Incidence
5-15% of posterior dislocations
Aetiology
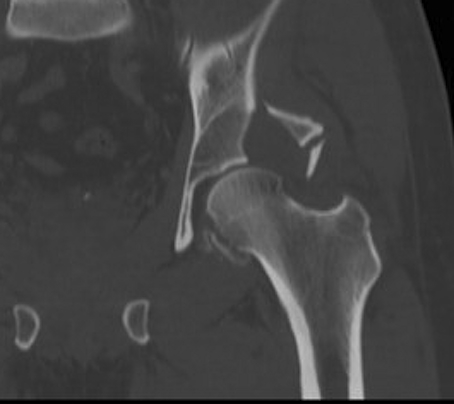
Posterior hip dislocation
Pipkin Classification
Type I - head fracture below fovea
Undisplaced
- non operative
Displaced
- excise fragment if small
- ORIF fragment if large (can contribute to instability)
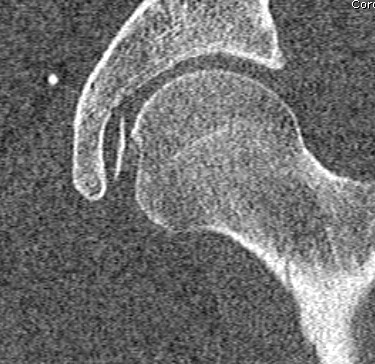
Type II - head fracture above fovea
Undisplaced
- rare, usually unstable
Displaced
- excise if small
- ORIF if large
Type III - Type I/II with NOF fracture
Issue
- very high incidence of AVN
Mangement
- ORIF young patient
- hemiarthroplasty / THR older patient

Type IV - Type I/II/III associated with acetabular fracture
Non operative management
Indications
Type 1
- < 2mm displacement
- stable hip
- congruent joint
Type 2
- rarely anatomic
- usually unstable
Surgical Management
Choice of Approach
Fragment usually anteromedial
Type 1 and II
- anterior or anterolateral approach
- Smith Petersen / Watson Jones
- careful capsulotomy to preserve blood supply
- deep branch MCFA runs along superior femoral neck




Type III
- anterolateral approach / Watson Jones
- ORIF NOF + fix/excise Pipkin fracture in young patient
- very high incidence AVN
- THR > 60
Type IV
A. Associated with posterior dislocation / non operative acetabular fracture
Posterior approach
- this can make it difficult to access fragment
- need IR +++
- can attempt posterior to anterior screw fixation
Anterior approach
- if stable and no acetabular fracture requring ORIF
- involves making anterior capsulotomy
- patient already has posterior capsular defect
B. Associated with posterior acetabular wall fracture that needs ORIF (>40%)
- posterior approach
C. Associated with anterior acetabular fracture
- ilioinguinal with SP extension
Anterior Approaches
Many options
- Hardinge
- Watson Jones
- Smith Peterson
- Ganz osteotomy
Any of these are blood supply preserving if perform safe capsulotomy
- avoid capsulotomy along superior neck
- Z capsulotomy
- capsulotomy along anterior acetabular rim superior to inferior
- along inferior femoral neck
- down medial femur
Ganz trochanteric flip osteotomy
- trochanteric slide
- gluteus medius and sastus lateralis attached / digastric
- osteotomy with saw posterior to anterior
- leave short external rotators attached to preserve deep branch MCFA
- slide GT fragment anteriorly
- capsulotomy as above
- allows access to anterior aspect femoral head
- dislocate femoral head anteriorly / surgical dislocation
Smith-Petersen approach
- good approach if only Pipkin fracture needs fixation
- higher risk of HO
Complications
Sciatic nerve injury 4%
- traumatic
- iatrogenic
Infection 3%
Recurrent instability
- large femoral head fracture excised
- posterior wall fracture
- rarely due to labral tear
AVN
HO
- increased with anterior approach
OA
Results
Giannoudis et al Injury 2009
- systematic review
- Pipkin I: excision gave better results than fixation
- Pipkin II: ORIF
- AVN 11% / OA 20% / HO 17%
- no difference between trochanteric flip / anterior or posterior approach
Chen et al Int Orthop 2010
- RCT of excision v non operative for Pipkin 1 in fracture dislocation
- better outcomes in excision
