Incidence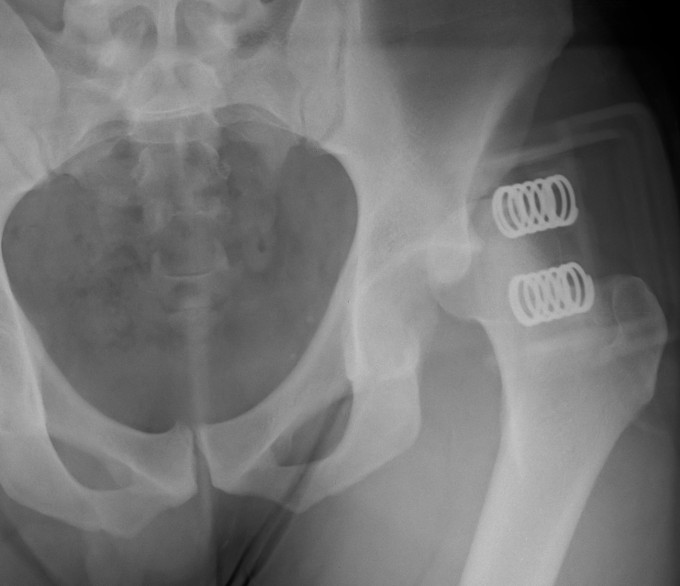
Young men
Posterior / Anterior 9:1
Aetiology
High velocity injury
- head direction at impact decides direction of dislocation
Anterior Dislocation
Externally rotated & abducted leg
- flexion = inferior dislocation
- extension = pubic dislocation
Posterior Dislocation
Axial compression of adducted leg
- more flexion causes pure dislocation without fracture
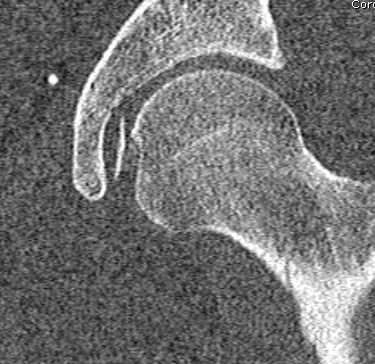
Anatomy
Inherently stable joint
- large head on smaller neck
- allows deep seating of femoral head
- acetabulum deepened by labrum
- capsule reinforced by ilio/pubo/ischio femoral ligaments
40% femoral head in contact with articular cartilage
10% in contact with labrum
Blood supply
Majority by deep branch of Medial Circumflex Femoral Artery
- minimal by medial epiphyseal artery via ligamentum teres
- little to non via LCFA
MCFA
- arises medial aspect of profunda
- along posterior intertrochanteric crest extracapsular / back of femoral neck
- passes between iliopsoas and pectineus medially
- runs along inferior border of obturator externus, above adductor brevis
- deep to quadratus femoris
- emerges between quadratus and inferior gemellus
- runs over conjoint tendon (2 gemelli and obturator internus)
- then penetrates capsule between conjoint and piriformis
- runs along superior aspect of neck to femoral head
Transverse branch (to ischium) and ascending branch (to trochanteric fossa0
- arise anterior to quadratus
Must protect this deep branch MCFA in a posterior approach
With dislocation and capsular tears
- some ascending cervical branches stretched/kinked
- emergent reduction can improve blood flow to femoral head
Associated Injuries
50-95% have other injury
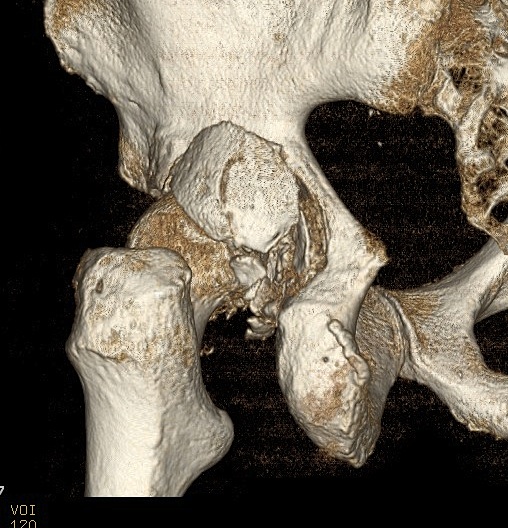
Acetabular fracture
Femoral head fracture / Pipkin fracture
Sciatic nerve 10% / posterior dislocation
Patella fracture
PCL
Femoral artery injury - anterior dislocation
Femoral shaft fracture
- reduce head via steinman pin in proximal fragment
- then IMN femur
Classification
Direction
1. Medial / Central
- really medial displacement with acetabular fracture
2. Anterior
- pubic / obturator / perineal
3. Posterior
Pathoanatomy
Capsule & Ligamentum teres torn
Labral tears & muscular injuries also occur
Y / iliofemoral ligament often intact with posterior dislocation
- blocks reduction
- bony fragments also block reduction
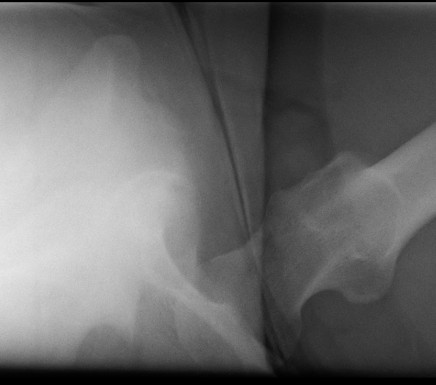
Clinical Features / Xray
Posterior dislocation
- leg shortened, flexed, adducted & internally rotated
- head small on xray
Anterior dislocation
- leg short and externally rotated
- head larger on xray
Check NV status / sciatic nerve

Management
Immediate
Assess & manage life threatening injuries
- EMST / ATLS principles
Principles
1. Emergent reduction
- closed +/- open
- reduce risk AVN
AVN
- < 6 hours 10%
- 20% - 50% if >24 hours
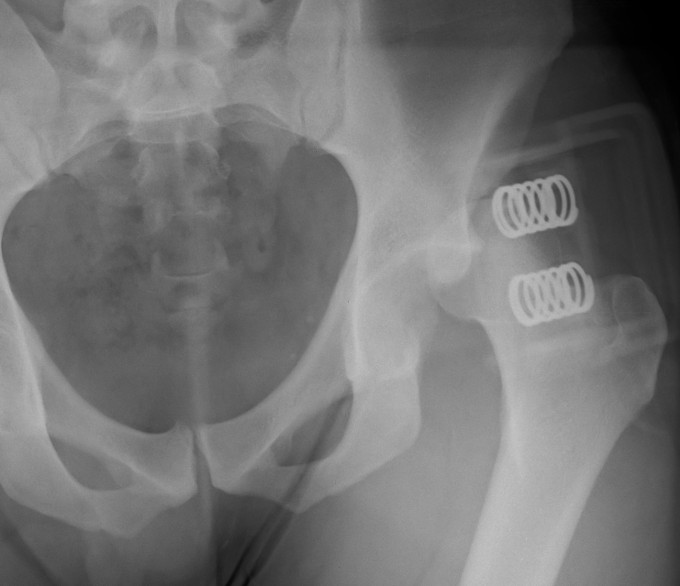
2. Assess stability
Posterior wall fracture > 40%
- need ORIF for stability

Posterior wall fracture < 40%
- can be unstable
- EUA after reduction to assess stability
- should be able to flex to 90o and some IR without instability
3. Screen for retained fragments
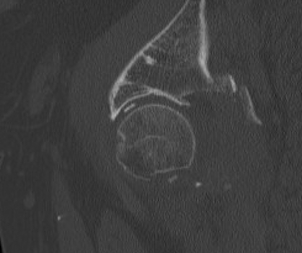
Compulsory CT
- xray will not detect fragments < 2mm
Remove / ORIF depending on size of fragment and location / Pipkin type
4. Reconstruct acetabulum if unstable or incongruent
Closed Reduction Posterior Dislocation
Technique
Full muscle paralysis on radiolucent table
- supine
- assistant places downward pressure on ASIS
- operator up on bed grasping leg
- flex hip to 90o, flex knee to 90o
Technique
- ER head around acetabulum / axial traction or
- IR head around acetabulum / axial traction
Post reduction
- check concentric reduction on II
- check stability in flexion
Unstable reduction
- skeletal traction / femoral steinman pin
Post op
NV examination when patient awake
- ensure sciatic nerve working
- ensure hasn't become entrapped with reduction
CT
Closed Reduction Anterior Dislocation
Technique
- as above
- traction in line with femur flexed
- internal rotation maneuver
Irreducible Dislocations
Incidence
- 2-15%
Causes
1. Capsule / Labrum / Ligamentum teres
2. Muscle interposition
- anterior usually rectus / psoas
- posterior usually piriformis / G maximus
3. Bone fragment
4. Muscle tone
- patient requires relaxant
Management
Open reduction
Non-concentric Reduction
Esssential to obtain X-ray and CT after reduction
X-ray
- head - teardrop distance must equal contralateral side
CT
- only with CT can < 2mm fragments be seen
MRI
- may be needed to see labral tears blocking reduction
Open reduction
Indications
1. Irreducible dislocation
2. Non-concentric reduction
- loose bodies / interposed tissue
3. Post operative sciatic nerve palsy
4. Unstable posterior acetabular fracture
5. Associated NOF fracture
6. ORIF Pipkin fracture
Approach
Usually from direction of dislocation
- preserve intact capsule
- preserve remaining blood supply
- i.e. with posterior dislocation the posterior capsule will be torn
- provides entry into joint
Posterior Approach
Aim to preserve intact anterior capsule and blood supply
- beware sciatic nerve
- divide piriformis and conjoint tendon away from insertion to preserve deep branch MCFA
- may need to extend posterior capsular rent
- allows direct visualisation of blocks to reduction
- blocks include G. max, piriformis, capsule, bony fragments
- may need to excise ligamentum teres
- explore acetabulum for loose bodies
- close capsule afterwards
- may need to excise L Teres
Other issues
Posterior acetabular fracture
- ORIF if > 40% or unstable
Pipkin fracture
- manage as per Femoral Head Fractures
Subcapital fracture
- Watson Jones / Smith Peterson approach
- supplementary lateral approach to insert fixation
Post Operative
NWB for 6/52
Bone scan re vascularity
Issue
- °AVN = FWB
- AVN = consider bisphosphonates
Yue et al J Orthop Trauma 2001
- 5/54 low blood flow on early SPECT
- no correlation with AVN
Complications
AVN
Related to
- time to reduction <12/24
- velocity of injury
- open reduction vs closed (x4)
- direction (anterior < posterior)
Timing
- < 6/24 = 2-10%
- > 12/24 = 52%
Direction
- posterior 17%
- anterior 2%
Tends to be localised
- revascularisation occurs on reduction
- damage to lateral & medial epiphyseal artery
- metaphyseal blood supply remains
- occurs in first 18 months
OA
Incidence
- 15 - 20 %
Causes
- AVN
- instability
- incongruous reduction
- cartilage damage at time of dislocation
Philippon et al Arthroscopy 2009
- hip arthroscopy post traumatic dislocation in 14 athletes
- all had chondral defects, 11 had loose fragments
- all patients had labral tears
Sciatic Nerve Palsy
Posterior dislocation
- 8 - 19%
- more common after fracture / dislocation
Type
- usually partial CPN
- usually resolves
Only explore if onset after MUA
Else observe
Instability < 1%
Myostitis Ossificans
Uncommon
- usually little functional problem
