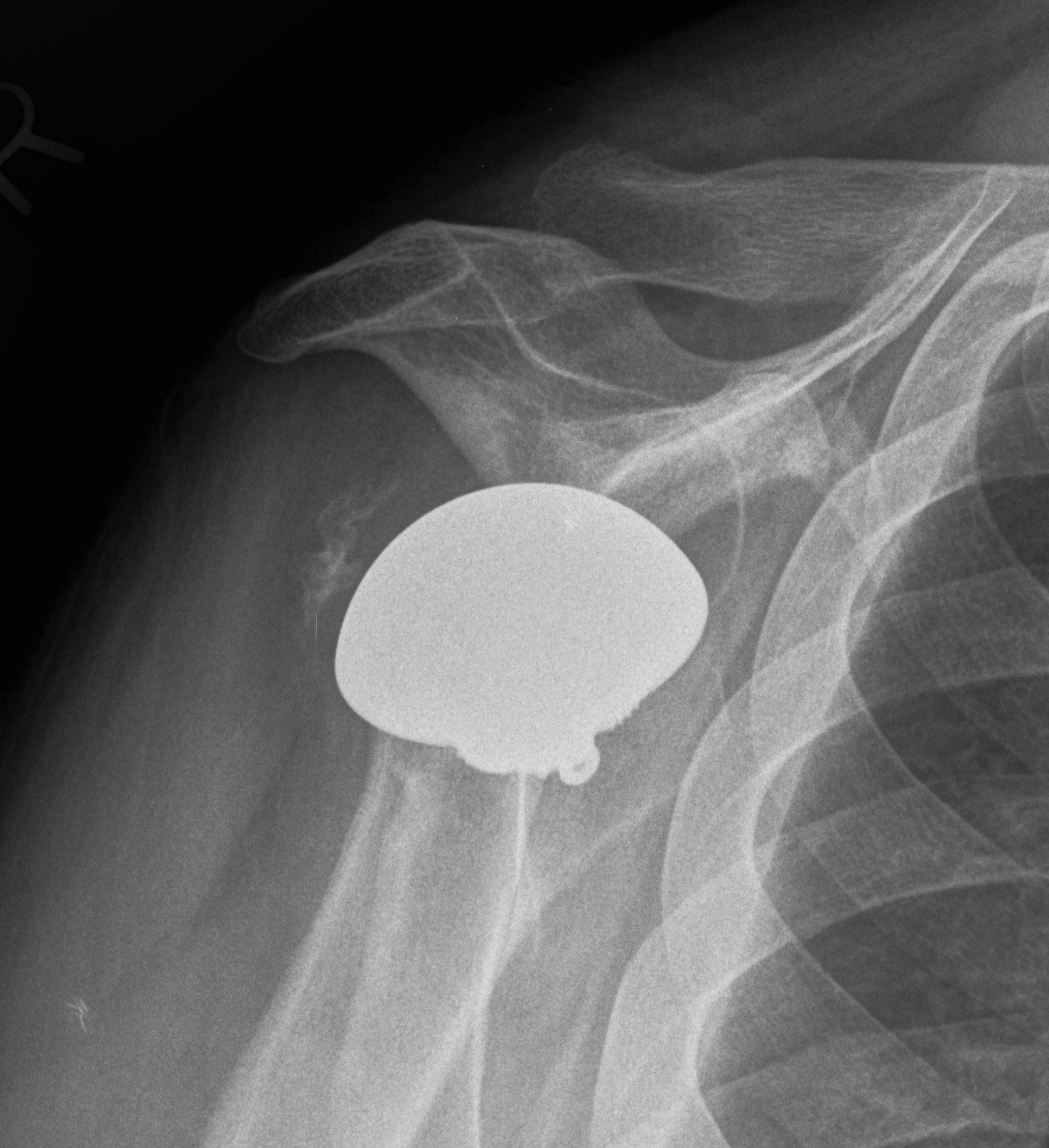
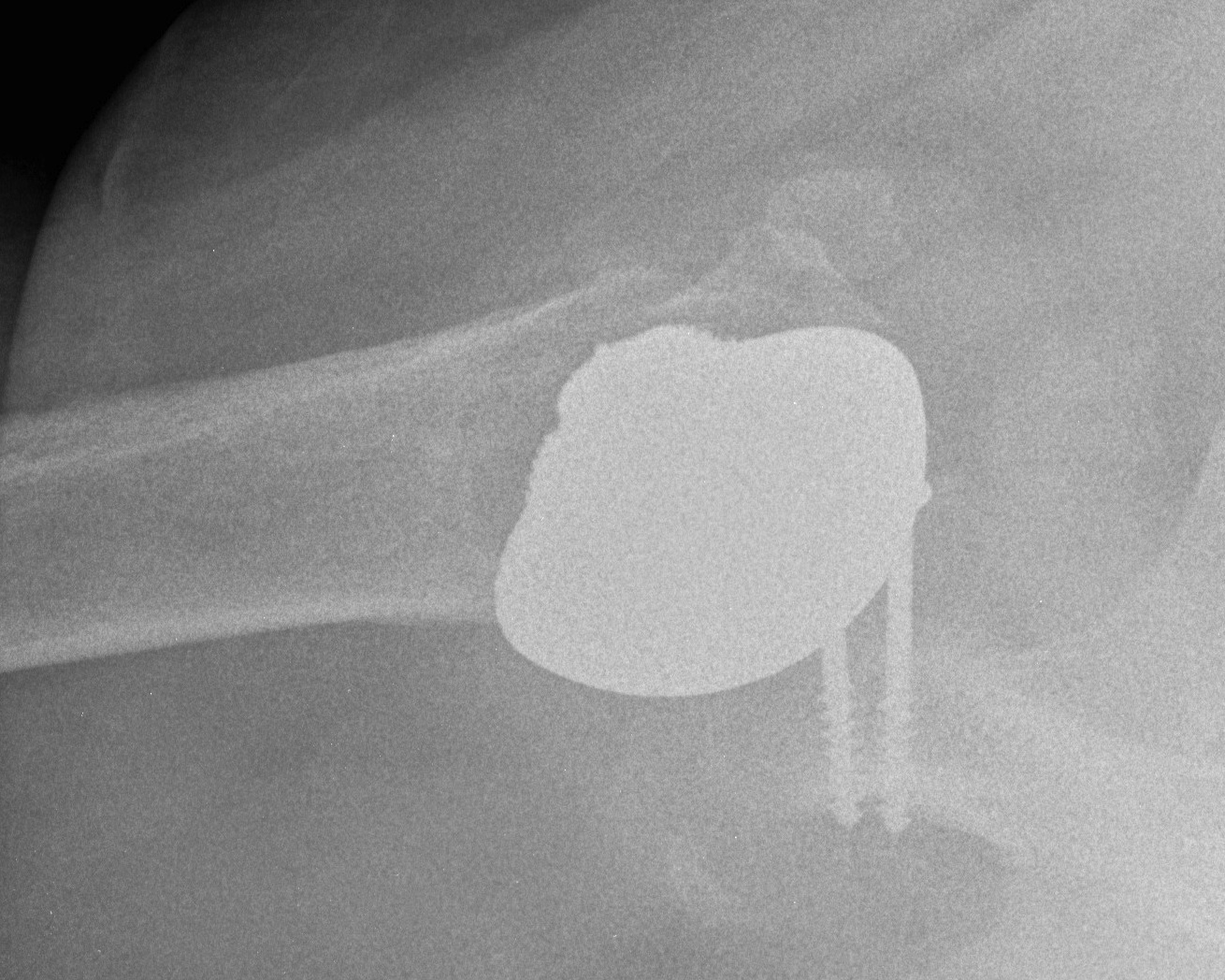
CASE 1
50 year old, missed locked anterior dislocation one year
- head severely mis-shapen
- missing 50% glenoid
- massive rotator cuff tear
Treatment
- open reduction
- shoulder hemiarthroplasty / humeral head used to bone graft glenoid / rotator cuff repair
- unfortunately rotator cuff repair failed, and developed recurrent instability
- option: Reverse TSR / fusion



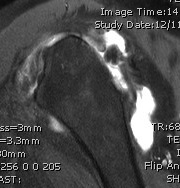
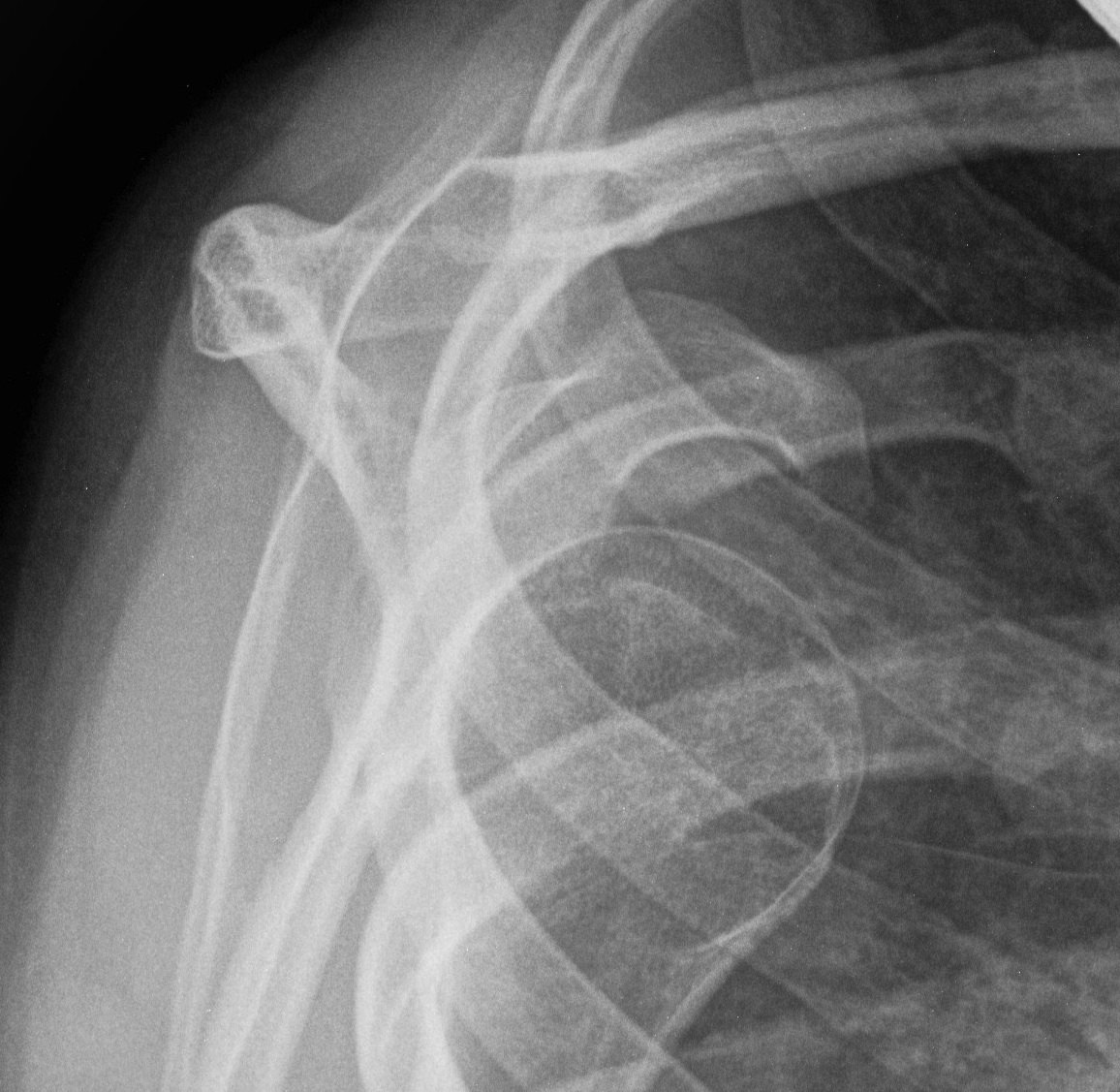
CASE 2
26 year old female
- ligamentous laxity, but no previous shoulder problems
- traumatic anterior shoulder dislocation
- leading to recurrent anterior subluxation
- had an arthroscopic anterior and posterior capsular plication
- shoulder now permanently dislocated anteriorly
- options: open posterior capsular release and latarjet / or fusion

Chronic Posterior Dislocations
Approach
Standard DP approach
- manage SSC depending on operative plan for humeral head defect
- open capsule
- remove any fibrous tissue in glenoid
- use lever to reduce humeral head
- usually can ignore posterior capsular detachments
Manage humeral head / glenoid defects
See Posterior Shoulder Instability
1. Humeral Head defects
Posterior dislocation
- anteromedial
Defects < 40%
A. Disimpaction and bone graft
- < 4 weeks, young patient
- articular cartilage must be salvageable
- via anterior approach
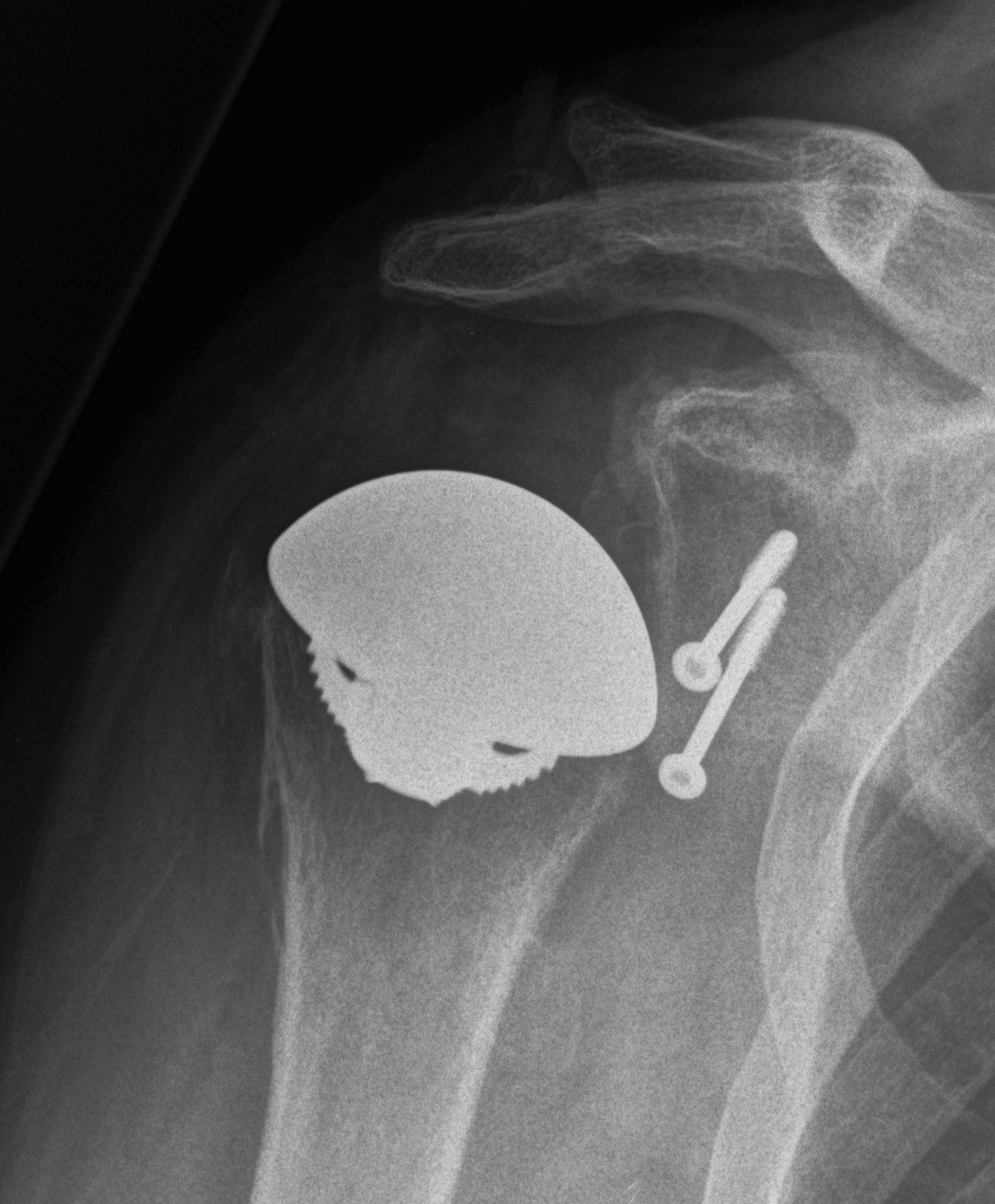
B. McLaughlin
- < 20%, SSC only
- < 40% transfer SSC + LT into defect
- secure with 2 x cancellous screws
Defects > 40%
A. Allograft
- young patient
B. Hemiarthroplasty / TSR
2. Posterior Glenoid Deficiency
May need posterior bone graft
