Surgical Algorithm
Stage 1 Tendonitis
Non-operative
Walking cast / NSAIDS
- 6/52
UCBL
- 3/12
- worn inside the shoe
- ends under malleoli
- controls the heel (which must be flexible)
- supports the arch
Operative / Synovectomy and debridement
(+/- FDL transfer and calcaneal osteotomy +/- T Achilles lengthening)
Stage 2 Tendon Rupture
Non Operative
- UCBL
Operative
2A - FDL transfer & calcaneal osteotomy +/- T Achilles lengthening
2B - + Lateral column lenthening to correct abduction
Stage 3 Rigid valgus hindfoot
Non Operative
Rigid AFO
Caliper: Outside iron with inside T strap
Operative
Triple arthrodesis
Stage 4 / Abnormal AKJ
Pathology
- valgus angulation of talus
- deltoid ligament gone
- early degeneration of ankle joint
- degenerative changes in subtalar & midtarsal joints
- valgus angulation of talus
Non Operative
- double metal uprights with PTB
Operative
- pan talar fusion
Operations
Tibialis Posterior Synovectomy and Debridement
Position
- supine on table
- foot falls into ER
- tourniquet
Incision
- tip of medial malleolus to navicular
- open tendon sheath
- often fluid and synovitis
Synovectomy
Repair any fissures
Inspect insertion
- if partially avulsed
- FDL transfer
Close tendon sheath
S/L cast for 3/52
Results
- 75% good results
Calcaneal Osteotomy / Medial Calcaneal slide
Aim
- shifts calcaneum medially
- reduces valgus thrust on hindfoot
- pull of gastoc/soleus is medial to STJ
Indications
- stage 1 or 2
- in combination with FDL transfer
Timing
- perform osteotomy first, then tension FDL
Set up
- sandbag under ipsilateral hip
- table rolled over to expose lateral heel
- then unroll bed to expose medially

Incision
- lateral incision
- in line with peroneal tendons
- need to protect sural nerve posteriorly
Osteotomy
- protect peroneals
- protect T Achilles
- behind posterior facet STJ
- transverse osteotomy at 45o to plane of foot
- complete with osteotome to protect medial structures
- use osteotome to gently break up periosteum
- use lamina spreader to break up final adhesions
- translate 10mm medially
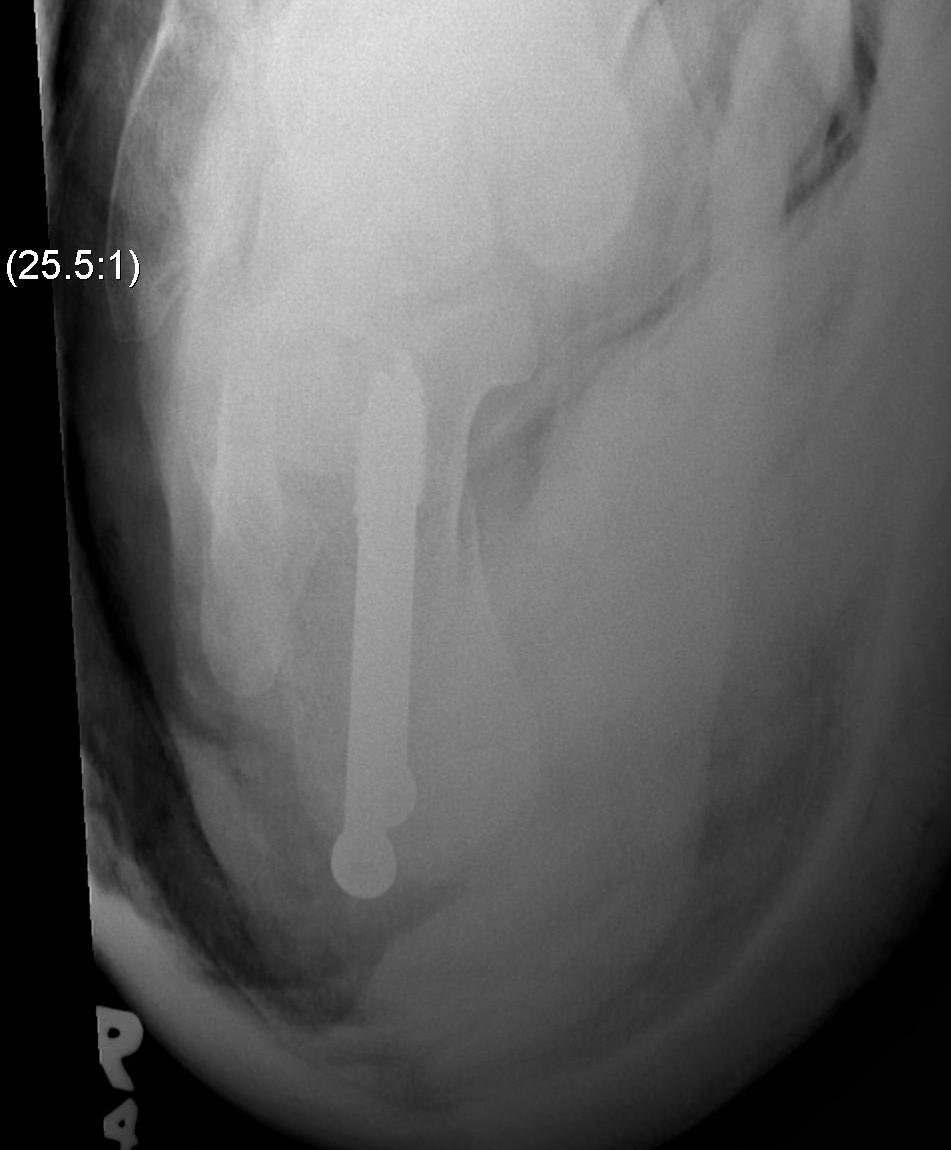
ORIF
- K wire lateral to T Achilles, towards CCJ
- check II, 6.5 mm partially threaded cannulated screw
Lateral column lengthening
Indications
- midfoot abduction
Technique
- anterior calcaneal ostetomy
- insertion bone graft wedge
- stabilisation plate or screws
FDL transfer
Reasons
- FDL easily found by reflecting abductor hallucis
Indications
- foot should be supple with no fixed deformity
- stage 1 / 2
Incision
- along entire length T posterior
- 10 cm proximal to medial malleolus
- to metatarsal cuneiform joint
Superficial dissection
- expose T posterior in sheath
- may be ruptured, avulsed, deficient, fissured
Deep dissection
- abductor hallucis reflected plantarward
- find fat / Knot of Henry
- release Master Knot of Henry
- crossover of FDL & FHL
- FDL plantar to FHL
- suture together and release proximal FDL
TNJ
- open to visualise
- 4.5mm drill hole through navicular
- Reinsert FDL into underside of navicular
- plantar to dorsal
- pulled tight with ankle in equinus & forefoot in varus
- close TNJ capsule
- No need to attach proximal T Post to FDL
Repair spring ligament
Closure abductor fascia
Post op
- 6/52 in equinus and inversion NWB
- x-ray to check osteotomy has healed
- 4/52 weight bearing in removable cast with ROM exercises
- may need physio
Triple Arthrodesis
Indication
- fixed hindfoot deformity with lateral joint pain
Aim
- realign hindfoot
- plantigrade surface
- maintain integrity of adjacent jts
- avoid neuromas
Issues
1. Fuse TNJ first
- this should passively align STJ
- need medial approach to reduce TNJ
2. Fuse STJ
- slight valgus not neutral or varus
- lateral approach
- may need large lateral bone wedge
- may have issues with lateral skin closure
