
Definition
Loss of ligamentous stability between atlas and axis
Can cause impingement of the spinal cord
Etiology
Down's syndrome - combination of ligamentous laxity, ondontoid dysplasia & os odontoid
Rheumatoid arthritis - attrition of transverse ligament and ondontoid erosion
Ligamentous laxity - Marfan's, Larsen's
Os odontoid - failure of fusion of odontoid
Congenital - SED, Achondroplasia, Morquio's syndrome, Klippel Feil
- 904 surgical cases
- os odontoid 429/904 (47%)
- atlas occipitalization 265/904 (29%)
- transverse ligament loose 84/904 (9%)
- rheumatoid arthritis 36/904 (4%)
- nonunion odontoid fracture 25/904 (3%)
- anklylosing spondylitis 11/904 (1%)
- Down syndrome 7/904 (1%)
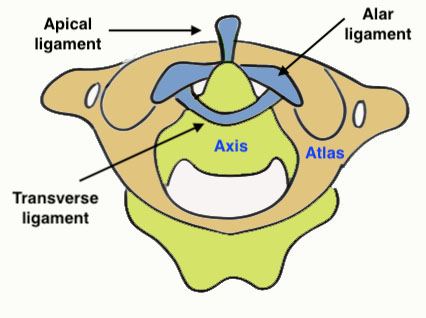
Anatomy
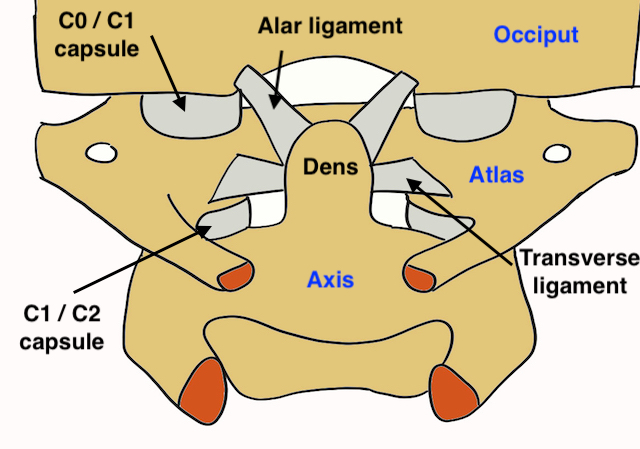
Bony
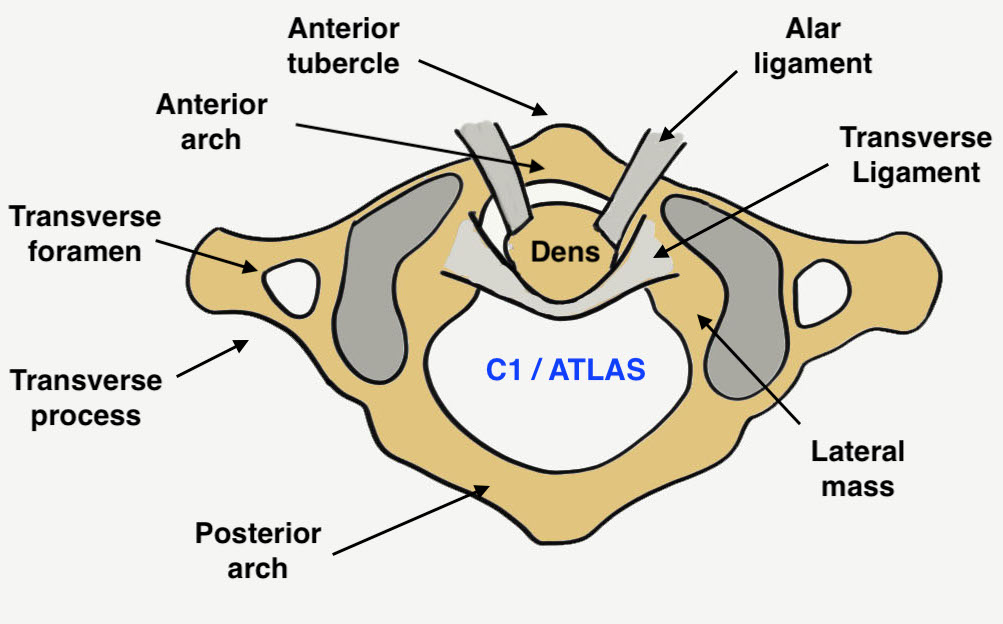
Atlas - ring of anterior and posterior arches with lateral mass
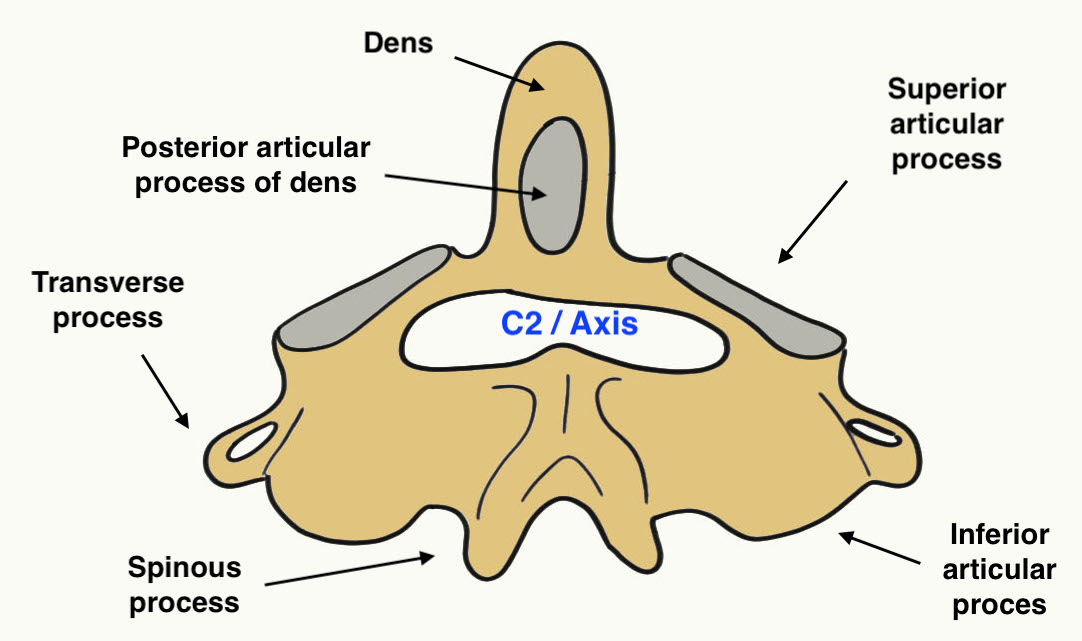
Axis - odontoid, vertebral body, and articular facets
Ligaments
| Structure | Attachments | Action |
| Cruciform ligament | Transverse ligament - tubercles medial aspect lateral mass C1 | Prevents anterior displacement of atlas |
| Longitudinal bands - from transverse ligament
up to occiput and down to C2 |
|
|
| Alar ligament | Side of the dens up to the lateral margins foramen magnum | Prevent excessive rotation |
| Apical ligament | Tip of dens to anterior foramen magnum | |
| Tectorial membrane |
Extension of PLL behind transverse and alar ligaments |
Mechanism
C1/C2 - 50% of rotation of the cervical spine
Symptoms
Neck pain
Neurological symptoms
Signs
Myelopathy
- abnormal gait
- hyper-reflexia
Boneschool / myelopathy examination
Xray
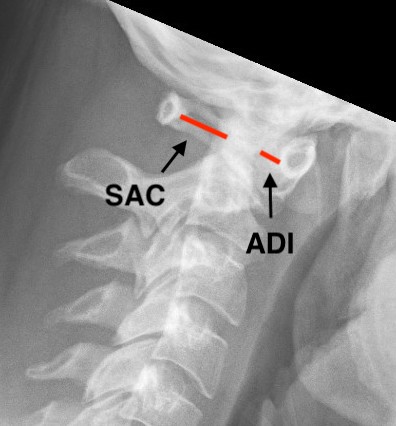
Atlanto-dens interval (ADI)
- > 5 mm indicates instability
Space available for Cord (SAC)
- posterior atlanto-dens interval (PADI)
- < 13 mm concerning

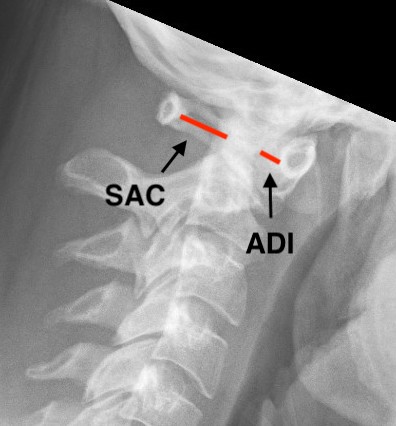
Increased ADI in patient with Down's syndrome
Flexion / Extension views


Down's syndrome flexion xray Down's syndrome extension xray
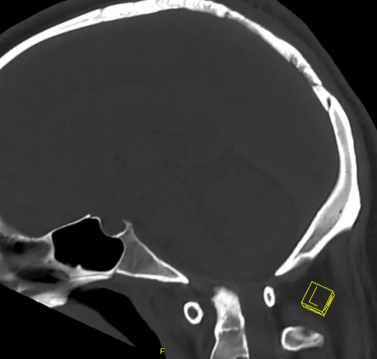
CT
MRI
Assess transverse ligament
Assess space available for cord (SAC)
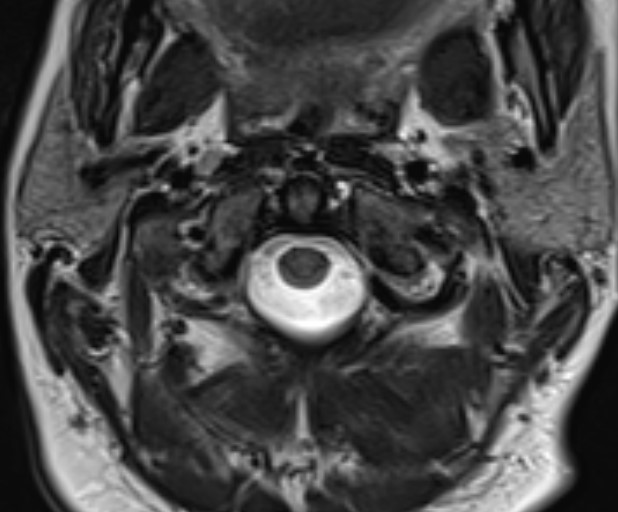
Intact transverse ligament on MRI
Classification
Wang classification Spine 2013
904 cases
| Type I | Instability | Reduced on flexion or extension xray | 472 (52%) | Reduce and posterior fusion |
| Type II | Reducible dislocation |
No bony fusion on CT Reducible under GA with skeletal traction |
160 (18%) | Reduce and posterior fusion |
| Type III | Irreducible dislocation |
No bony fusion on CT Not reducible under GA with skeletal traction |
268 (30%) |
Trans-oral anterior release Posterior fusion |
| Type IV | Bony dislocation | C1/C2 bony fusion on CT | 4 (<0.5%) |
Trans-oral anterior osseous decompression Posterior fusion |
Criteria for diagnosis of AAI
1. ADI > 5 mm
2. Overriding of the anterior arch of the atlas over the odontoid
3. Space available for the cord (SAC) of less than 13 mm
4. Violation of the Steel’s rule of thirds (one-third cord, one-third odontoid, and one-third safe space)
5. Translation of the tip of the odontoid of more than 4 mm of the basion
Surgical technique
Reduction
- cranial traction with Gardner-Wells tongs
- GA and muscle paralysis
- gradual increased in traction weight up to maximum 1/6 patient body weight
- fluoroscopic assessment after 10 minutes
Type I / II
- anatomic reduction with skeletal traction
- posterior fusion
- transarticular C1/C2 (Mageryl)
- C1 lateral mass / C2 pedicle screw (Goel and Harms)
- occasional occiput - C2 fusion
Type III
- irreducible with skeletal traction
- trans oral release / facet joint release
- posterior fusion
Type IV
- bony fusion on CT
- anterior release +/- trans oral odontoidectomy
- posterior fusion
Results
- 904 cases of AAI treated surgically
- anatomic reduction in 99%
- 99% solid fusion
- neurological improvement in 84.1% (512/609) of the patients with myelopathy.
- 2 vertebral artery injuries with trans-oral approach (1 death)
- 4 vertebral artery injuries with posterior approach
- 1 death from PE
- 3 deaths from respiratory distress
Down's Syndrome
Incidence
- up to 60% develop AAI
- 1% neurological symptoms and signs
Definition
Bouchard et al Spine Deform 2019
- ADI > 6mm
- SAC < 14 mm
Natural history
- 91 Down's syndrome children with AAI > 4 mm
- half randomly allowed to play sport, half restricted
- at one year, no difference in neurological outcomes
Management guidelines
ADI > 5mm & asymptomatic: ?avoid contact sports
ADI > 5mm & symptomatic: fusion
ADI > 10 mm: C1/C2 fusion
Tomlinson et al Clin J Sports Med 2020
- screen for myelopathy
- ensure good neck control / encourage regular neck strengthening
- ensure good neck ROM
- allow to play sports if above 3 categories met
- monitor for any neurological symptoms
Rheumatoid Arthritis
Cause
- transverse ligament incompetent
- bony erosions
Os Odontoid
