
Options
Marrow stimulation - microfracture / microdrilling
Cartilage restoration
- Matrix autologous cartilage implantation (MACI)
- Autologous membrane induced chondrogenesis (AMIC)
- Autologous minced cartilage implantation (AutoCart)
- Allogenic minced juvenile cartilage implantation (DeNovo)
- Osteochondral autograft (Mosaicplasty / OAT)
- Osteochondral allograft (OCA)
Concept
Microfracture
- has traditionally been the gold standard but
- best for smaller lesions < 2 cm2
- not indicated for osteochondral lesions
- not as effective in the patellofemoral joint
- results tend to deteriorate over time
Cartilage restoration procedures
- indicated for
- larger lesions / osteochondral lesions / failed microfracture / young patients / athletes
- it is not clear which is the best procedure
- depends on cost / availability
Results
Long term function
- systematic review of microfracture
- improved knee function in 67 - 86% of patients at 6 - 7 years
- systematic review of 6 RCT with minimum 5 year follow up
- better long term outcomes with osteochondral autograft / ACI than microfracture
Return to sport
- return to sport after surgical management cartilage lesions in knee
- microfracture 58%
- ACI 82%
- osteochondral allograft / OCA 88%
- osteochondral autograft / OAT 93%
Indications for surgery
Grade 3 or 4 ICRS lesions
Symptomatic
Knee Osteotomy
Indicated for any malalignment depending on knee compartment affected
Dhillon et al Orthop J Sports Med 2023
- systematic review of cartilage repair +/- osteotomy of the knee
- 5 studies and 1700 patients
- improved outcomes and lower reoperation rates with osteotomy patients
www.boneschool.com/knee/osteotomy
PFJ chondral lesions
www.boneschool.com/knee/chondromalaciapatella
Results
van Tuijn et al Cartilage 2023
- systematic review of microfracture
- worse outcomes in PFJ than in knee condyles
- systematic review of PFJ cartilage lesions in 2000 patients
- clinical patient improvement of various restoration procedures
- MACI 83%
- OAT 78%
- OCA 71%
- AMIC 64%
- OCA had highest failure rate
Tibial tuberosity osteotomy (TTO)
- systematic review of patients with PFJ chondral lesions
- compare isolated ACI versus combined ACI and TTO
- better outcomes with ACI / TTO
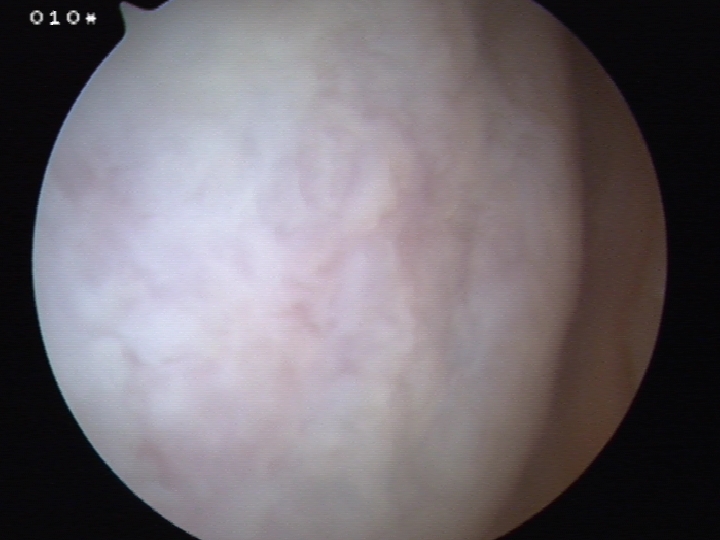
Marrow stimulation / Microfracture / Microdrilling
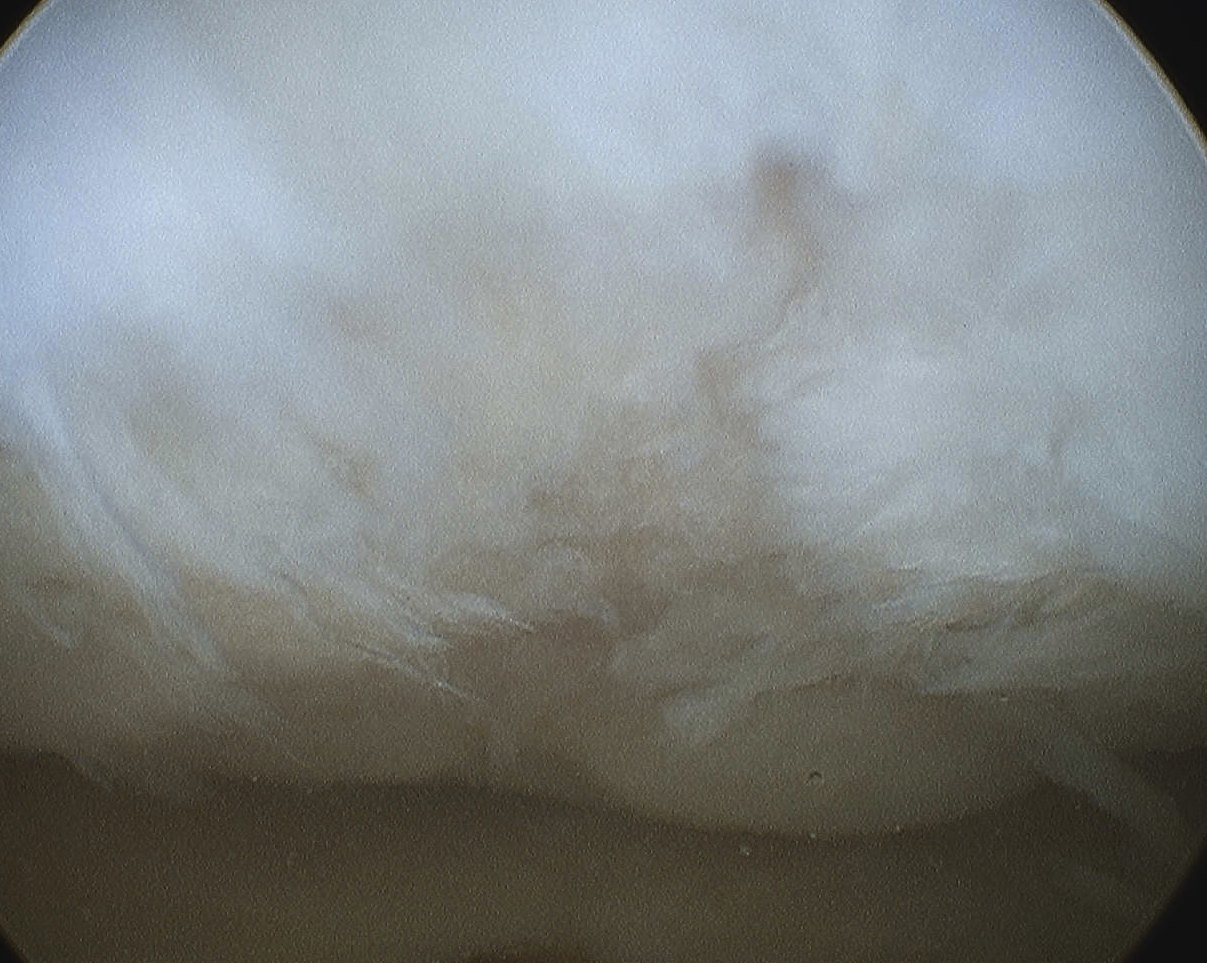

Principles
Pluripotent marrow cells produce fibrocartilage to varying degree
- low stiffness and poor wear characteristics over time
- may be more beneficial to combine with realignment procedure
Indications
- young patient < 40
- < 2 cm2
- chondral defect - not osteochondral defect
- contained defect - cartilage on each side of defect
- BMI < 30
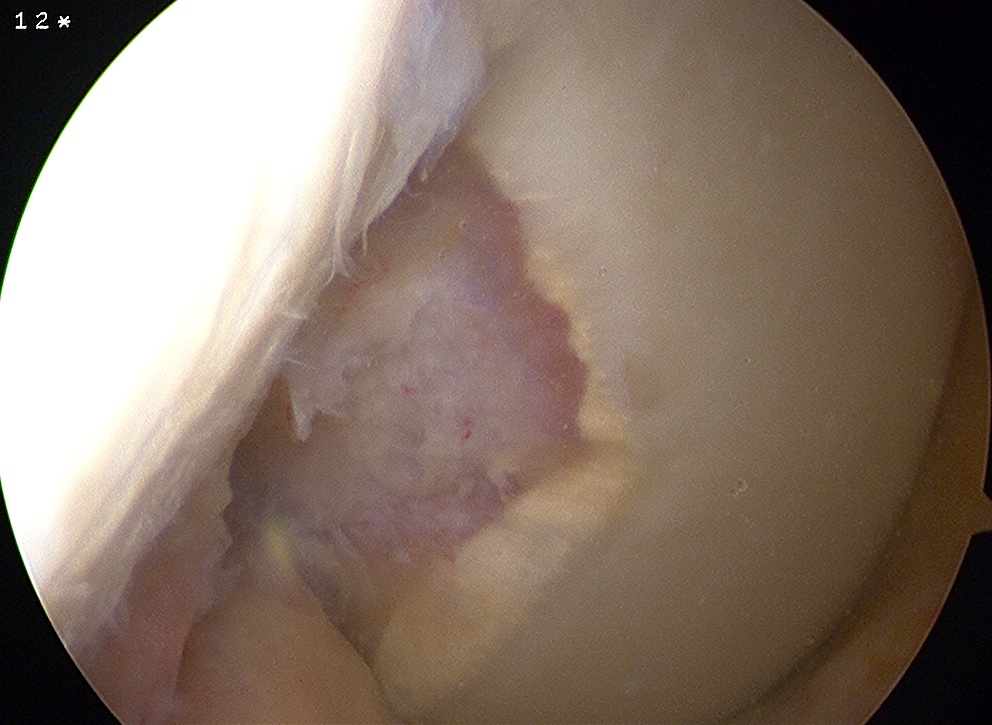
Uncontained lesion on intercondylar notch
Advantage
- simple
- able to perform in setting of unexpected cartilage lesion i.e. ACL reconstruction
Issue
- produces fibrocartilage
- results tend to deteriorate over time

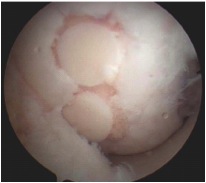
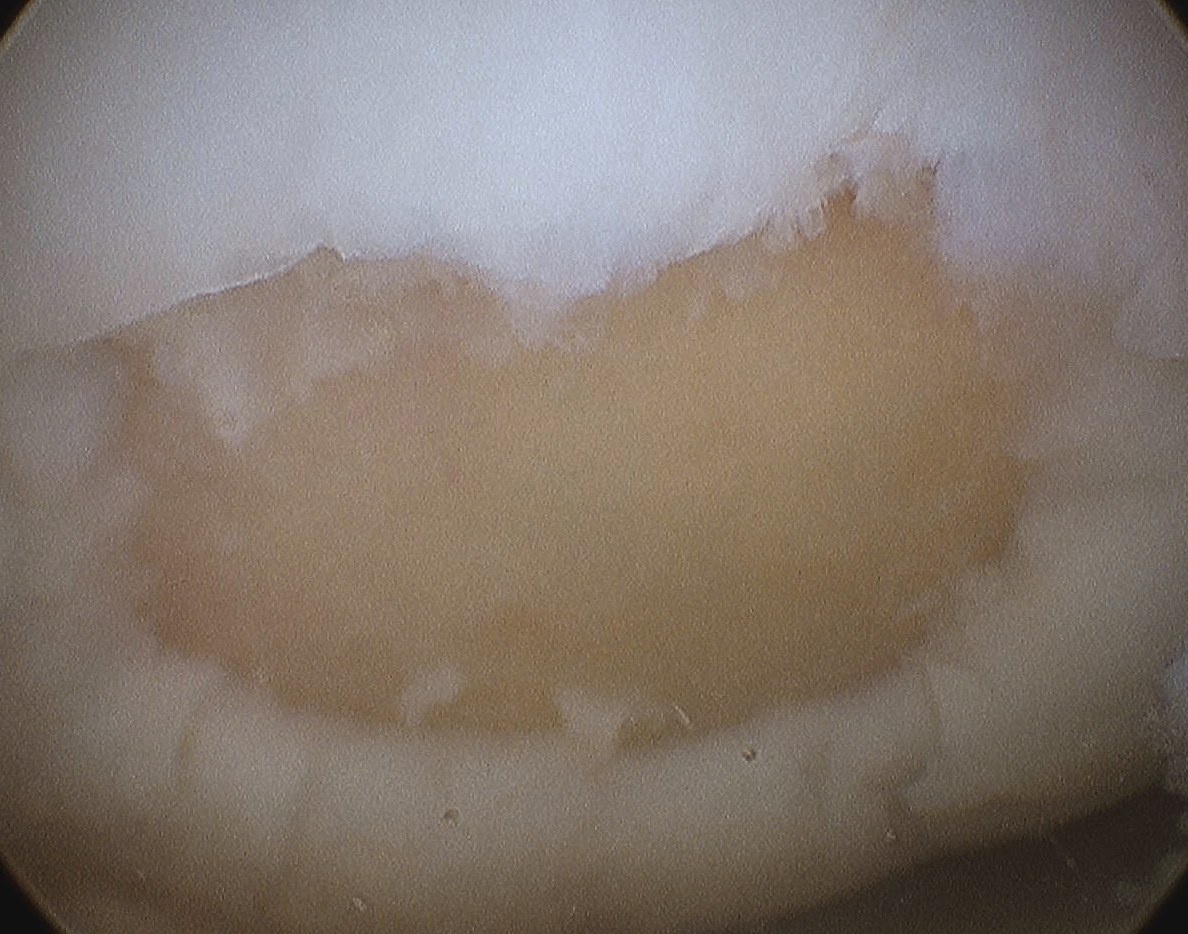
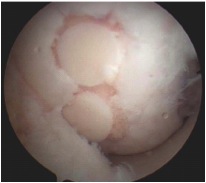
Fibrocartilage response to microfracture
Technique
Debride all unstable cartilage to stable edge
- removed calcified cartilage layer with curette, protect subchondral bone
- create a perpendicular edge which helps to hold the clot
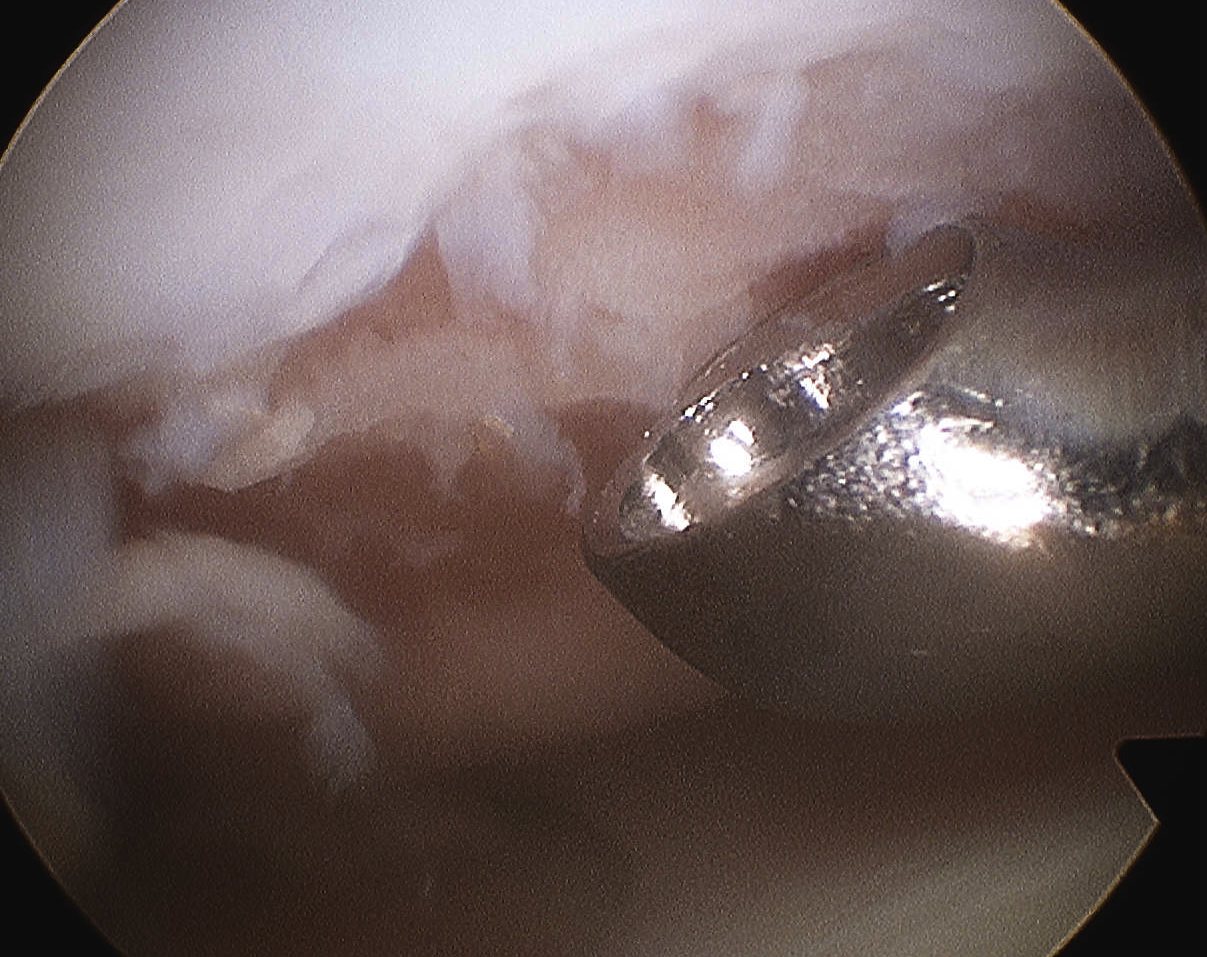

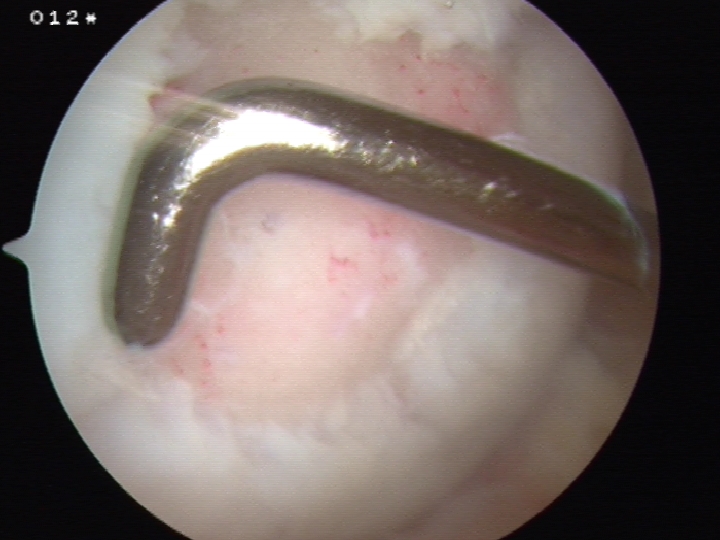
Arthroscopic microfracture awl / 1.6 mm drill
- typically 3-4 mm apart
- depth until see fat globules
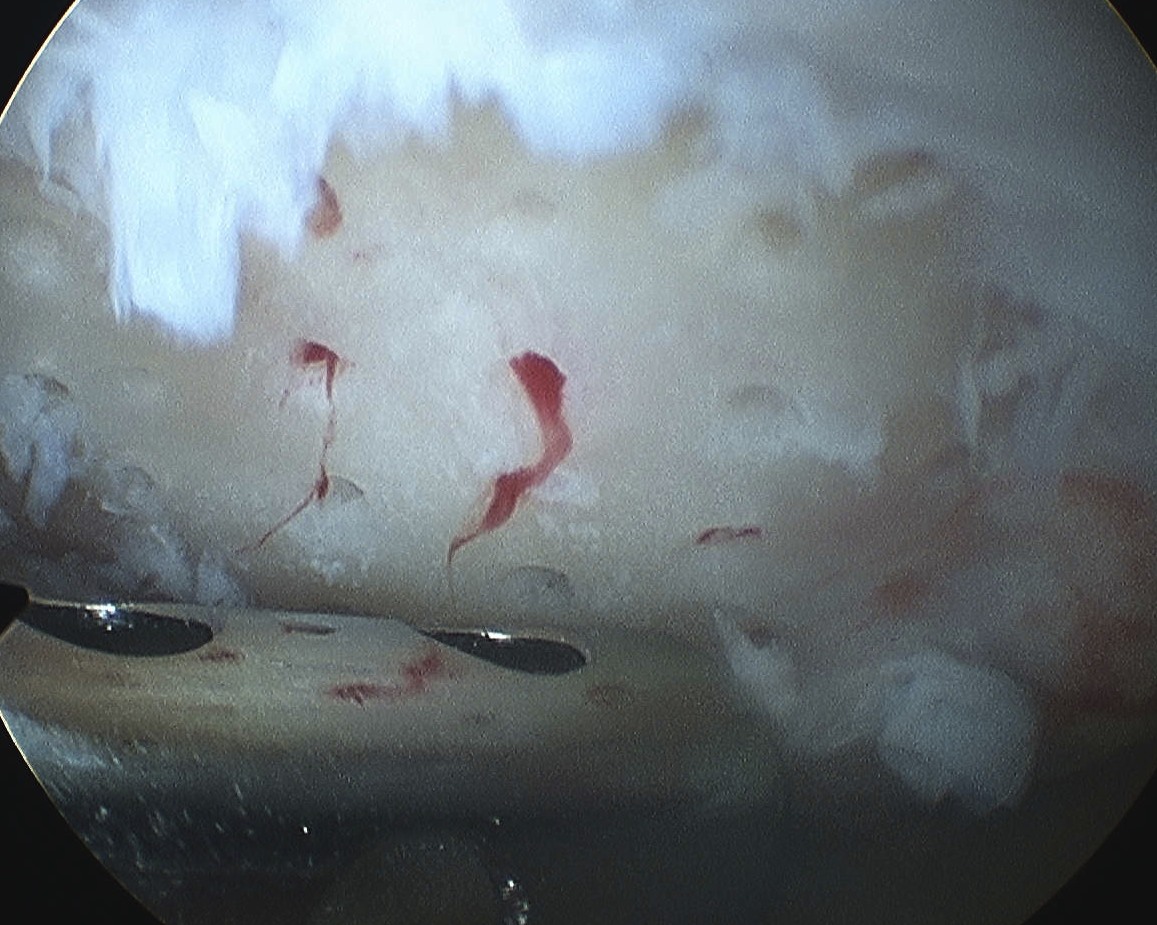
Post arthroscopic drilling with K wire
Results
van Tuijn et al Cartilage 2023
- systematic review of microfracture
- worse outcomes with larger lesions / PFJ lesions / bipolar lesions
Kraeutler et al Orthop J Sports Med 2020
- systematic review of basic science studies
- microfracture versus microdrilling
- improved biology with microdrilling due to increased depth
- reduced damage to subchondral bone with microdrilling
Autologous Cartilage Implantation (ACI, MACI)

Principle
Transplant living viable cells
- capable of synthesizing and maintaining a cartilaginous matrix
- makes a substance physically and histologically similar to hyaline cartilage
First generation ACI - harvest periosteum to secure cells in place
Third generation M-ACI - cells presented on a matrix / membrane for implant
Issues
- 2 stage procedure
- significant costs
Technique
Harvest mature chondrocytes
- biopsy taken from non weight bearing area in notch or lateral edge of femoral cartilage
- cells isolated and washed
- expanded in cell culture
- attached to membrane
- process takes about six weeks
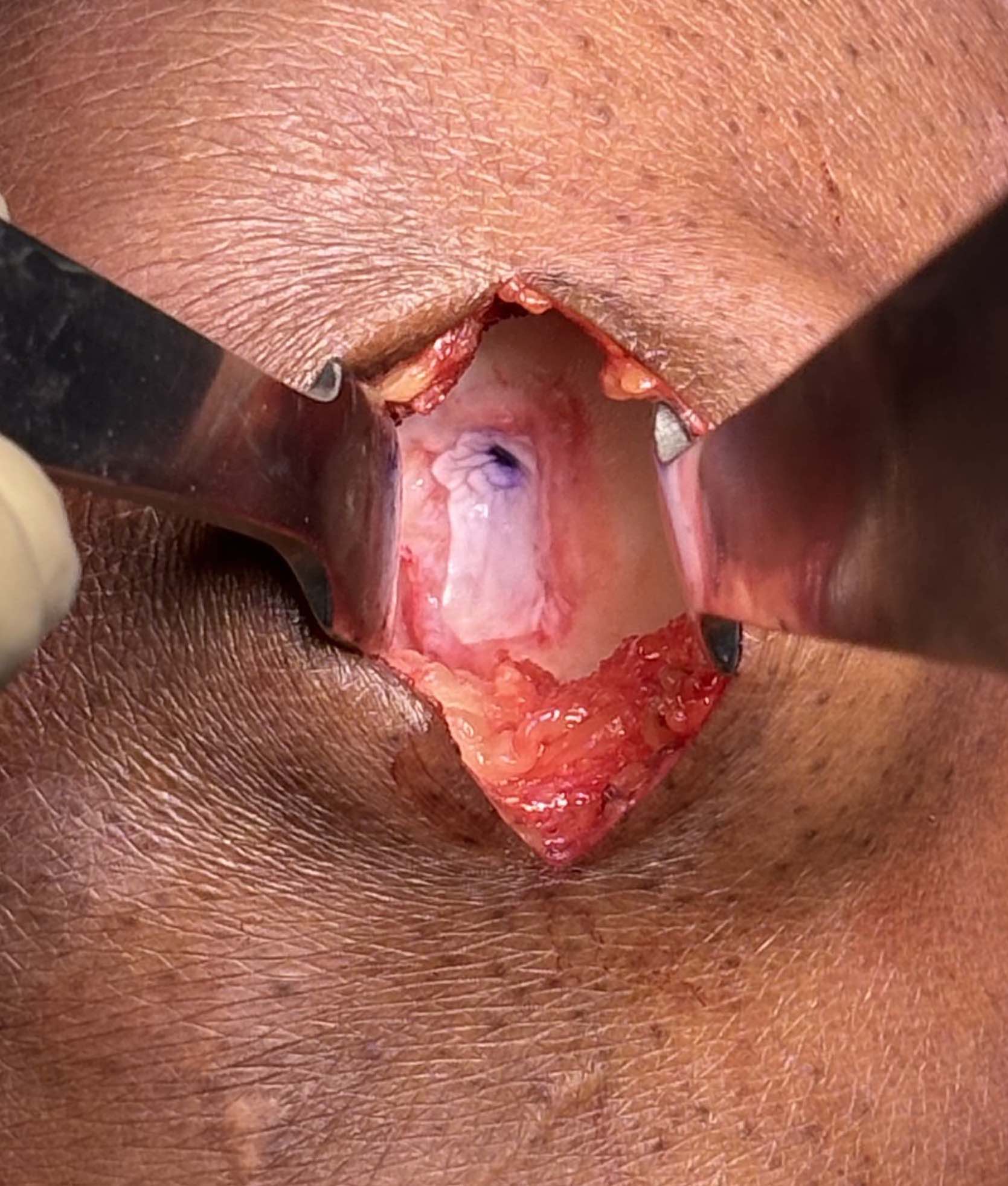
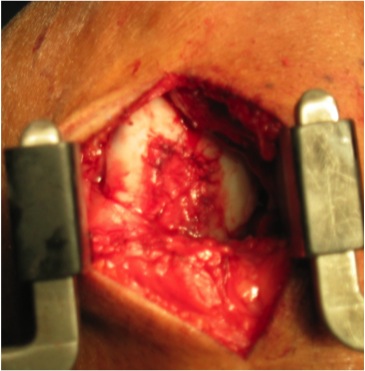
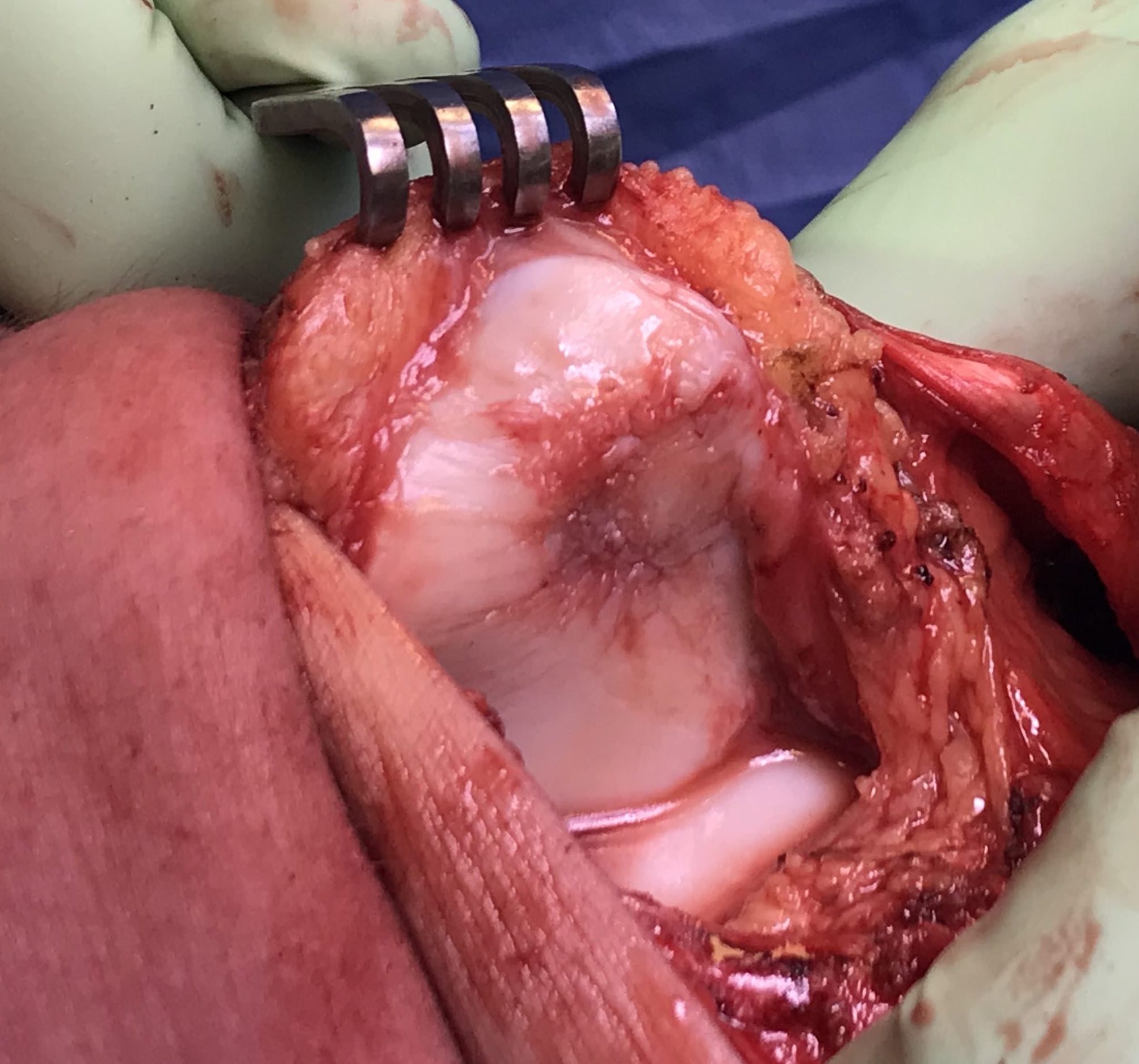
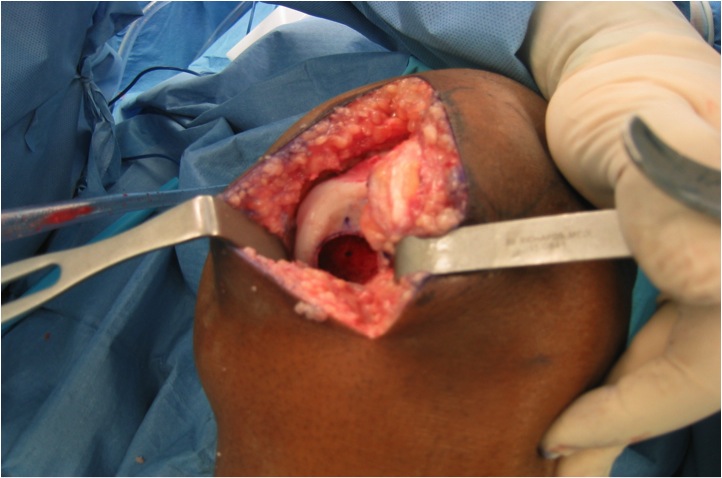
Implantation
- medial or lateral parapatellar approach
- create sharp stable margins
- curette base
- control bleeding with adrenalin soaked gauze to avoid graft displacement
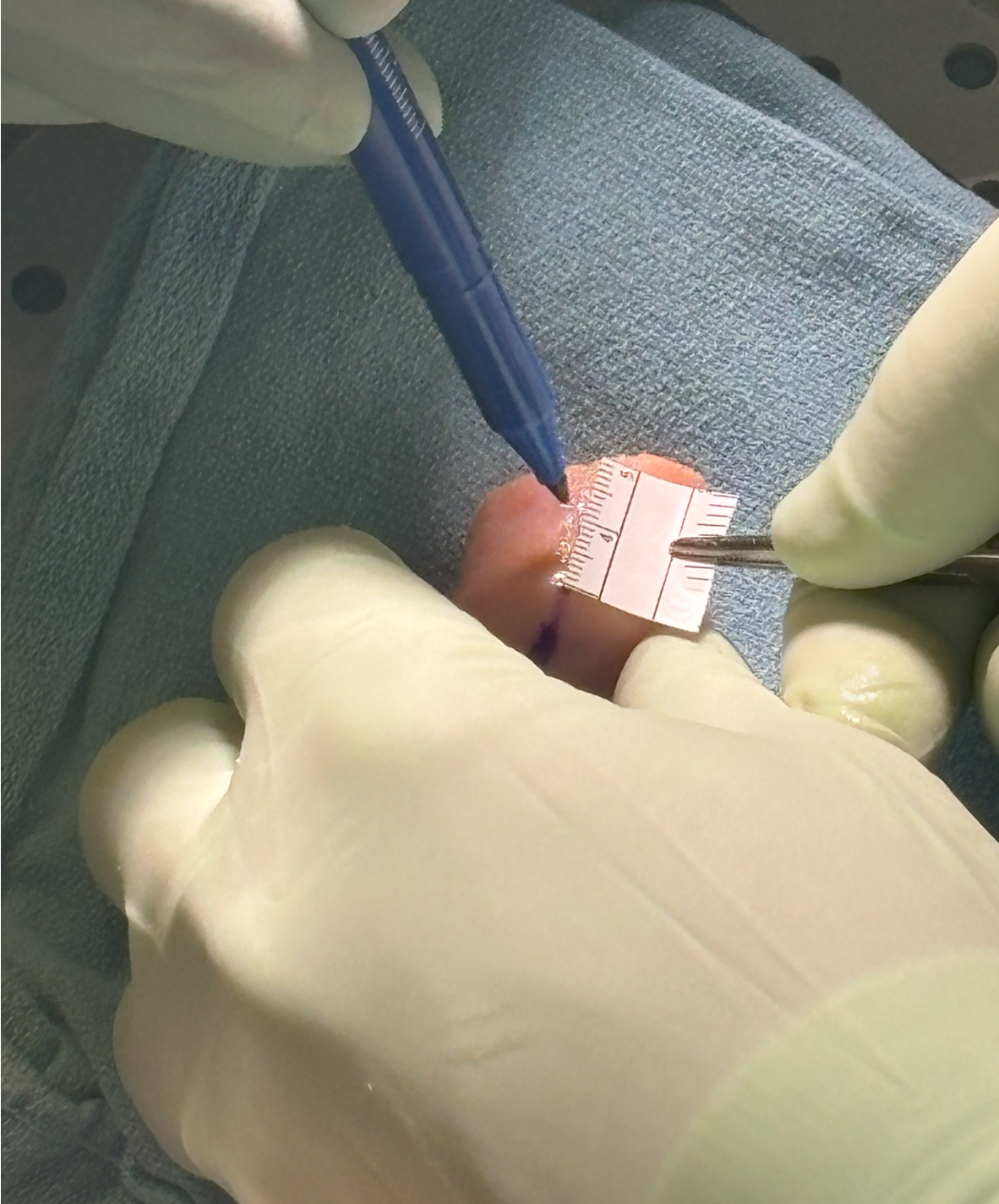
- size defect with foil - graft cannot be prominent or will displace with ROM
- secure with fibrin glue / Tisseal
- ensure graft stability with knee range of motion
Results
Dhillon et al Arthroscopy 2022
- systematic review of MACI v microfracture
- five level I and 1 level II studies
- 500 patients
- lower failure rate and better outcomes with MACI
- 5 year follow up of RCT of MACI v microfracture
- better outcomes with MACI at 5 years
- 10 year follow up of MACI
- 11% failure
- better outcomes with tibiofemoral graft than patellofemoral
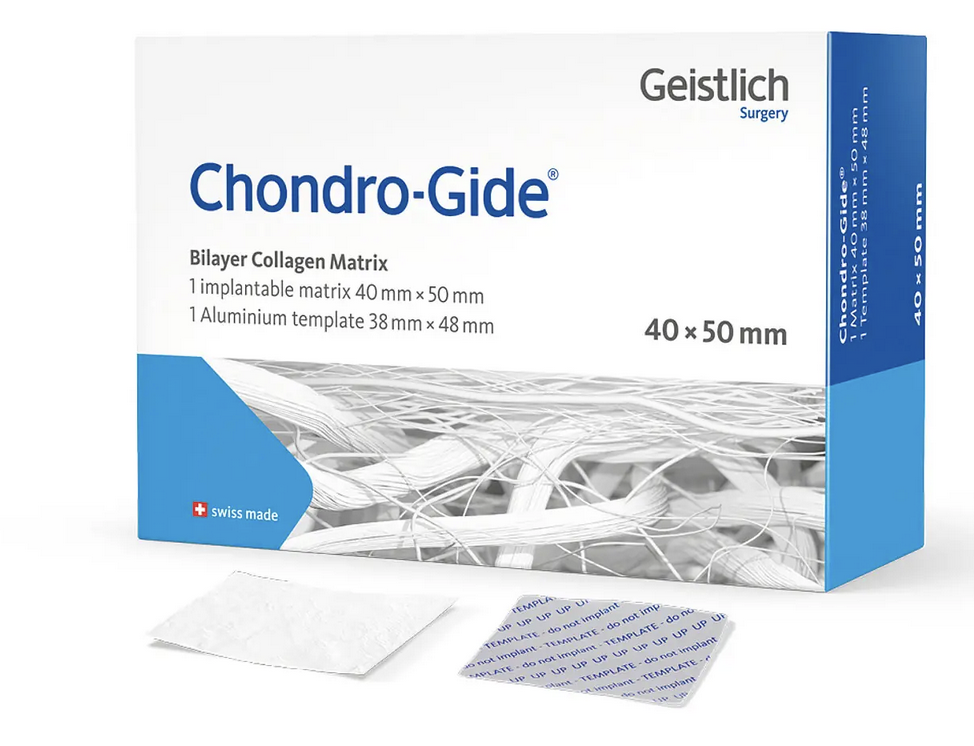
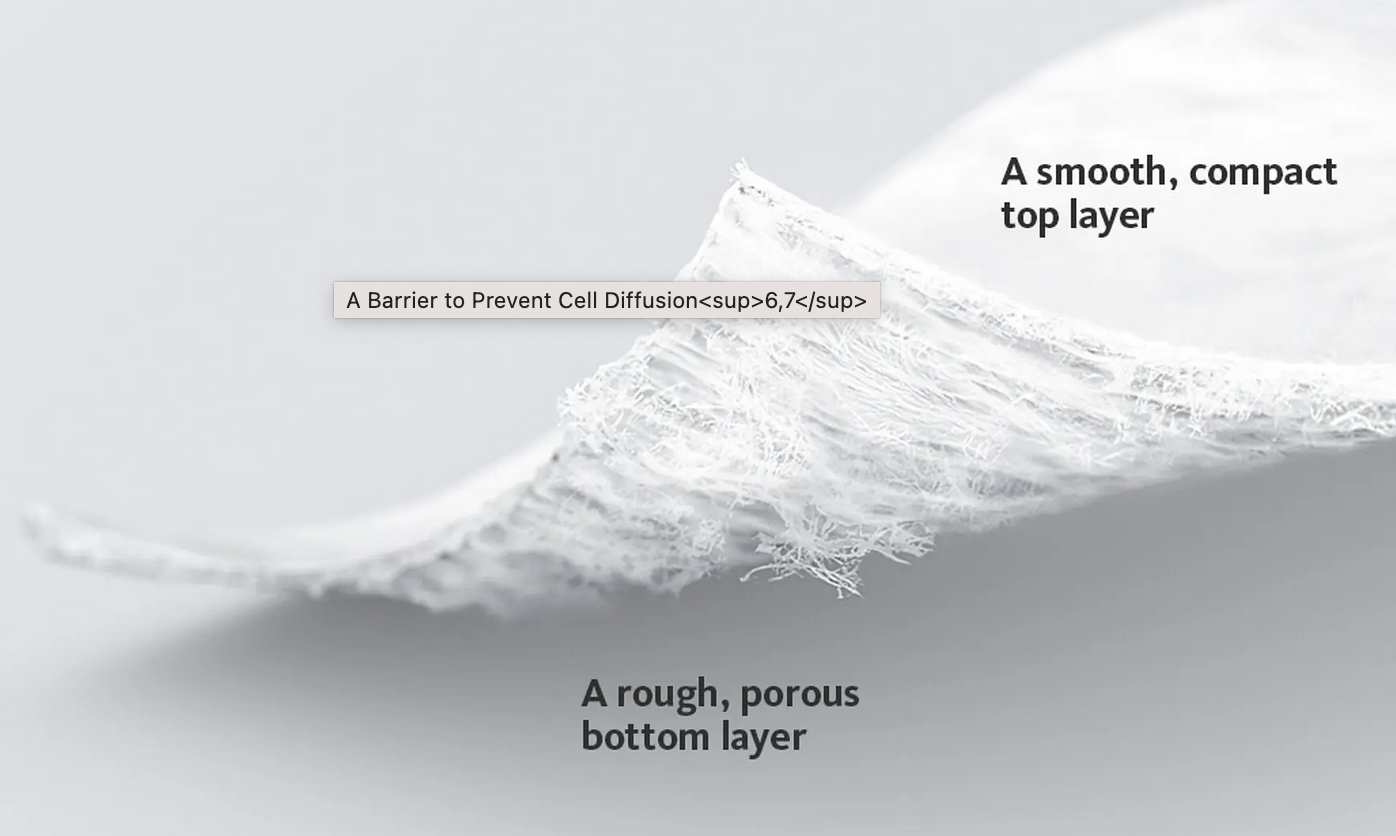
Autologous Membrane Induced Chondrogenesis (AMIC)
Principle
Addition of a Type I/III collagen membrane to microfracture
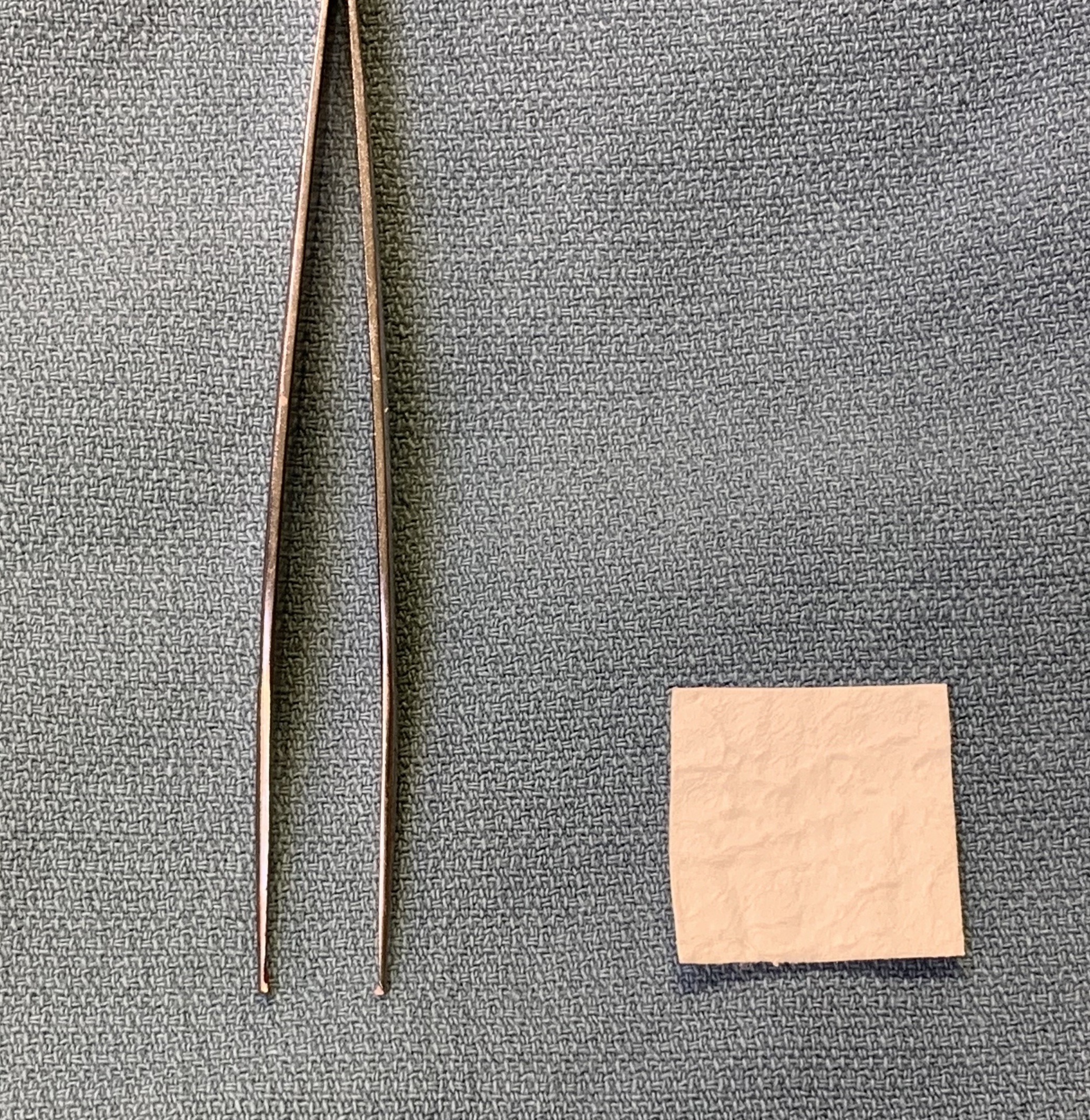

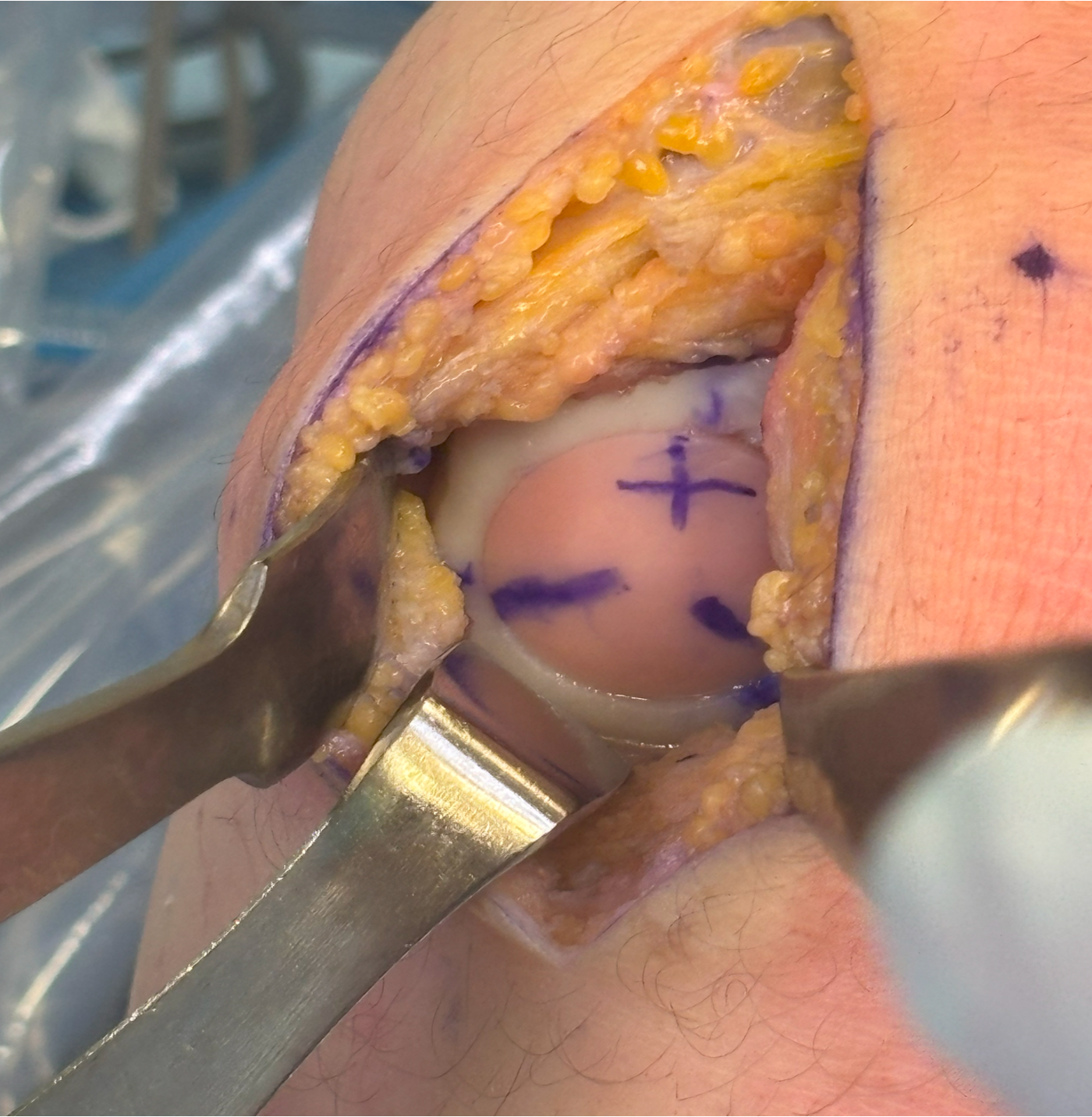
Technique

Medial or lateral parapatellar approach
- create sharp stable margins
- curette base / microdrill
- control bleeding with adrenalin soaked gauze to avoid graft displacement
- size defect with foil - graft cannot be prominent or will displace with ROM
- porcine collagen
- bilayer collagen I/III membrane
- secure with fibrin glue / Tisseel
- ensure graft stability with knee range of motion
Results

Volz et al Eur J Orthop Surg 2024
- 10 year follow up of RCT AMIC v microfracture
- results of microfracture deteriorated
- results of AMIC stable
Autologous Minced Cartilage Implantation (AutoCart)
Principle
Mechanical fragmentation of viable cartilage
- chondrocyte proliferation
- regeneration of hyaline cartilage
Technique
Vumedi autologous minced cartilage implantation video
Vumedi autologous minced cartilage video
Obtain cartilage from edge of lesion or non weight bearing areas
- intercondylar notch / periphery femoral trochlea
- can also use loose bodies / OCD lesions
- cut sharply with scapel to minimize bone death
- particles < 1 mm / have a paste like appearance
- secure with fibrin glue / Tisseel or membrane patch / Chondrogide
Results
- RCT of microfracture versus autologous minced cartilage
- 29 patients
- better outcome with autologous minced cartilage at 2 years
Allograft minced juvenile cartilage implantation (DeNovo)
Principle
Donor articular cartilage from patients < 13 years
- juvenile cartilage
- may have more favorable regenerative characteristics
Technique
Results
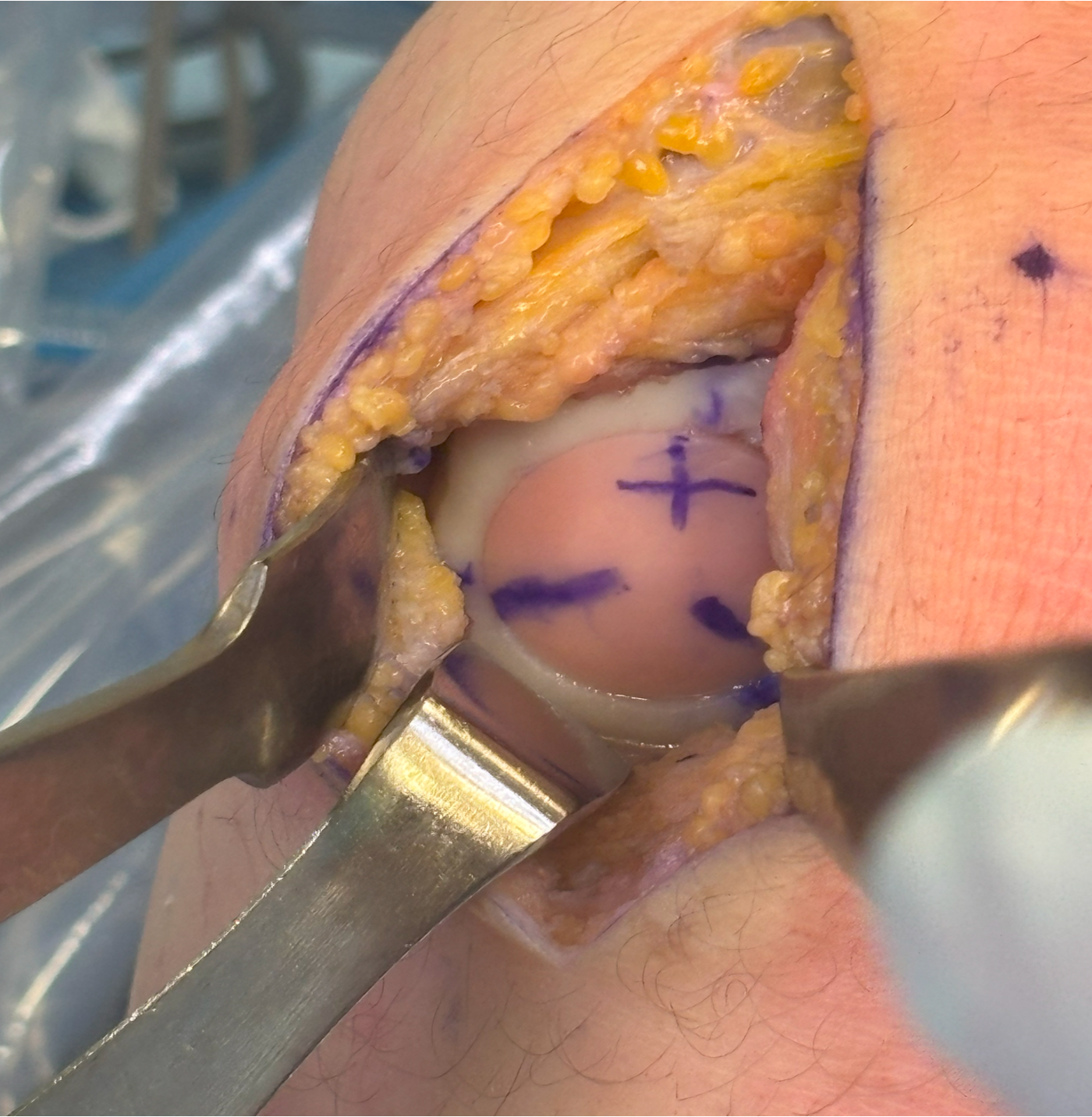
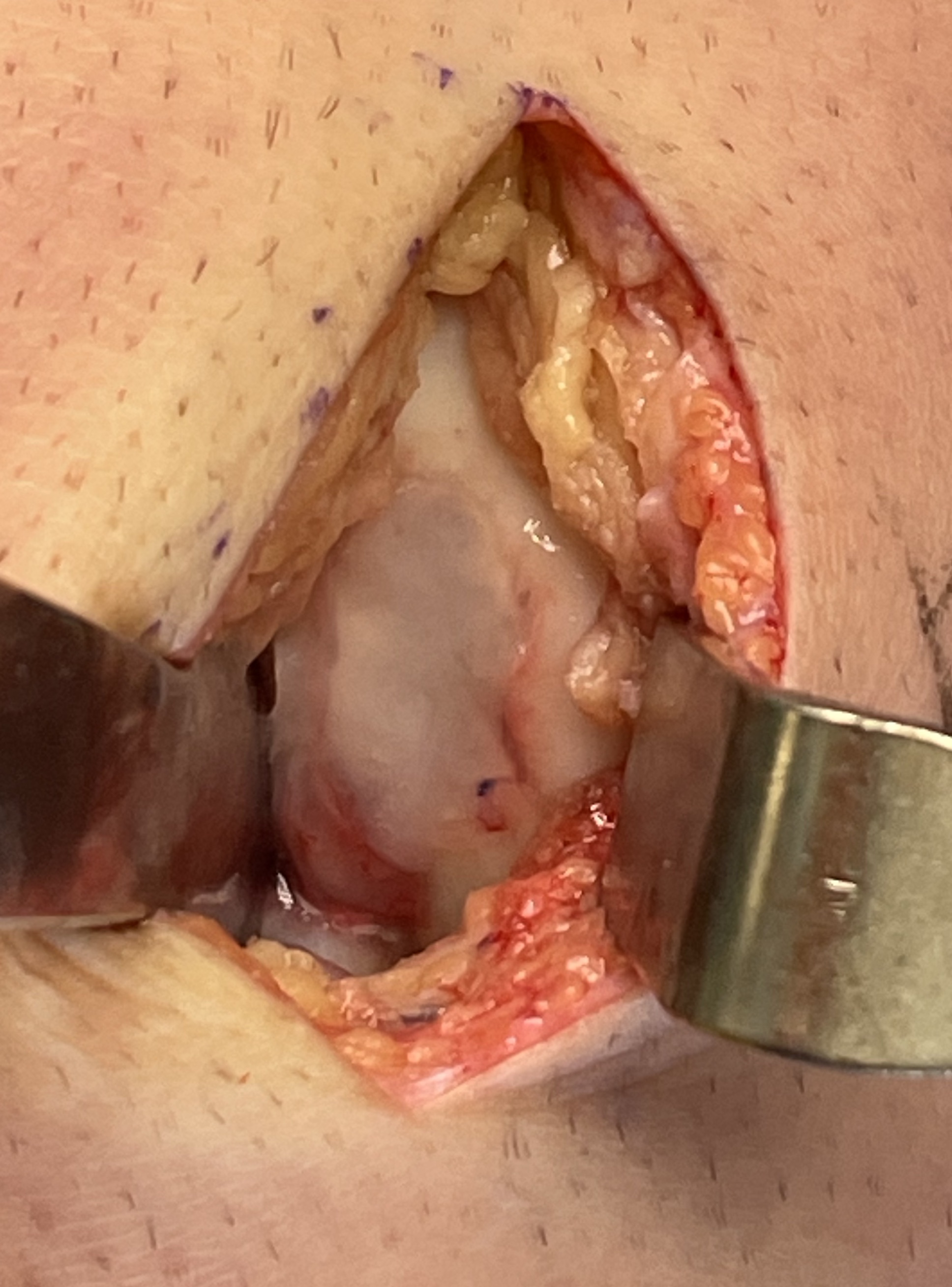
Osteochondral autograft transplantation / mosaicplasty
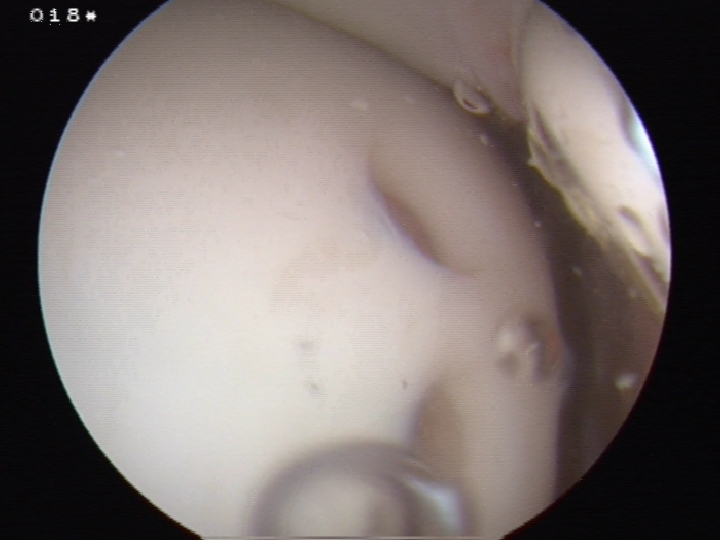

Principle
Autologous osteochondral bone plugs implanted in defect
- taken from low weight bearing areas of the knee
- can be associated with donor site morbidity
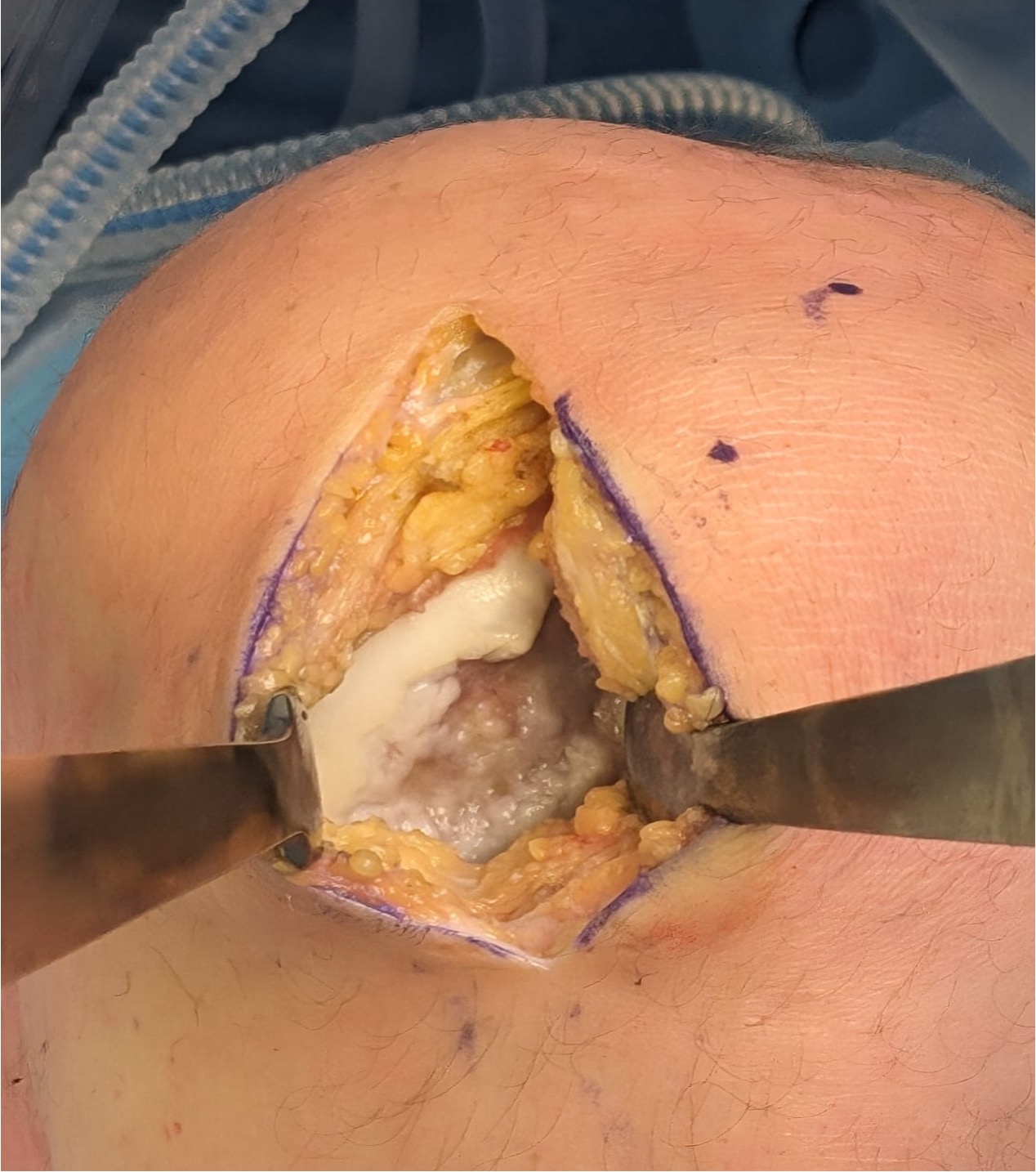
Technique
Debride all tissue from defect
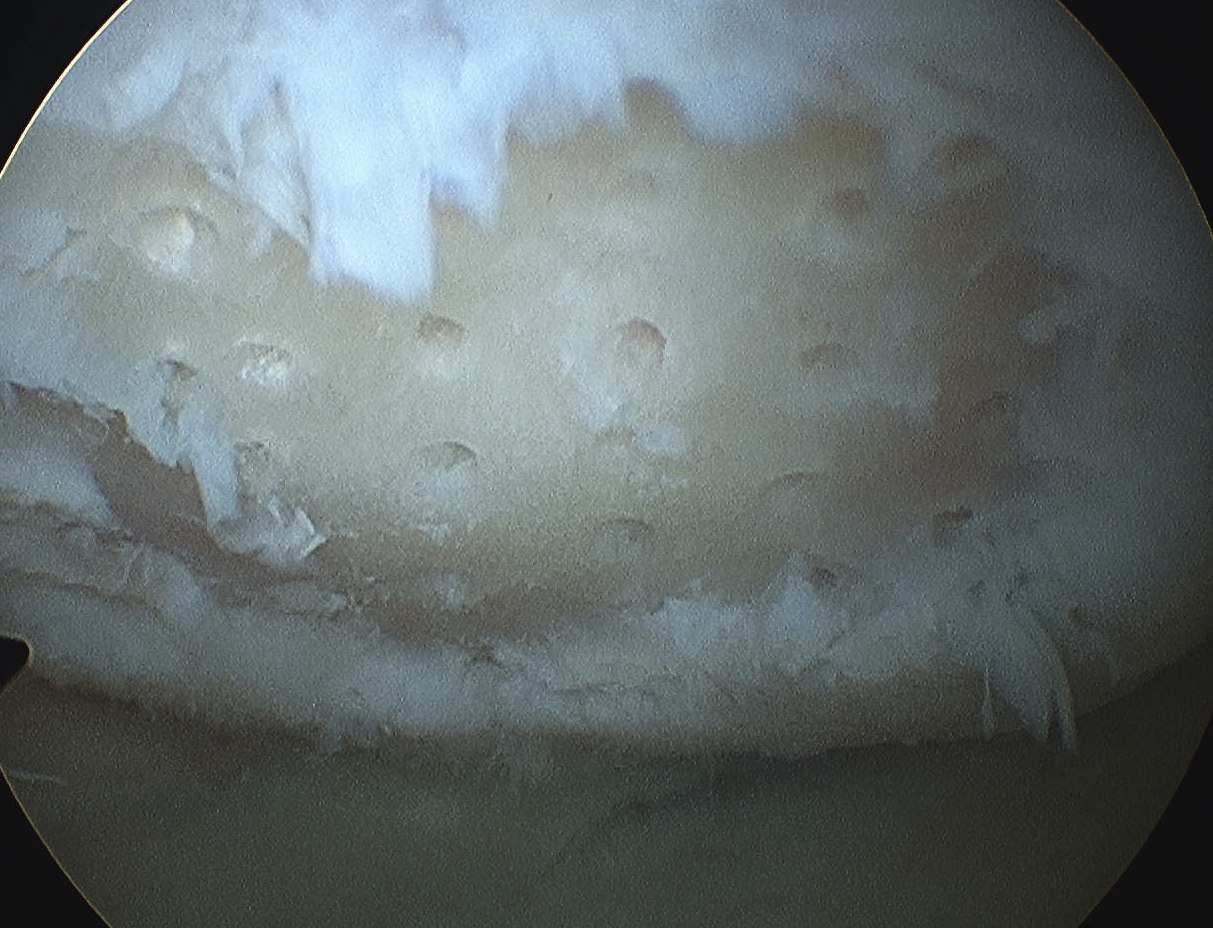
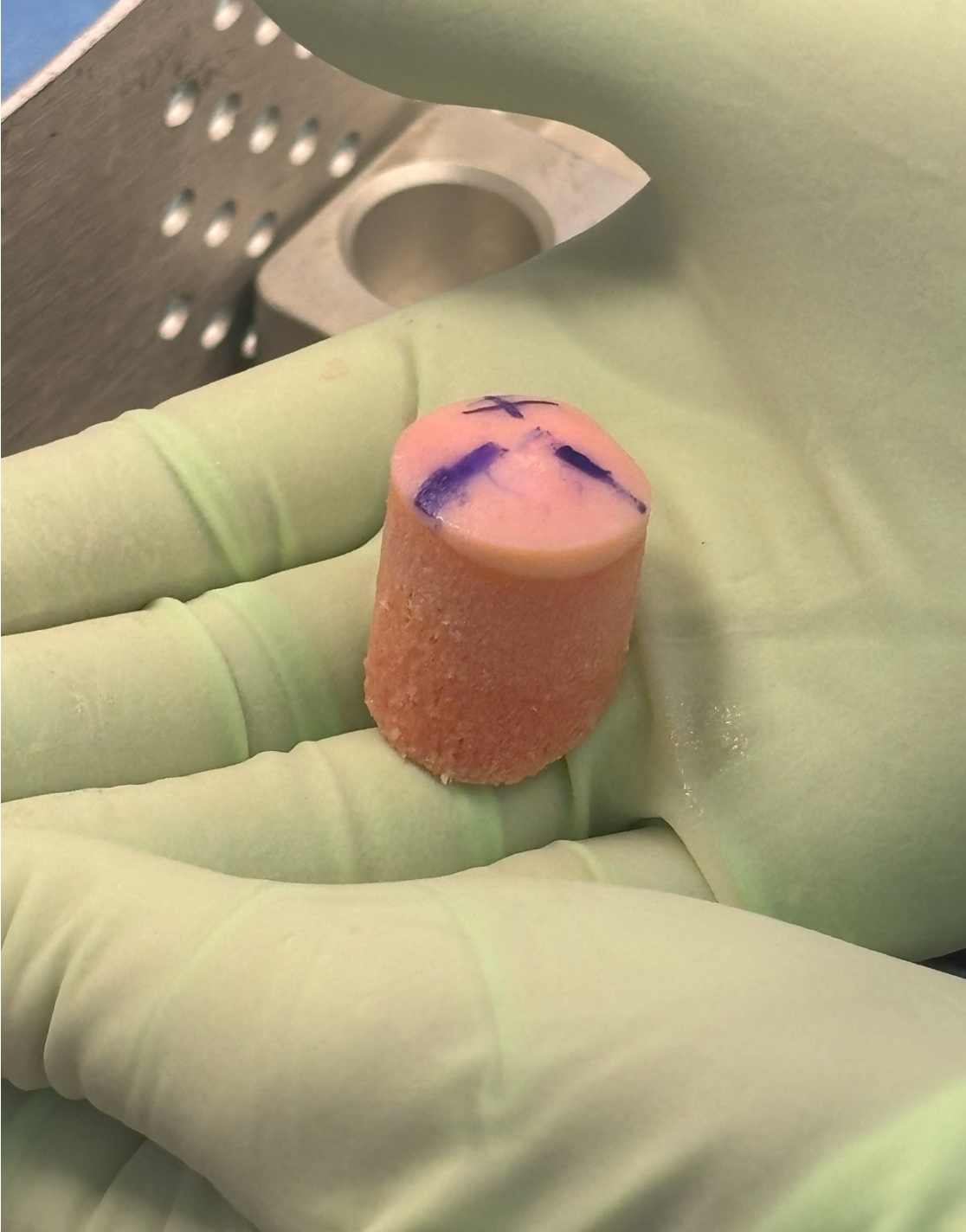
- obtain osteochondral plugs 4.5 mm
- periphery of femoral trochlea / notch
- create cylindrical holes with drill
- insert osteochondral plug
- small gaps between plugs
- ensure slightly recessed
Results
- systematic review of 6 studies comparing microfracture and osteochondral autograft
- better outcome scores and lower failure rates with osteochondral autograft and lesions > 3 cm2
Hangody et al Am J Sports Med 2010
- 354 patients followed up for average 9 years
- good results in 91% femur / 86% tibia / 74% PFJ lesions
- 5% of patients had PFJ pain from donor site
- RCT of OATS v microfracture of 60 young athletes
- 93% OATS and 50% microfracture returned to sport
- results maintained in 10 year follow up study
Osteochondral allograft


Principle
Indication
- very large, non contained defects
- previous failed cartilage procedures
Advantage
- restore anatomic contour
- nil donor site morbidity
- viable chondrocytes on fresh allograft < 30 days
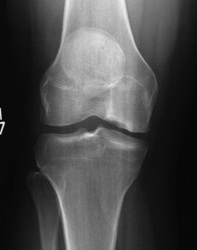

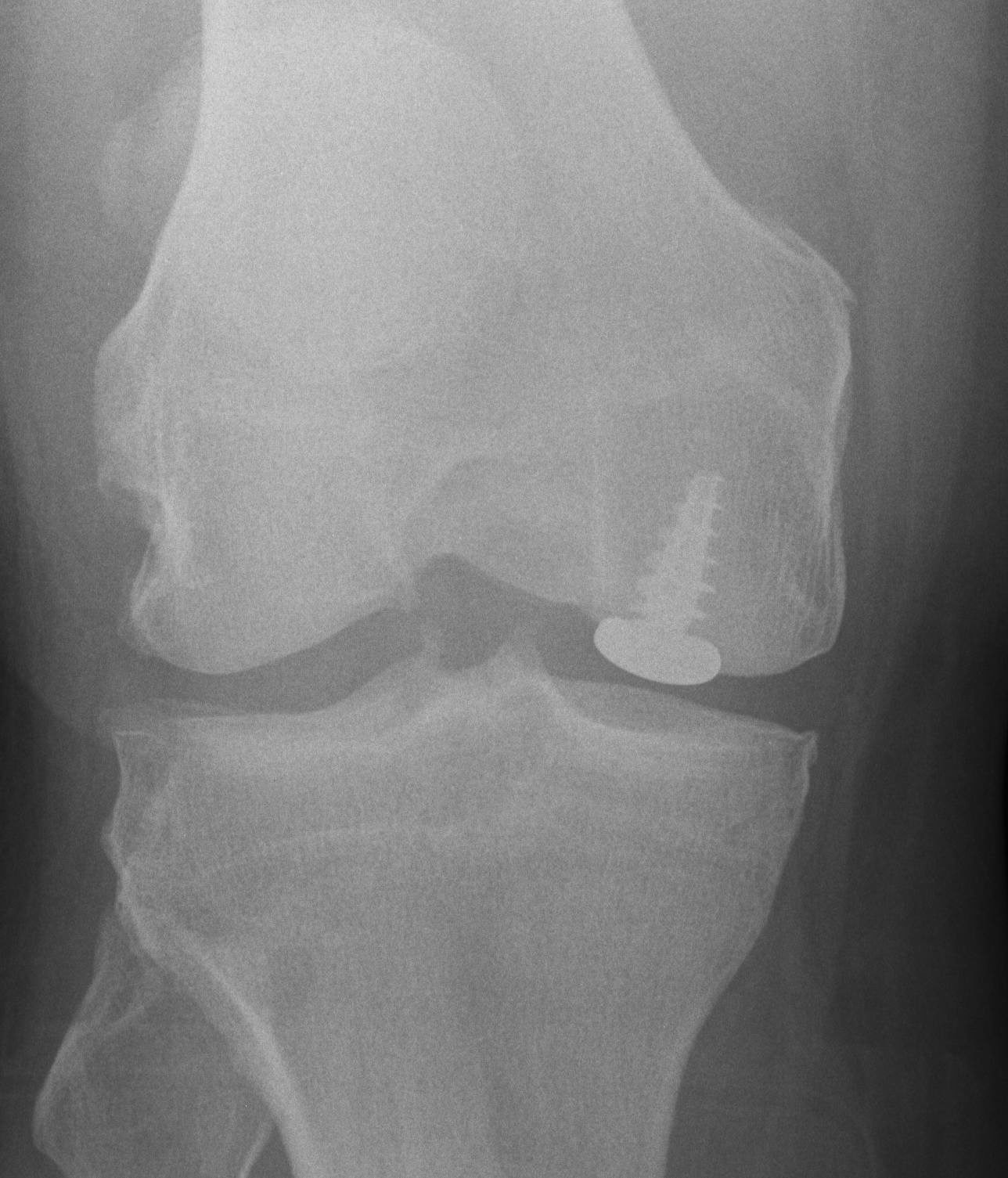
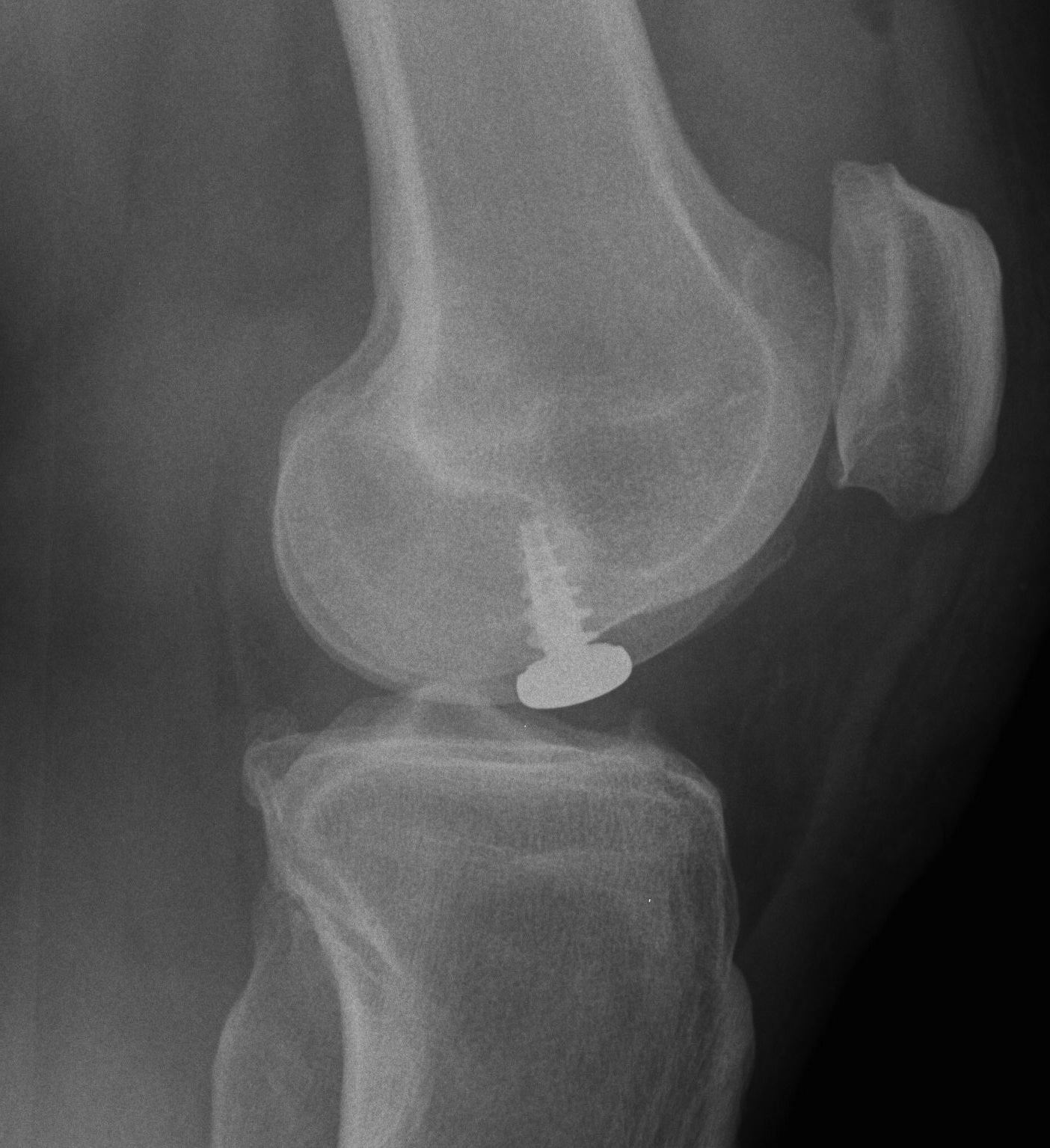
Pre and post OCA with HTO
Technique
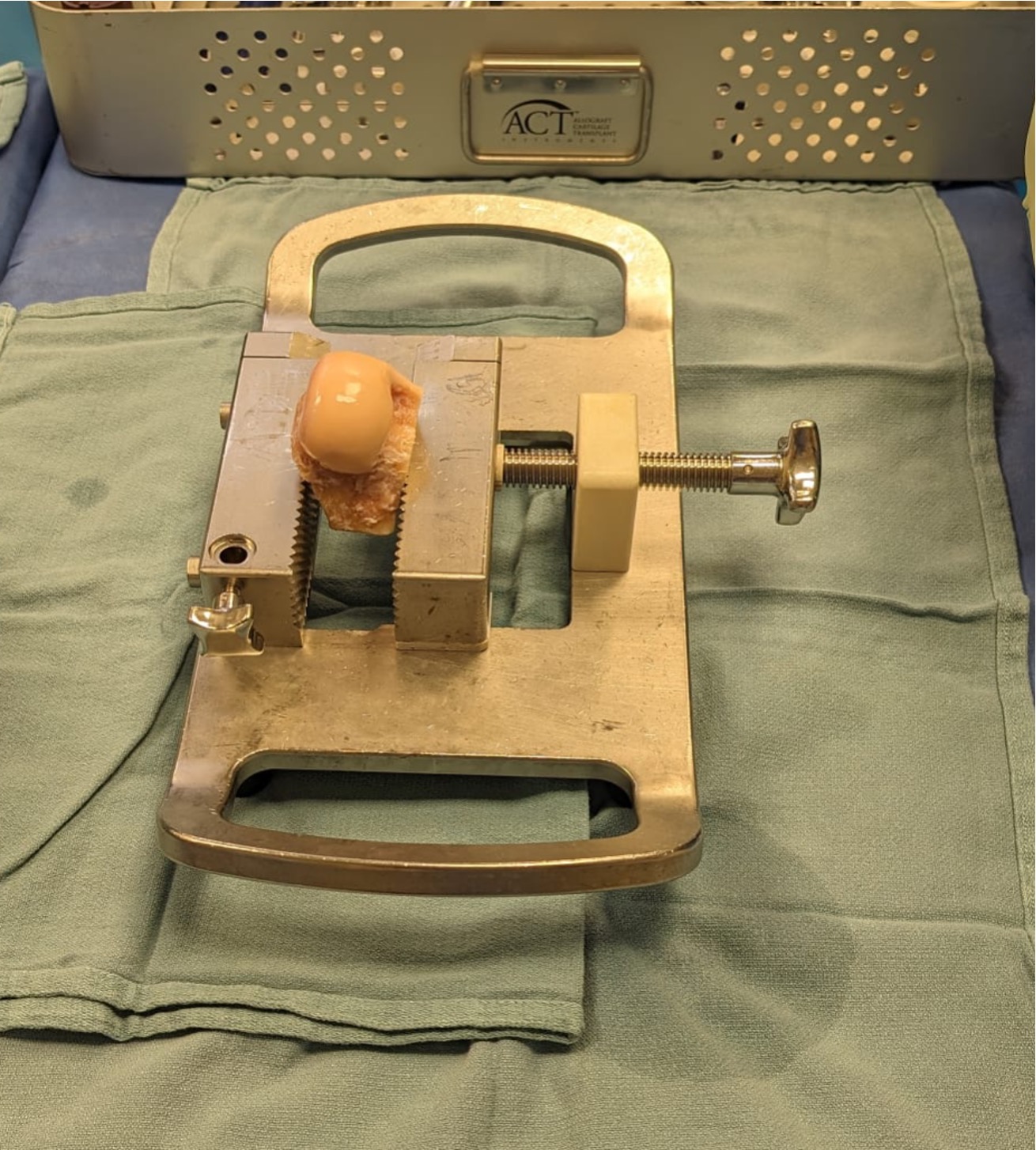
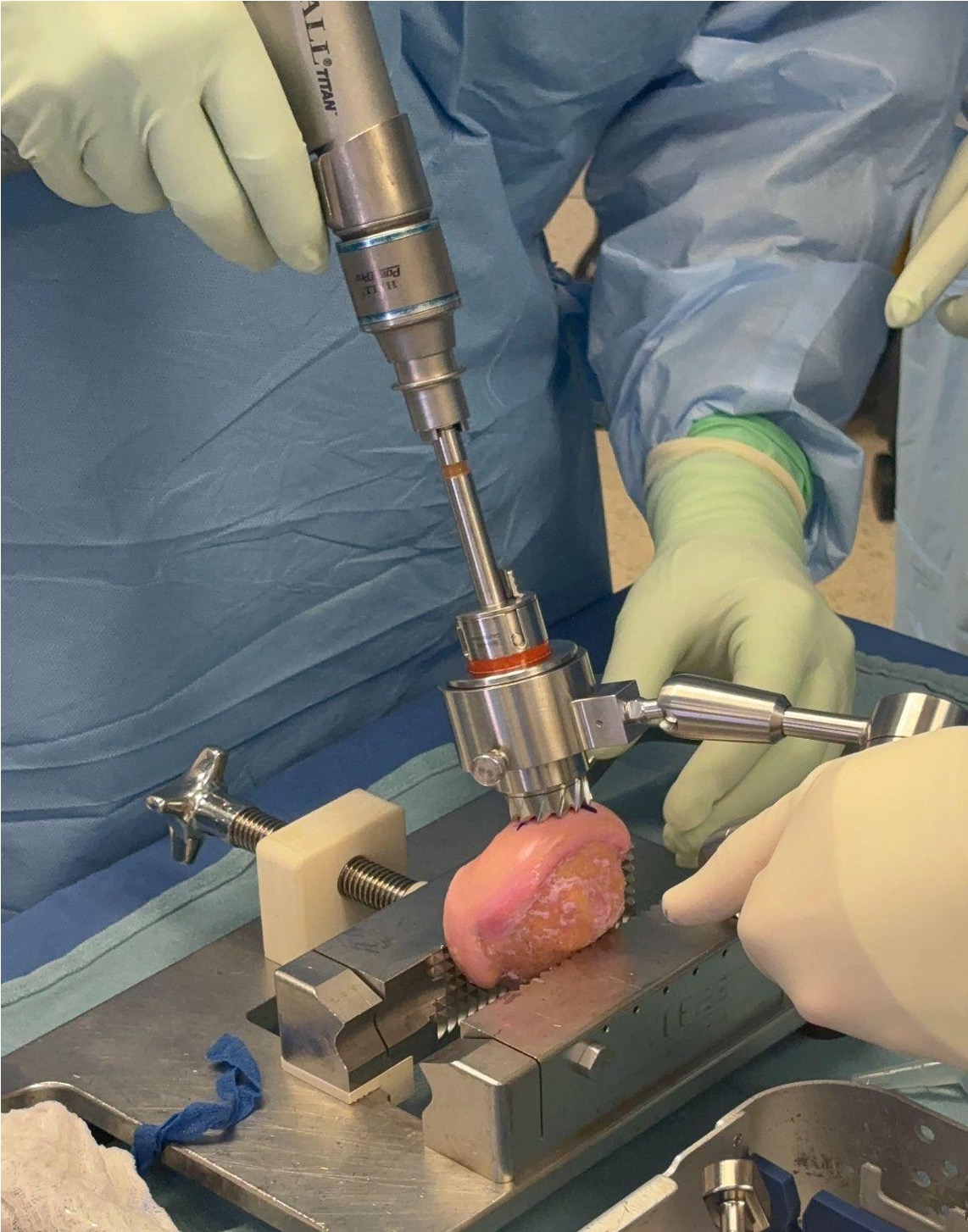
ConMed ACT Allograft technique video
Vumedi surgical technique video
Use CT to get appropriate size graft
Match curvature of radius of donor site
Press fit

Results
Wang et al Orthop J Sports Med 2023
- systematic review of OCA in 6000 patients
- mean lesion size 5 cm2
- failure rate 19%
- 83% satisfactory outcome
- survival rates at 5, 10, 15, 20, and 25 years were 94%, 87.9%, 80%, 73%, 55%, and 59.4%
Other options
Hemicap
