Indications
Lateral compartment OA
Valgus malalignment
- lateral cartilage procedures
- lateral meniscal transplant
High Tibial Osteotomy (HTO) for Valgus Malalignment
Issues
Valgus typically caused by hypoplastic lateral femoral condyle
Correcting varus in the tibia leaves joint tilt
- > 10o joint line tilt continues to overload lateral compartment
- get shear forces and lateral tibial subluxation
Historically
- poorer outcomes for HTO for lateral compartment osteoarthritis
Distal femoral varus osteotomy (DFVO)
Indications
- > 12o valgus
- mechanical axis passes through the lateral compartment
Contra-indications
- < 90o flexion
- > 15o fixed flexion deformity / contracture
- tibial subluxation
- medial compartment OA
- smoking
Aim
Focal cartilage defects / lateral meniscal defects
- produce 0-2° valgus of anatomical axis
- neutral mechanical axis (weight bearing line between tibial spines)
Lateral compartment OA
- 62.5% into the medial compartment
Options
- medial closing wedge
- lateral opening wedge
Lateral compartment OA
Saithna et al Open Orthop J 2012
- systematic review of DFVO for lateral compartment OA
- survival with arthroplasty as endpoint
- 64 - 82% at 10 years
- 45% at 15 years
Preoperative Planning
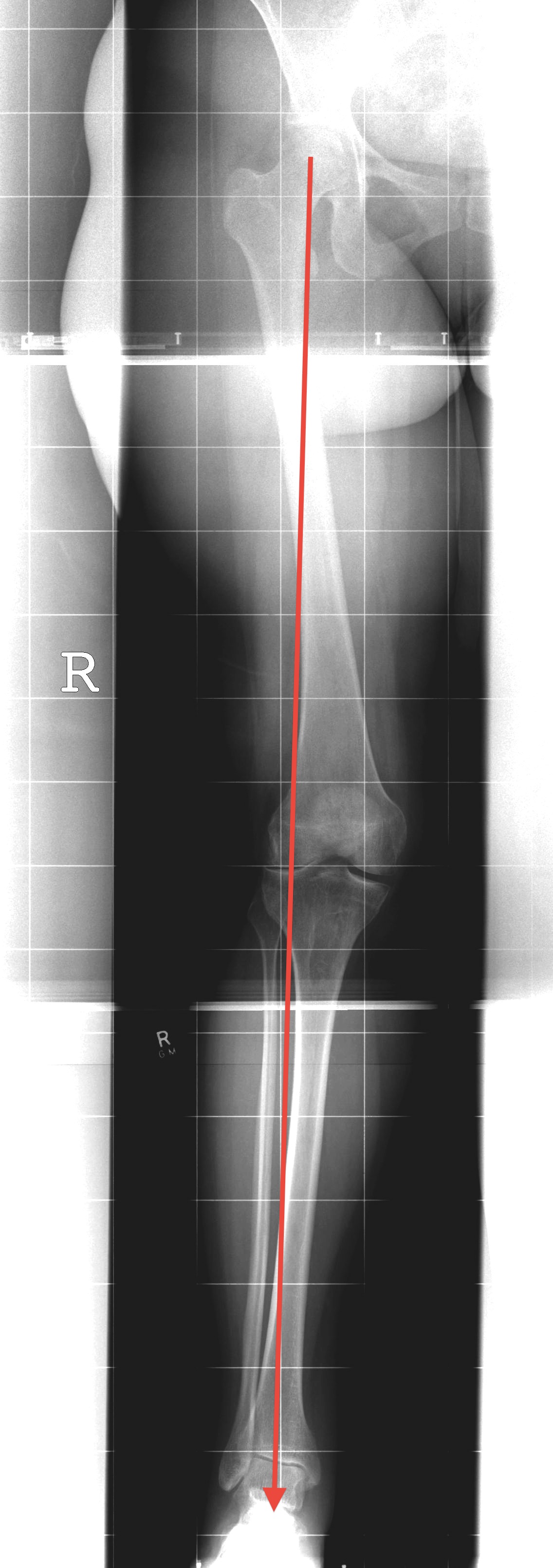
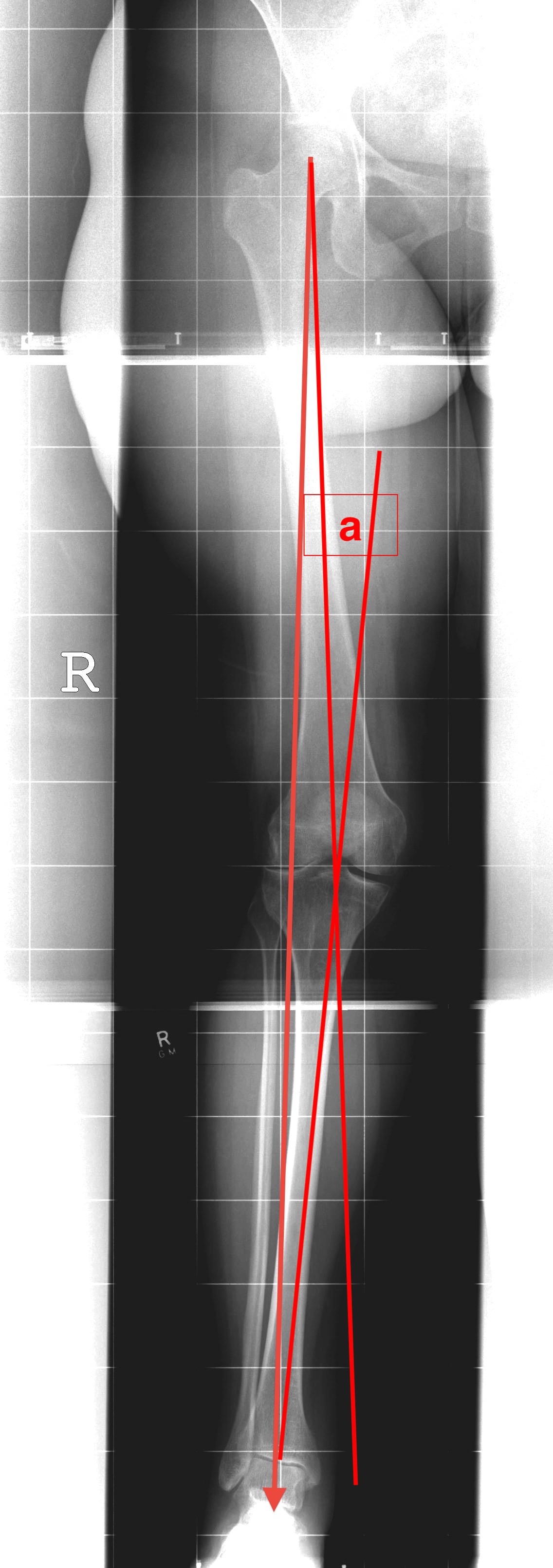
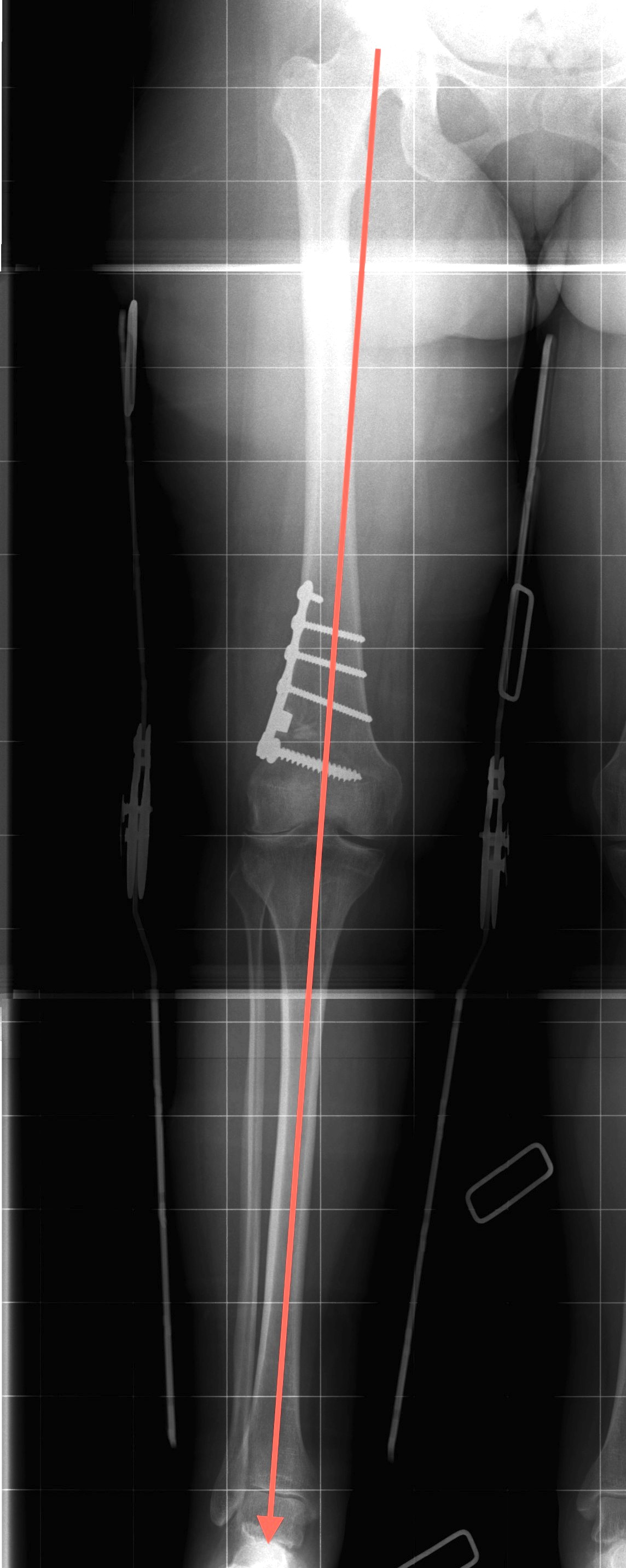
AP full length standing xrays
Line from centre of talus to desired mechanical axis
Line from centre of femoral head to desired mechanical axis
a) is the desired angle of correction
Opening wedge versus Closing wedge
Diaz et al Am J Sports Med 2023
- systematic review of opening wedge (OW) versus closing wedge (CW)
- 23 studies and 619 patients
- no significant difference in outcomes scores
- no significant difference in complications
- painful hardware requiring removal most common complication
- 8 year survival CW DFVO 82%
- 4 year survival OW DFVO 91%
Lateral Opening Wedge Femoral Osteotomy
Advantage
- simple surgical approach
- single osteotomy cut
- more accurate correction
Disadvantages
- lengthen leg
- higher risk of non union
- better for smaller corrections
- plate often irritates iliotibial band


Technique
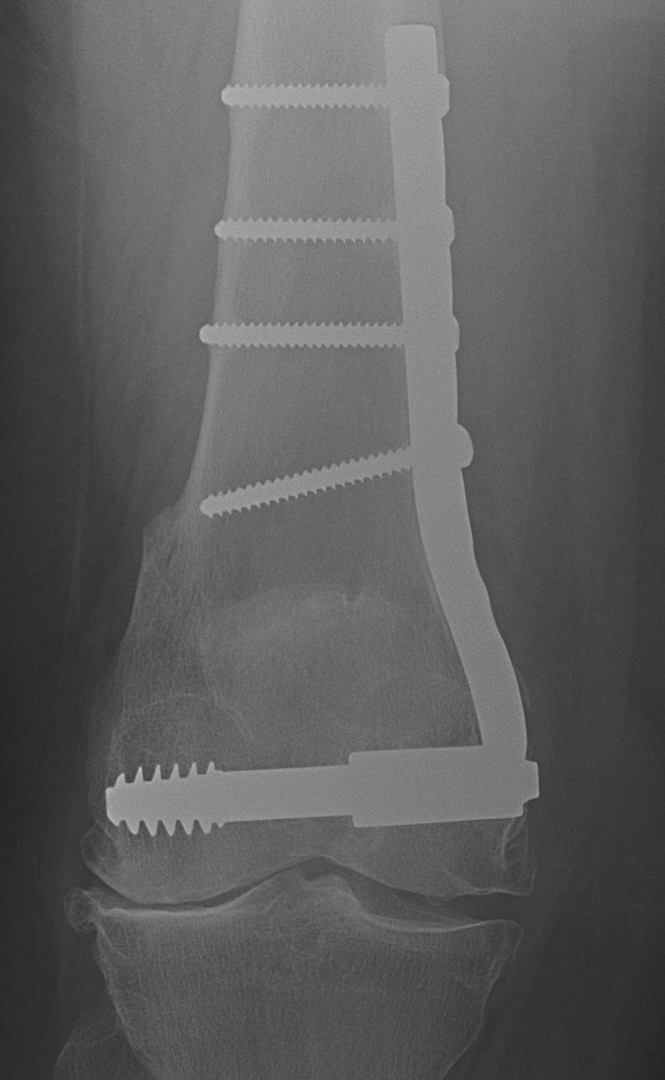
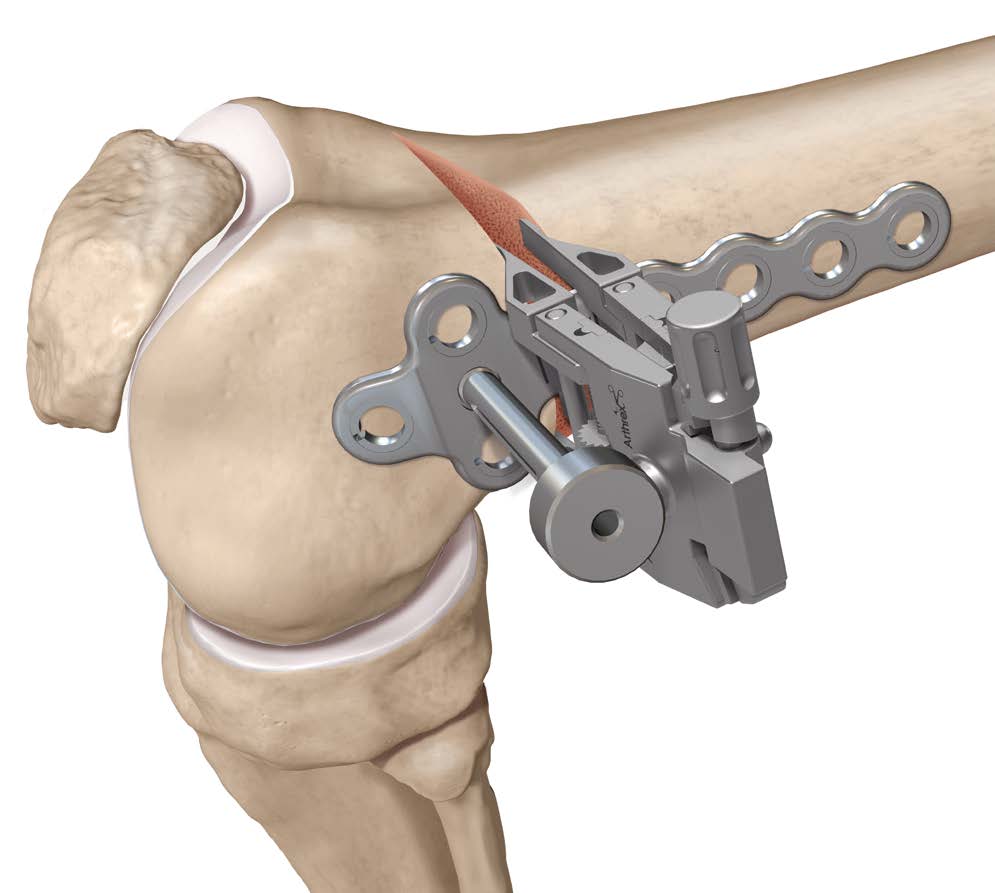
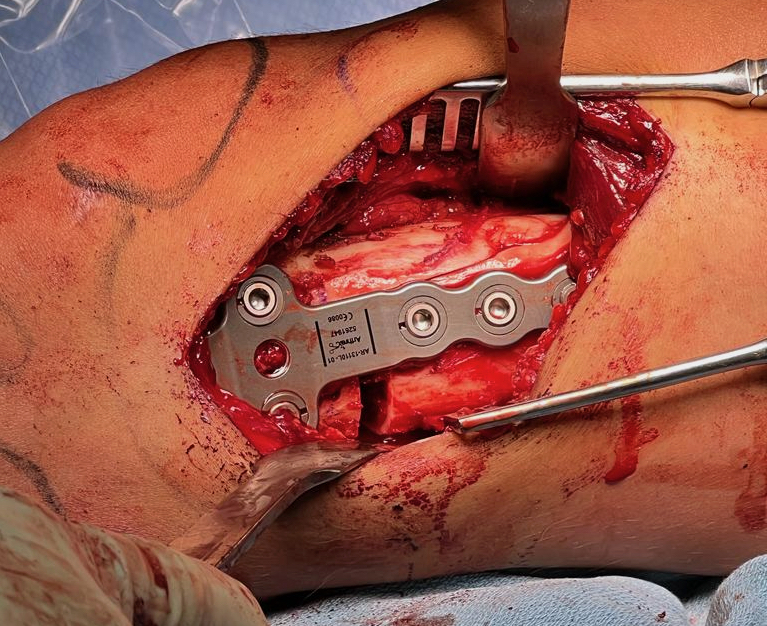
Arthrex ContourLock Distal Femoral Osteotomy Plates
Surgical technique video opening wedge distal femoral osteotomy
Vumedi technique opening wedge distal femoral osteotomy
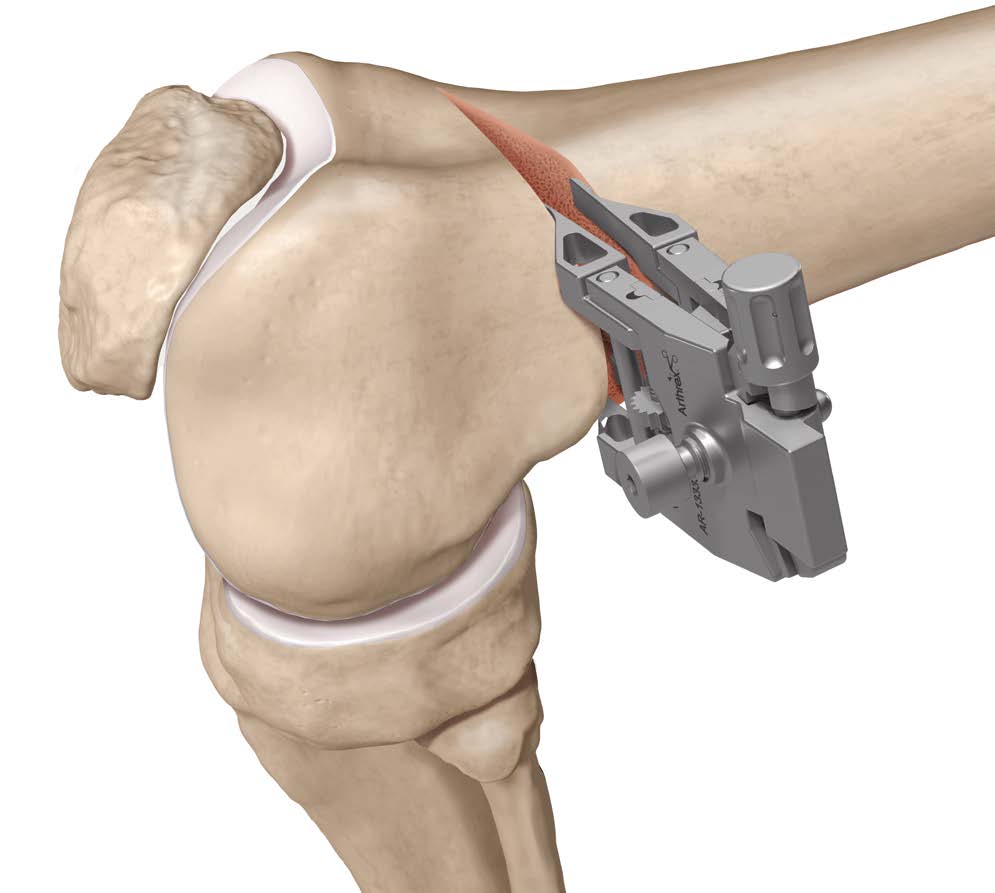
Patient supine on a radiolucent table
Surgical approach
- lateral 12 - 15 cm incision
- split iliotibial band
- ligate perforators and elevate vastus lateralis off intermuscular septum anteriorly
- release intermuscular septum posteriorly at metaphyseal-diaphyseal junction
- protect neurovascular bundle
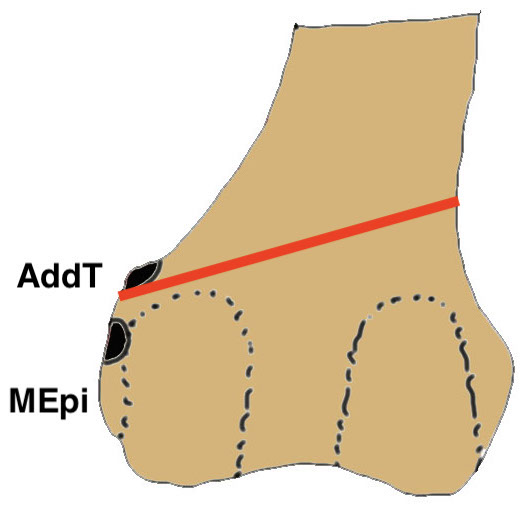
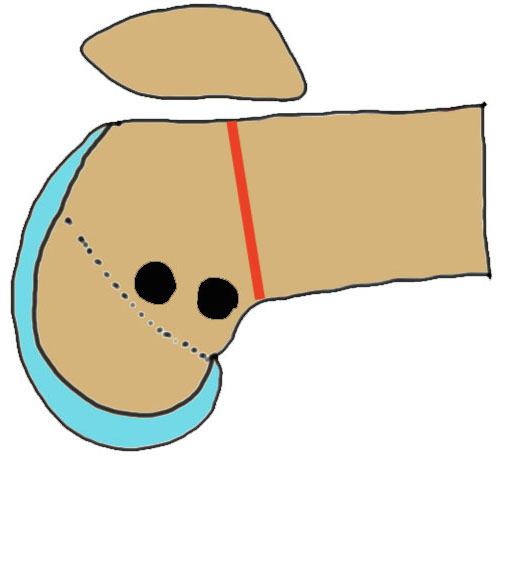
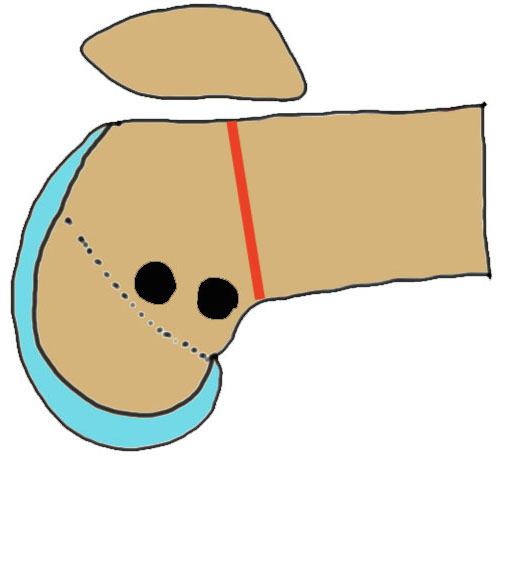
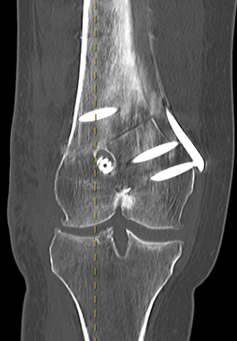
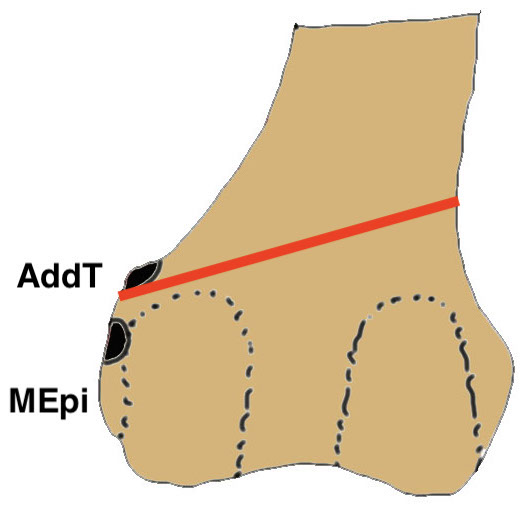
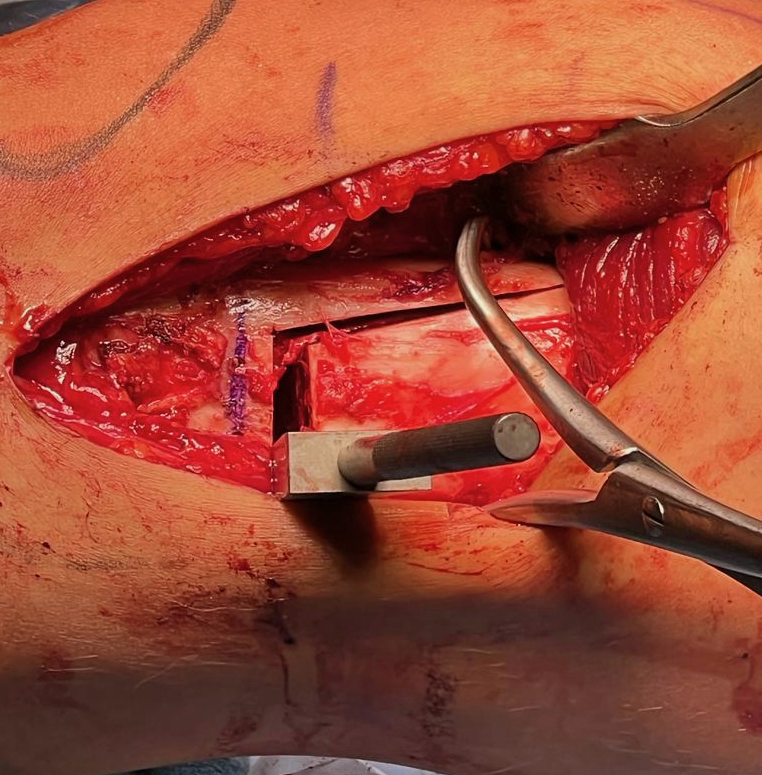
Osteotomy
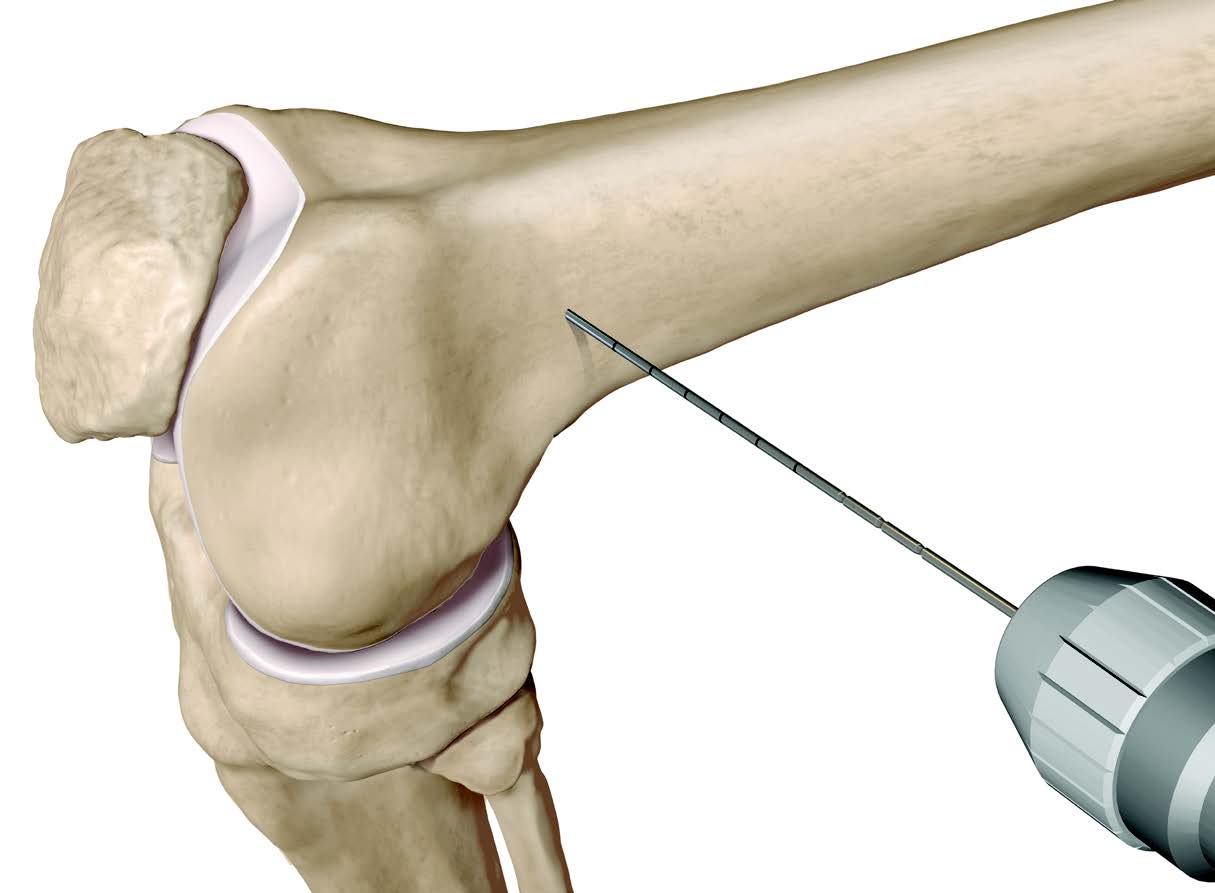
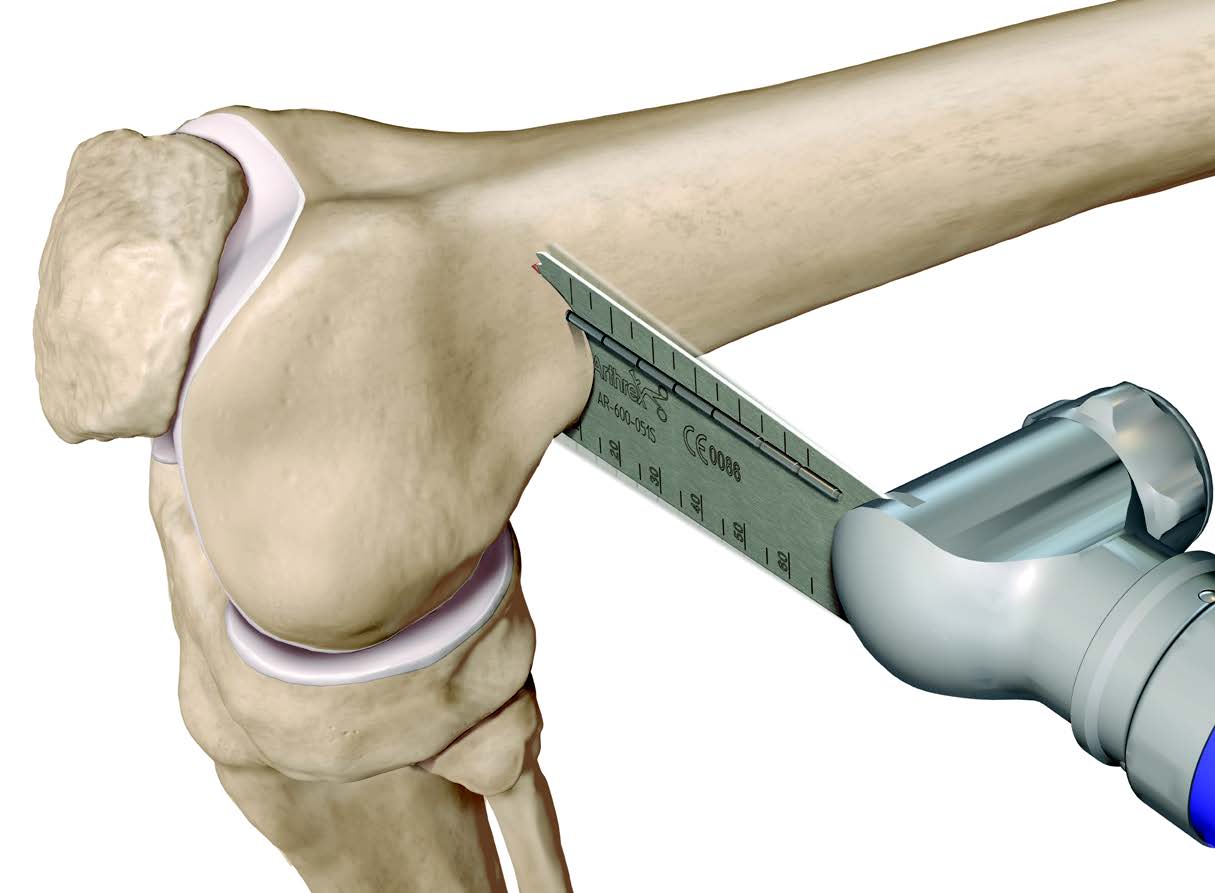
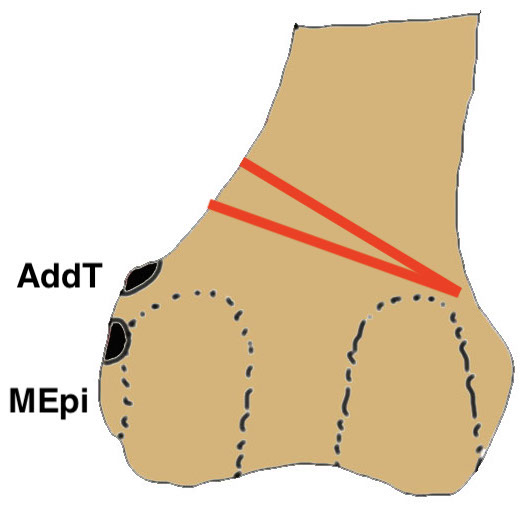
- insert guide wires
- proximal lateral to distal medial
- proximal 1 - 2 cm above flare of lateral condyle
- aim towards adductor tubercle
- risk of medial hinge fracture reduced if osteotomy at or distal to adductor tubercle
- ensure these are perpendicular to the femoral shaft in the sagittal plane
- above patellofemoral joint and posterior condyles
- stop osteotomy 1 cm short of medial cortex
Open osteotomy
- maintain medial cortical hinge
- limit opening wedge to reduce fracture risk
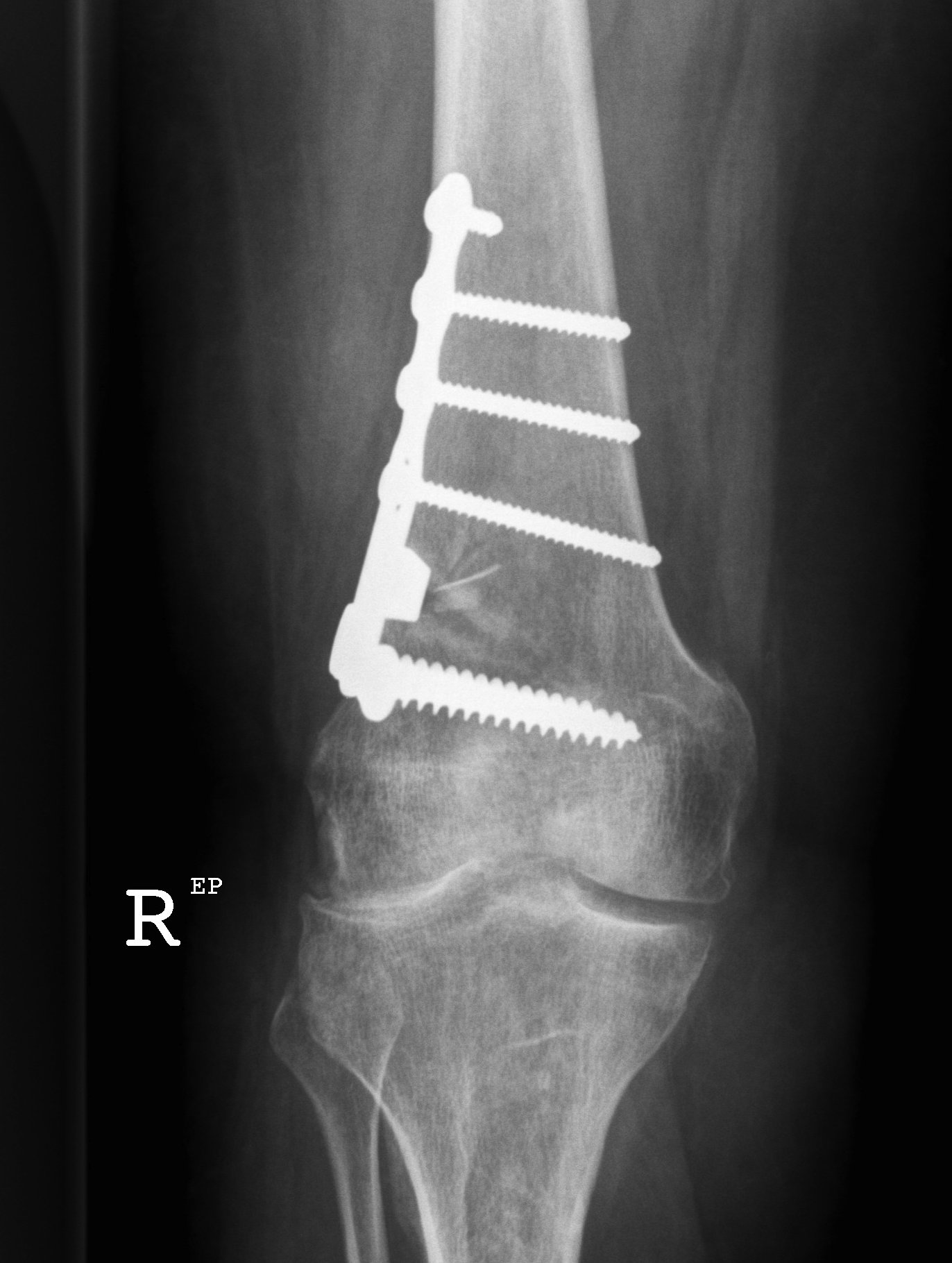
Distal femoral locking plate + bone graft






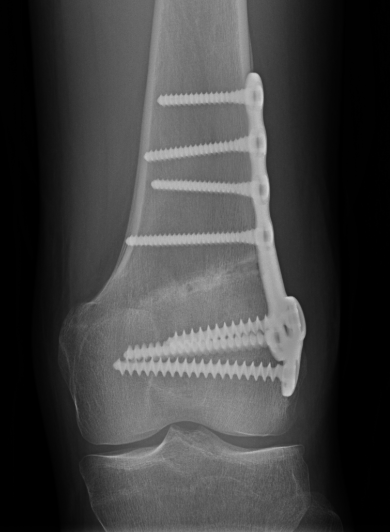
Results
- 5 year follow up of 18 patients treated with OW DFVO for valgus OA
- 79% survival at 5 years
- 1 nonunion, 2 loss of correction, 1 infection
- 2 persistence of symptoms
Avoiding medial cortical hinge fracture
- 100 patients with mean age 31 undergoing OW DFVO
- 46% incidence of medial cortical hinge fracture
- reduced risk if osteotomy at or distal to adductor tubercle (27%)
- increased risk if osteotomy closer to medial cortex
- increased risk with increased height of osteotomy gap
Nonunion
- 41 patients with OW DFVO
- medial hinge fracture in 39%
- 3 delayed union
- 1 nonunion requiring revision surgery
Medial Closing Wedge Osteotomy
Advantages
- lower risk of non union
- better for larger corrections
Disadvantage
- requires two osteotomy cuts
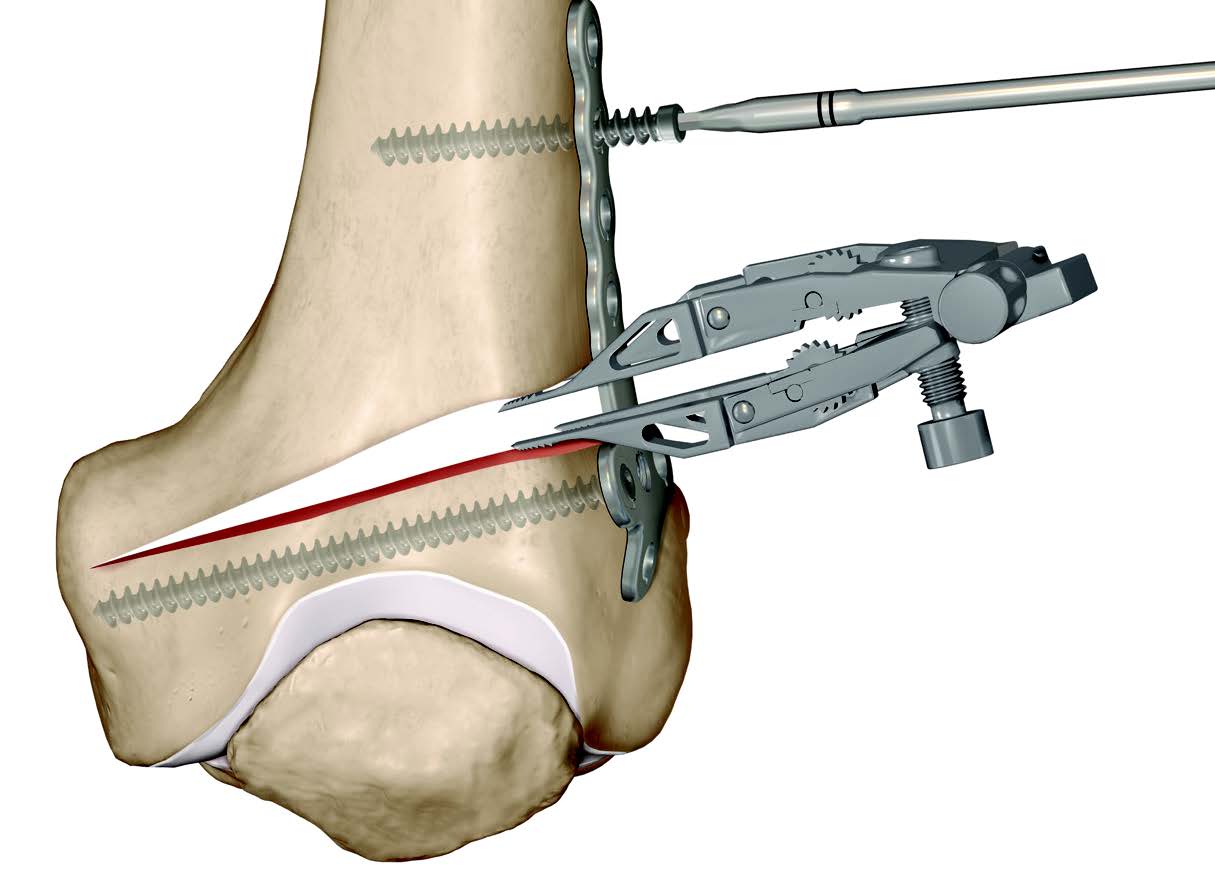
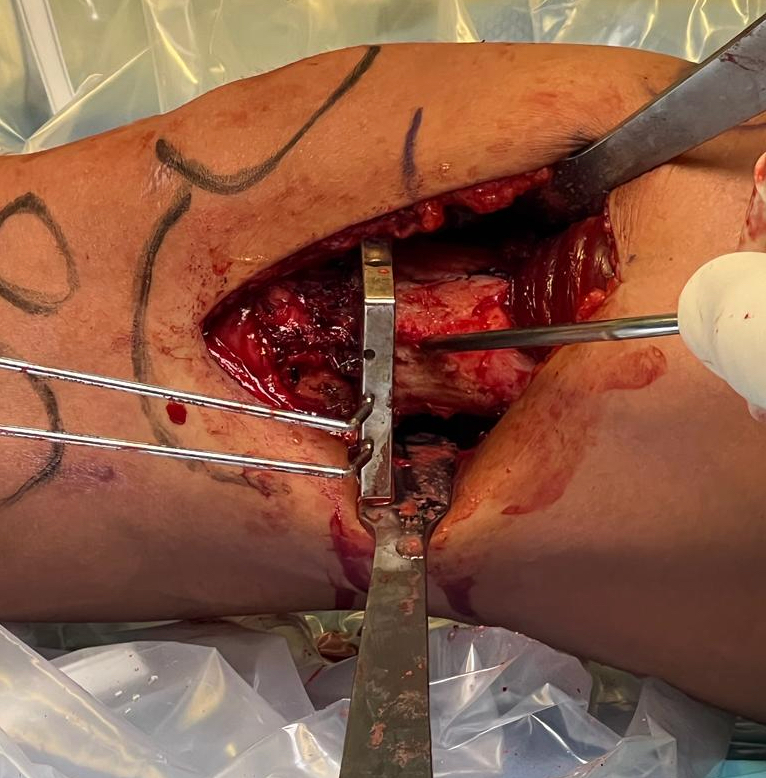
Technique
Vumedi medial closing wedge osteotomy
Patient supine on a radiolucent table
Surgical approach
- medial longitudinal incision
- identify fascia of vastus medialis and joint capsule
- elevate vastus medialis off medial intermuscular septum leaving cuff of tissue to protect vessels
- Hohmann retractor posteriorly to protect NV bundle
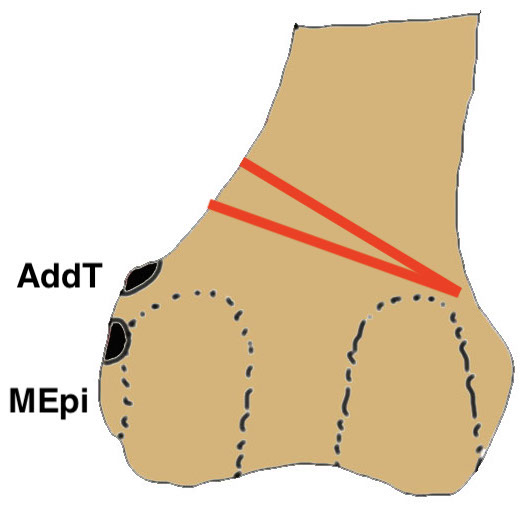
Osteotomy
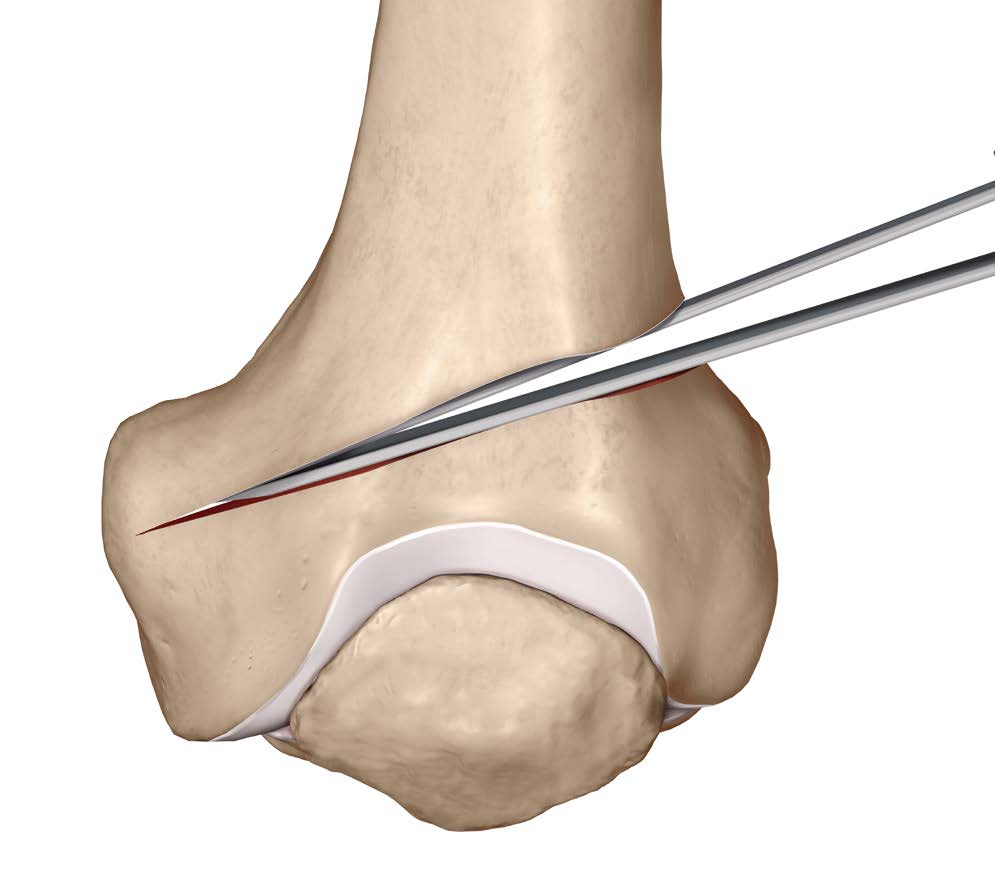
- insert two K wires for desired wedge
- resect templated wedge
- stop 1 cm short of lateral cortex
- close femoral wedge
Lateral hinge fracture
Fujita et al Arch Orthop Trauma Surg 2023
- 21 patients with CW DFVO
- lateral hinge fractures in 57%
- hinge fracture associated with delayed healing
- recommend osteotomy at endpoint of distal lateral cortex
Results
Sternheim et al Orthopedics 2011
- 45 CW DFVO for lateral OA
- mean 13 year follow up
- 90% 10 year survival
- 79% 15 year survival
- 22% 10 year survival
- 8 year follow up of 30 patients undergoing CW DFVO for lateral OA
- 83% satisfactory result
- remainder converted to TKA or poor result
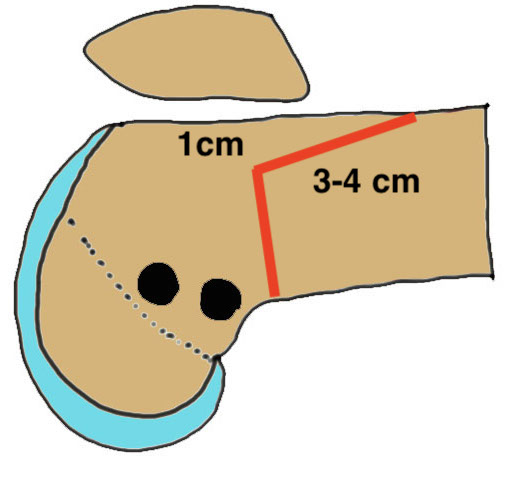
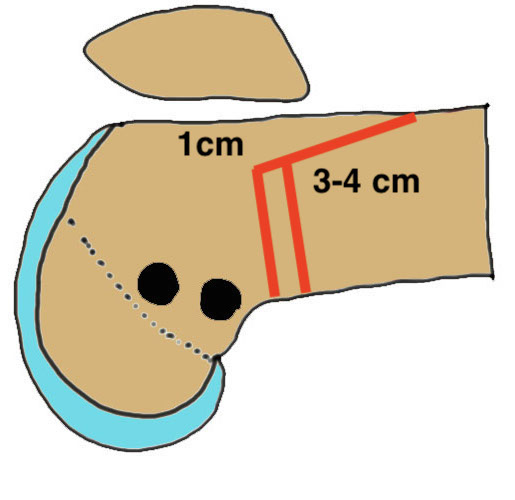
Biplanar Osteotomy
Concept
Create anterior flange
- minimum 1 cm deep
- 3 - 4 cm long

Advantage
Increased mechanical stability / controls rotation
Increases surface area for healing
Lateral Opening Wedge Biplanar Technique
Lateral opening wedge biplanar osteotomy surgical technique
Vumedi lateral opening wedge biplanar osteotomy surgical technique

Medial Closing Wedge Biplanar Technique
Medial closing wedge biplanar osteotomy surgical technique
Vumedi medial closing wedge surgical technique
Complications
Intra-articular fracture
- osteotomy too close to joint
- failure to divide posterior / anterior cortex
Fracture through far cortex
- leave sufficient hinge of bone
- make osteotomy sufficiently distal
Over / Under correction
Neurovascular injury
Keep knee flexed
Posterior retractors
- superior medial and lateral geniculate artery at risk during DFVO
- vascular anatomy of medial approach
- posterior border of VMO touched superficial femoral artery at average of 36mm from suprapatella border
Blood loss
Steinhaus et al J Knee Surg 2020
- reduced blood loss with TXA after DFVO
- most reduced with 1g TXA preop and 1g TXA 4 hours later
DVT / PE
Nonunion
- systematic review of 3000 opening wedge osteotomy cases
- delayed / nonunion rates autograft < allograft < bone substitute
Stiffness
Total Knee Arthroplasty following DFVO
Chalmers et al Bone Joint J 2019
- 31 TKA following DFVO
- average patient age 51, average time from DFVO 10 years
- 88% 10 year survival with revision as endpoint
- balancing the knee challenging
- 13% required varus valgus constraint
- 2 knees revised for instability
- 9 patients
- technically demanding
- femoral IM rod tended to place femoral component in varus