
Management
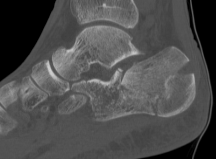
Operative versus non operative
- RCT of 309 displaced intra-articular fractures
- operative v non operative management with 2 year follow up
- extensile lateral approach and fixation with 1/3 tubular plate
- 2 year follow up
- overall no difference in outcomes
- better outcomes with operative: Type II / non workers compensation / women / < 29 / anatomic reduction
- RCT of 151 intra-articular fractures
- operative versus nonoperative for displaced intra-articular fractures
- no difference in outcomes
Zhang et al J Orthop Trauma 2016
- meta-analysis of 7 RCTs and 900 patients
- operative versus nonoperative for displaced intra-articular fractures
- no difference in most outcomes
- increased complications with operative management
- better shoe wear and walking ability with operative management
Non Operative Management
Indications
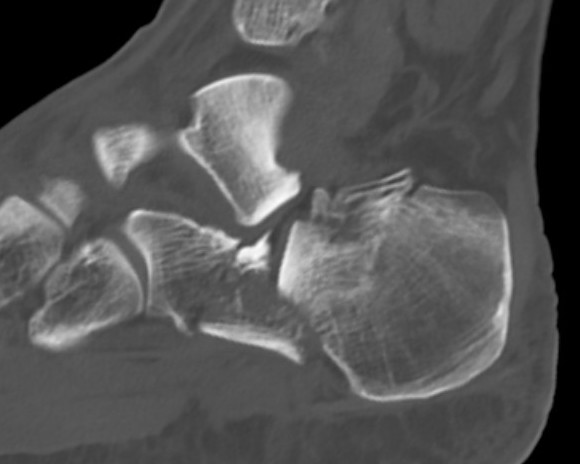
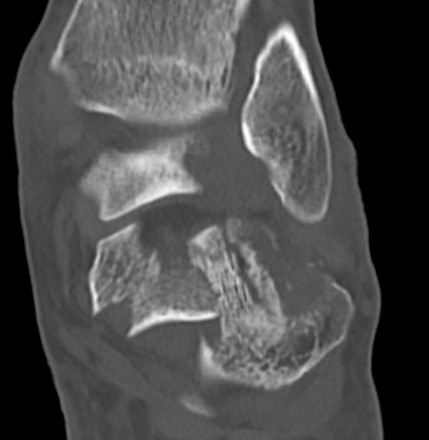
Sander I - non displaced
Sanders IV
Diabetes / smoker / peripheral vascular disease
Compound fractures
Technique
Cast / boot
NWB 6/52
Complications
Subtalar OA
Calcaneocuboid arthritis
Hindfoot varus malunion
Peroneal impingement or subluxation
Posterior tibial nerve entrapment
Difficulty with shoe wear

Operative Management
Aims
Pain free functional foot that can fit in a shoe
Goals
1. Restore heel shape (height, length / width / valgus)
2. Reduce joint surface
Options
ORIF via extensile lateral approach
Minimally invasive ORIF via sinus tarsi approach
Percutaneous fixation
Intramedullary nail
Primary subtalar arthrodesis
Results
Extensile lateral approach versus minimally invasive sinus tarsi approach
Nosewicz et al Foot Ankle Surg 2019
- systematic review of extensile lateral versus sinus tarsi approach
- 9 studies and 700 patients
- wound healing issues extensile lateral: 25%
- wound healing issues sinus tarsi 5%
- no difference functional outcomes
Screws versus plate in MIS vis sinus tarsi approach
Zhao et al Arch Orthop Trauma Surg 2024
- systematic review of fixation via sinus tarsi approach
- screw versus plate fixation in 7 studies and 700 patients
- no difference outcomes
- better reduction with plates
Percutaneous fixation versus extensile lateral approach
DeWall et al J Orthop Trauma 2010
- RCT of 125 fractures
- percutaneous fixation versus extensile lateral approach
- deep infection 6/42 extensile lateral
- deep infection 0% percutaneous fixation
Percutaneous fixation versus MIS / sinus tarsi
Feng et al BMC Musculoskeletal Disorders 2016
- RCT of 80 patients
- percutaneous screws v sinus tarsi approach / plate
- comparable clinical outcomes
- better restoration of heel width with sinus tarsi approach
Nail versus plate
Fu et al J Dis Relat Surg 2024
- systematic review of 5 controlled studies and 473 patients
- IM nail versus plate
- no difference in outcome
- lower total complications and wound issues with nail
Primary subtalar fusion
Patel et al J Foot Ankle Surg 2021
- systematic review 500 ORIF v 60 primary fusion for Type II/III
- better functional outcomes with ORIF
Buckley et al J Orthop Trauma 2014
- RCT of 31 patients with Type IV
- ORIF v primary fusion
- no difference in outcome
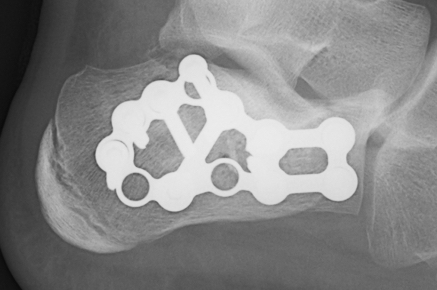
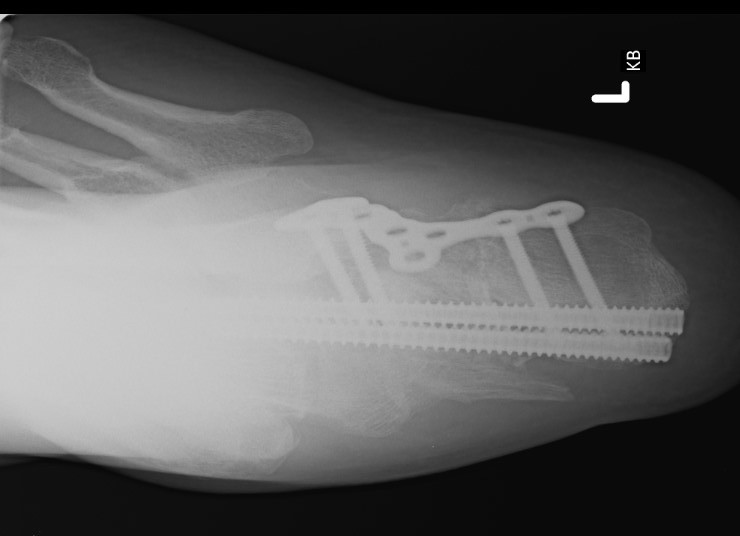
ORIF lateral plate using extensile lateral approach
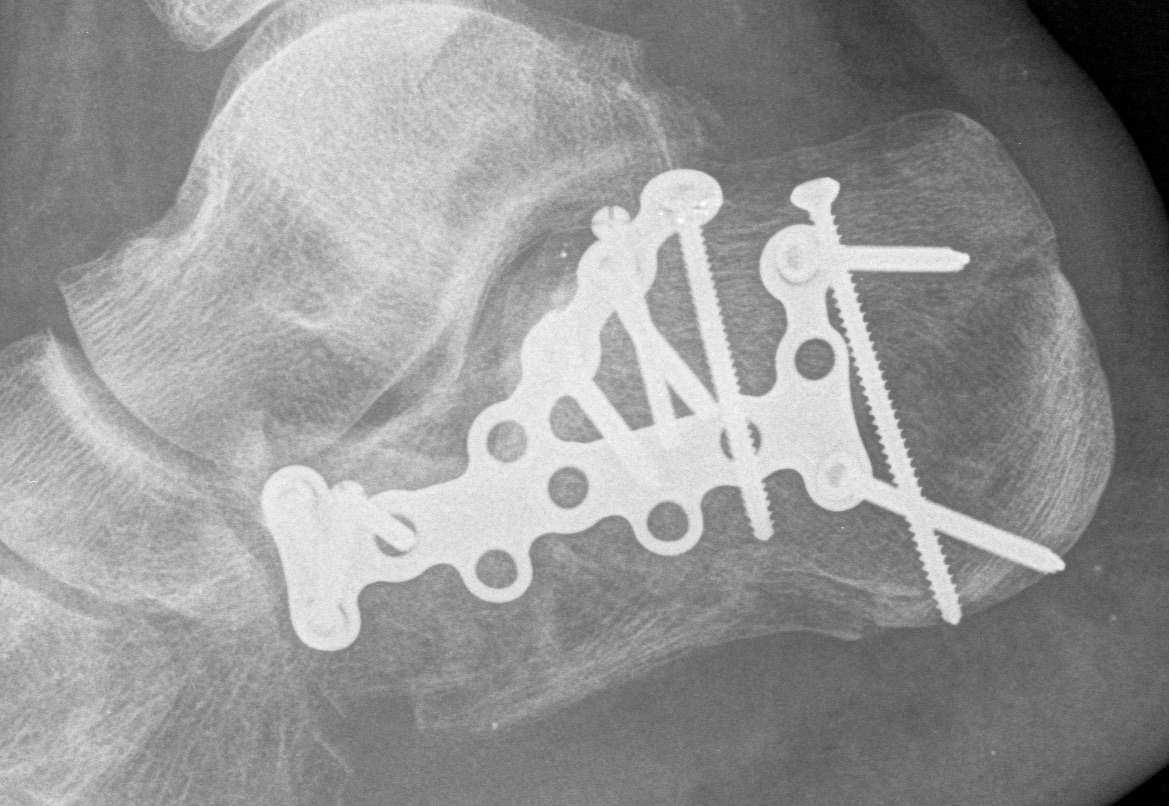

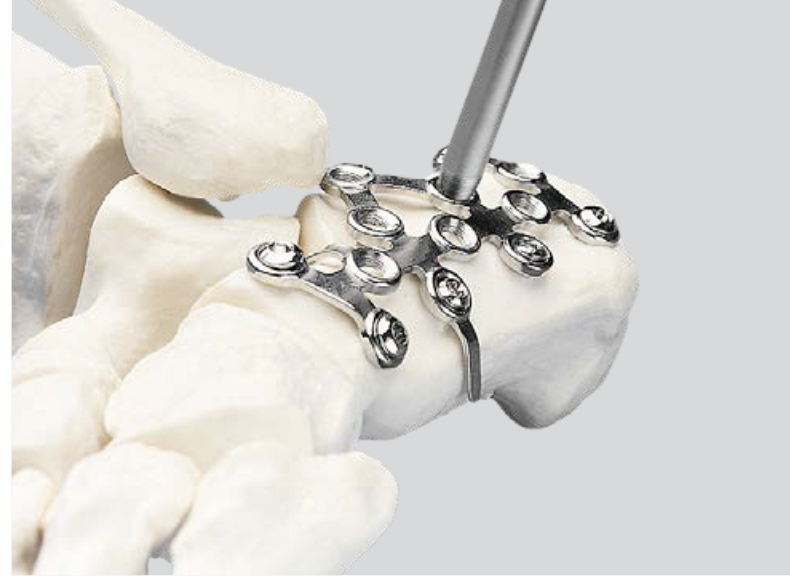
Depuy Synthes calcaneal locking plates PDF
Technique
AO surgery reference extensile lateral approach
AO surgery calcaneal ORIF lateral plate
Vumedi ORIF calcaneum via extensile lateral approach
Position
- patient on side, blankets under foot
- operated foot up
- radiolucent table, image intensifier
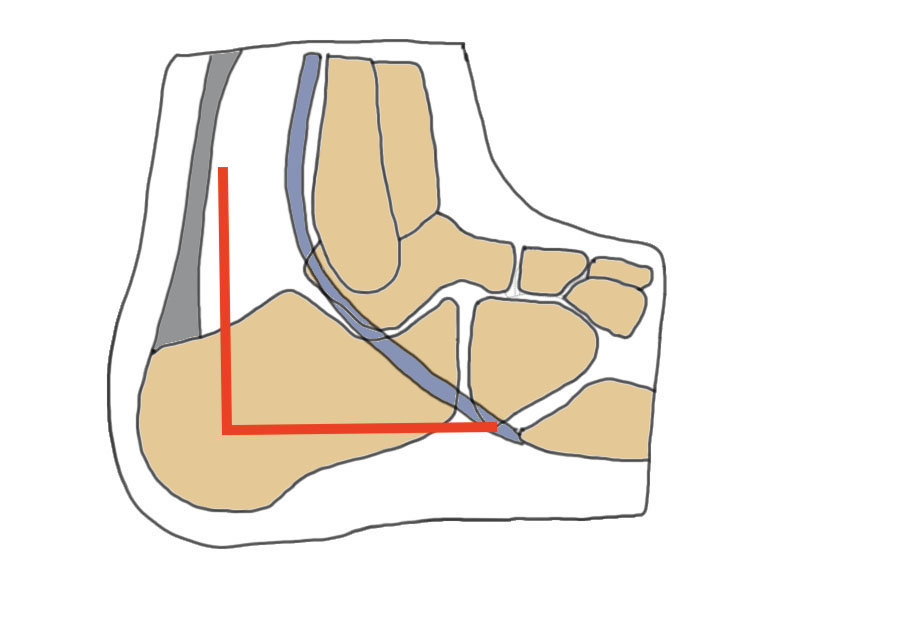
Extensile lateral approach
- vertical limb: between tendoachilles and fibula
- horizontal limb: in line with 5th metatarsal towards CC joint
- full thickness flaps - care ++++ with apex of incision
- divide peroneal retinaculum
- peroneal tendons elevated
K wires to retract skin flap
- 2 in talus / 1 in fibula
Expose subtalar joint
Reduction of varus
- Steinmann pin into tuberosity
- can elevate and pull out of varus
Reduction of subtalar joint
- open lateral wall fragment to access to subtalar joint
- lamina spreader
- reduce and ORIF with screws
- reduce and ORIF sustentaculum fragment
Anatomical contoured locking plate

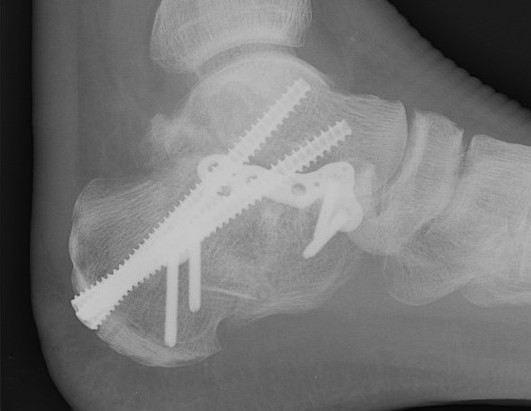
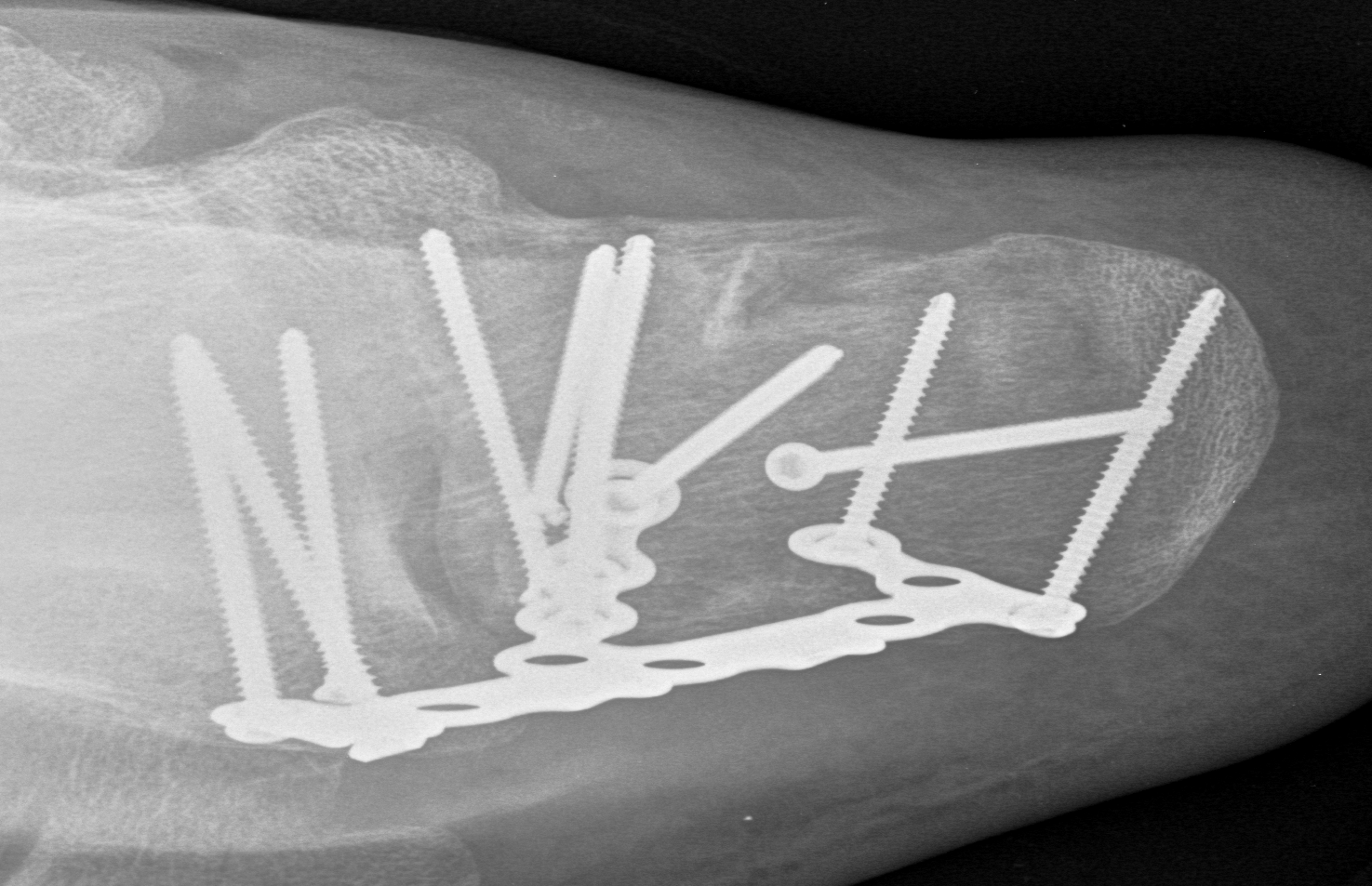
Minimally invasive surgery via sinus tarsi approach
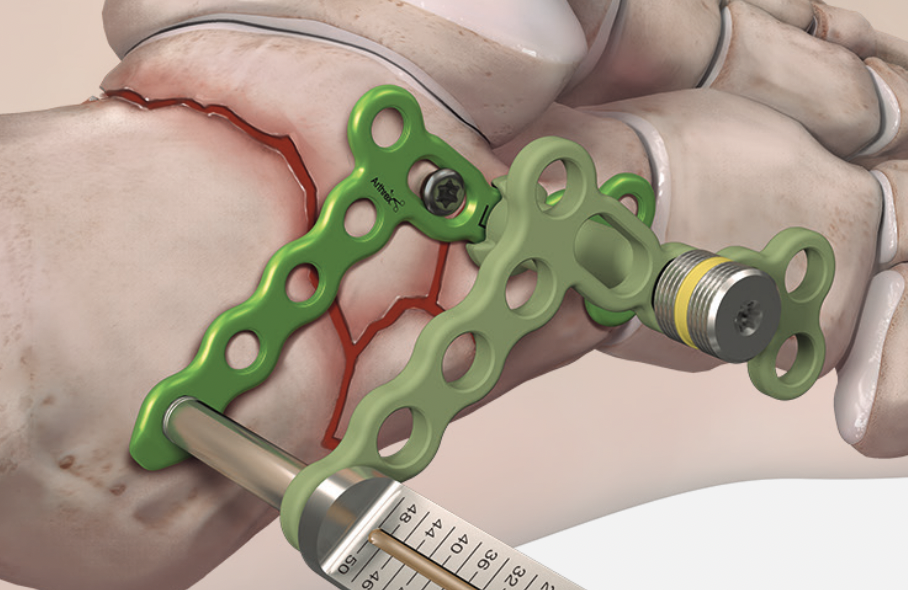
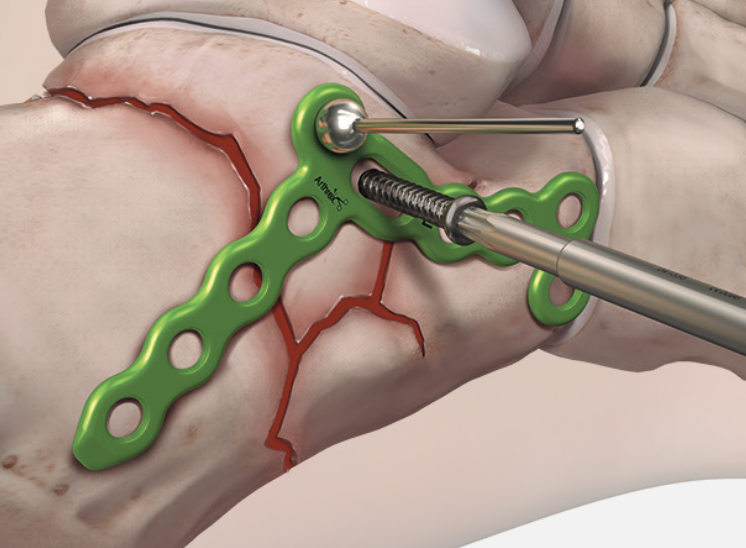

Arthrex MIS calcaneal plating system

Acumed MIS calcaneal plating system
Technique
AO surgery sinus tarsi approach
AO surgery MIS calcaneal ORIF via sinus tarsi
MIS sinus tarsi technique article
Vumedi MIS calcaneum fracture via sinus tarsi
Vumedi MIS calcaneum fracture via sinus tarsi 2
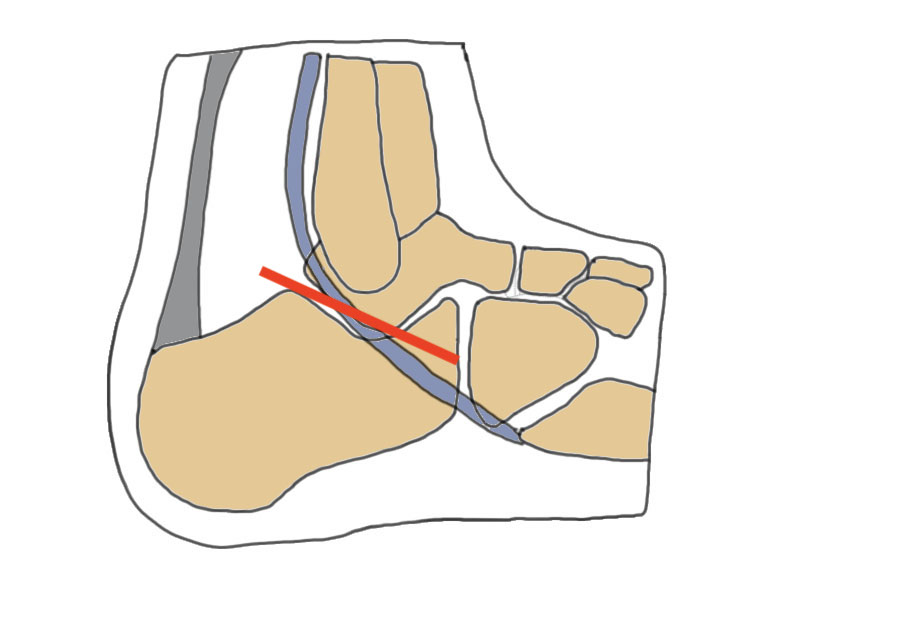
Sinus tarsi approach
- subfibular approach
- centred on subtalar joint
- peroneal and sural nerve inferior
- reflect extensor digitorum brevis
Distraction device
Reduce tuberosity with Schantz pin
Reduce and ORIF posterior facet / sustenaculum talus
Use lateral plate with minimally invasive techniques
Results
- 287 displaced intra-articular fractures
- MUA / Gissane spike percutanous reduction / K wire fixation
- 72% good or excellent results
- 1.7% deep infection, 7% superficial infection
Percutaneous Fixation

Technique
Needs to be performed 3 - 5 days after injury while fracture fragments mobile
Vumedi percutaneous fixation calcaneal fractures
Intramedullary nail
C-Nail


Medin you-tube C-nail animated surgical technique
Vumedi C-nail surgical technique
Reduction
- tuberosity Schantz pin
- percutaneous reduction / K wire fixation or
- sinus tarsi approach to reduce and screw fixate posterior facet
Insertion
- below achilles tendon
- aim towards CC joint
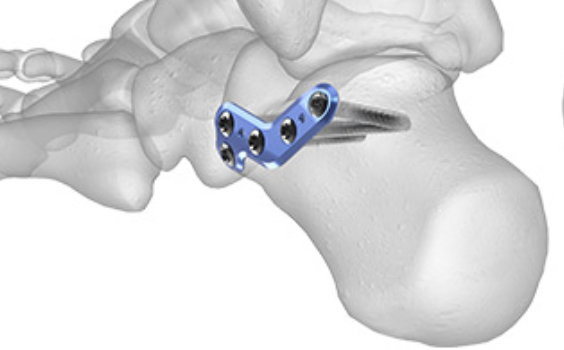
Primary Subtalar Arthrodesis


Indications
Type III / IV Sanders
Complications
General
Wound necrosis
Sural nerve injury
Compartment Syndrome
RSD
Non union
Infection




- RCT of 309 displaced intra-articular fractures
- operative v non operative management with 2 year follow up
- 5% deep infection
- 17% superficial infection
Osteoarthritis


- RCT of 309 displaced intra-articular fractures
- operative v non operative management with 2 year follow up
- STJ arthrodesis: non operative 17%, operative 3%
Calcaneal Malunion

Issues
Varus hindfoot - locks midfoot
Peroneal impingement
Shoewear problems
Options
Lateral wall exostectomy and peroneal tenolysis
Calcaneal osteotomy
STJ arthrodesis
Osteotomy for calcaneal malunion surgical technique PDF
Vumedi calcaneal osteotomy for malunion video
Results
Farouk et al Foot Ankle Int 2019
- 18 varus calcaneal malunions
- combined subtalar joint fusion / calcaneal osteotomy / lateral wall exostectomy
- outcome score increased from 60 to 80
