Radial Head Fracture


Mechanism
FOOSH (fall on outstretched hand)
- axial load with a valgus force
Biomechanics
1. Valgus stability
- secondary stabilizer
- 30%
- becomes primary stabilizer if medial collateral ligament deficient
2. Longitudinal stability
- aided by interosseous membrane
3. Load transfer
- 60% of load at elbow
- with radial head excision, load is transferred to ulno-humeral joint
- increase risk of OA
Anatomy
Radial head
Concave to articulate with capitellum
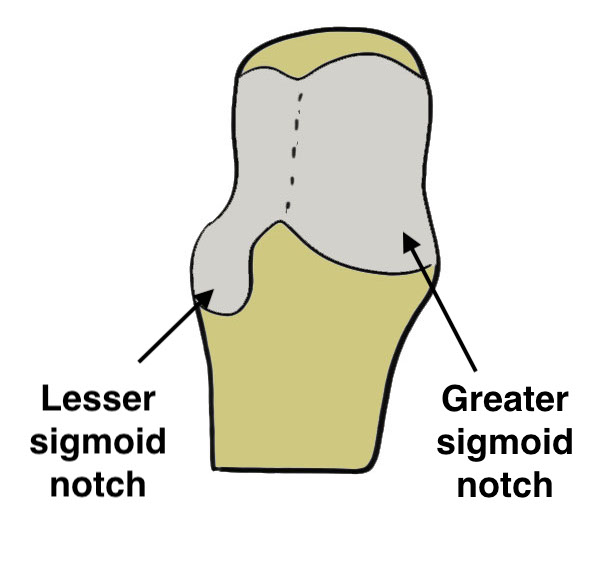
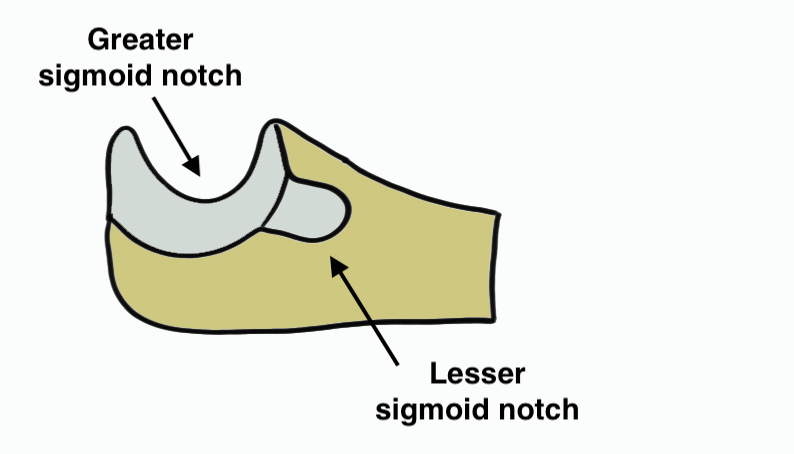
Articulating portion of rim
- articulates with lesser sigmoid notch of ulna
- covered with thick cartilage
Non articulating portion of rim
- covered with thin cartilage
- safe zone for screws
- 110 degrees
- between radial styloid and lister's tubercle
Lesser sigmoid notch
- articulation with ulna
- guidance for radial head replacement
Blood supply
- poor
- single intra-osseous vessel
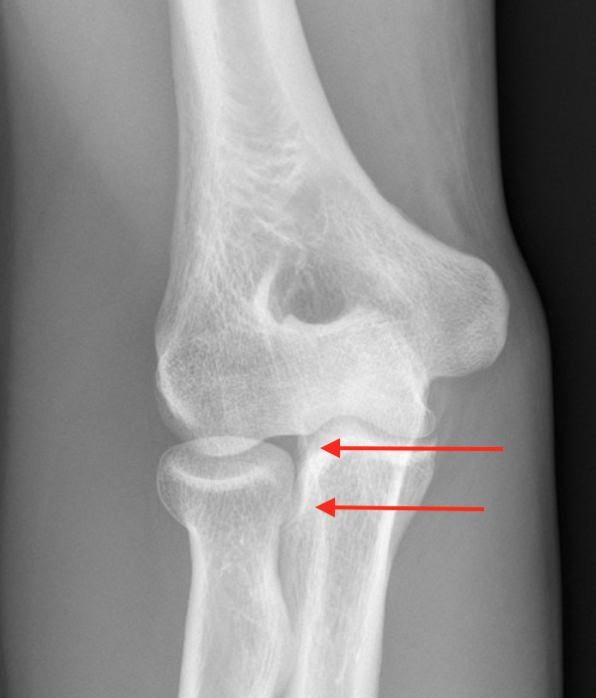
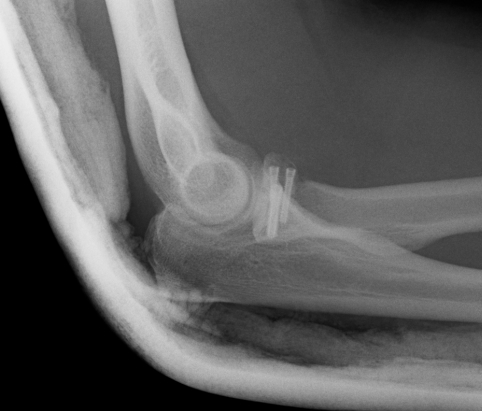
Hotchkiss modification of Mason Classification
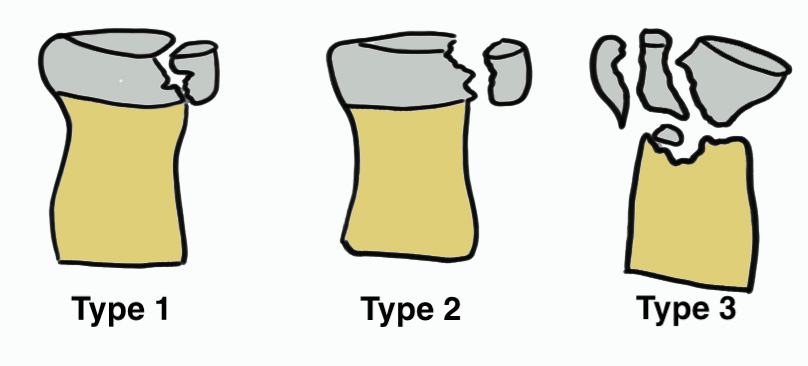
Type 1: Undisplaced fracture
Intra-articular displacement < 2mm
- no mechanical limitation to forearm rotation
- if in doubt, inject LA into radiocapitellar joint / soft spot
- ensure no mechanical block to rotation


Type 2: Displacement > 2mm / Motion mechanically limited / Reconstructable


Type 3: Severely comminuted fracture / Non reconstructable

Type 4: Radial head fracture with elbow dislocation


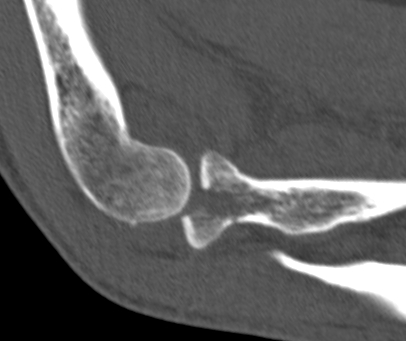
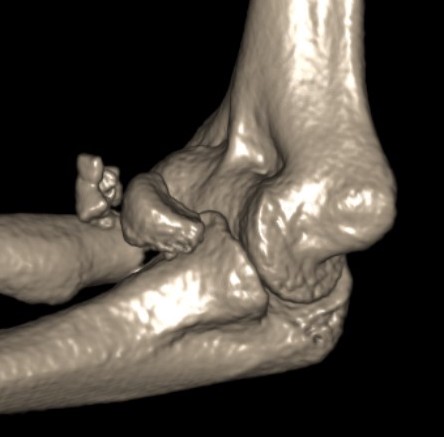
CT scan
Aids surgical planning i.e. fixation v arthroplasty
Identifies associated injuries i.e. coronoid fractures
Complicated Radial Head Fracture
1. Associated injuries
- MRI of 42 radial head fractures
- 24/42 (57%) elbows had LCL injury
- 1/42 (2%) had a MCL injury
- 16/42 (38%) had an injury of the capitellum
- 1/42 (2%) had a coronoid fracture
- 2/42 (5%) had loose osteochondral fragments
2. Elbow Dislocation
Terrible triad: radial head fracture, coronoid fracture, LCL injury
3. Essex Lopresti
Fracture radial head + Disruption DRUJ / interosseous membrane
- dorsal dislocation of DRUJ
Management
- ORIF / replacement radial head
- supinate DRUJ to reduce +/- TFCC repair +/- K wire
Non operative Management
Indications
Mason 1
No block to rotation
Mason 2
- systematic review ORIF v nonoperative treatment for Mason II
- 11 studies and 319 patients
- ORIF: 90% good or excellent results, 7% reoperation, OA 5%
- nonoperative: 95% good or excellent results, OA 12%
- isolated partial radial head fractures displaced > 2 but < 5 mm
- 30 ORIF versus 30 nonoperative
- ORIF group younger and fragments more displaced
- better outcomes in nonoperative group
- 8 cases of mild HO in operative group, and 2 hardware failures
Operative Management
Indications for surgery
van Riet et al Should Elbow 2020
Mechanical block after hematoma aspiration
Displacement > 5 mm
Comminuted fractures (> 2 parts)
Options
Radial Head Fixation
Radial Head Resection
Radial Head Arthroplasty (RHA)
Chaijenkij et al Musculoskeletal Surg 2021
- meta-analysis
- 210 ORIF v 227 RHA v 152 RHR
- RHA had highest outcome scores and lowest complication rate
Approach
Kocher approach
- between anconeus and ECU
- LCL or ulna collateral ligament is at risk
- may make repair or reconstruction of LCL easier
Kaplan interval
- split EDC / interval between EDC and ECRB
- protects LCL
- prevents iatrogenic posterolateral instability
AO Surgery Kocher & Kaplan reference
Posterior Interosseous Nerve (PIN)
Gruenberger et al JSES Int 2022
- 45 cadavers with EDC splint
- used lateral epicondyle as landmark
- PIN 70 +/- 10 mm from lateral epicondyle
- PIN 40 - 48 mm from radiocapitellar joint
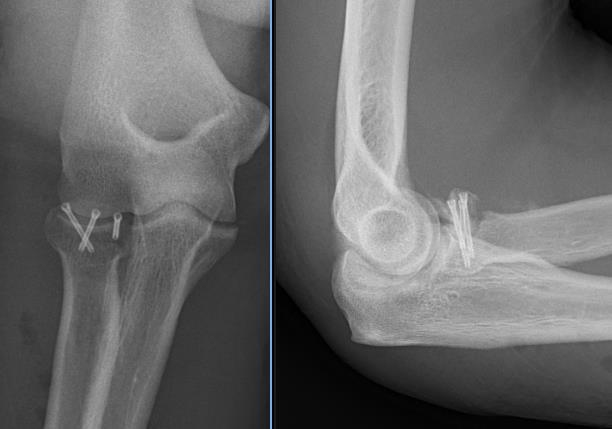
Radial Head Fixation

Indication
Significant fragment displacement
Reconstructable
Technique
Kocher / Kaplan approach
- dissect muscles off capsule
- divide capsule in line with incision / create anterior and posterior flaps
PIN (Posterior Interosseous Nerve)
- pronate forearm to protect PIN
- no Hohmann retractors anteriorly
- limit distal dissection
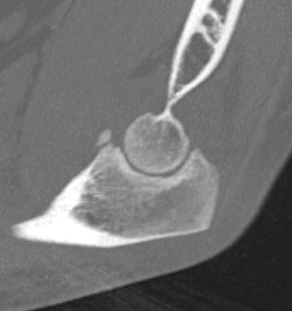
Safe zone for implants
- posterolateral portion of cartilage
- yellow and thinner, non articulating
- 90o arc between radial styloid and lister's tubercle
ORIF
- 2.5 or 3.5 headless compression screws
- 5 mm from joint line as radial head surface concave
Complications
PIN injury
Intra-articular screws
Hardware failure
Heterotopic ossification
AVN
Non union
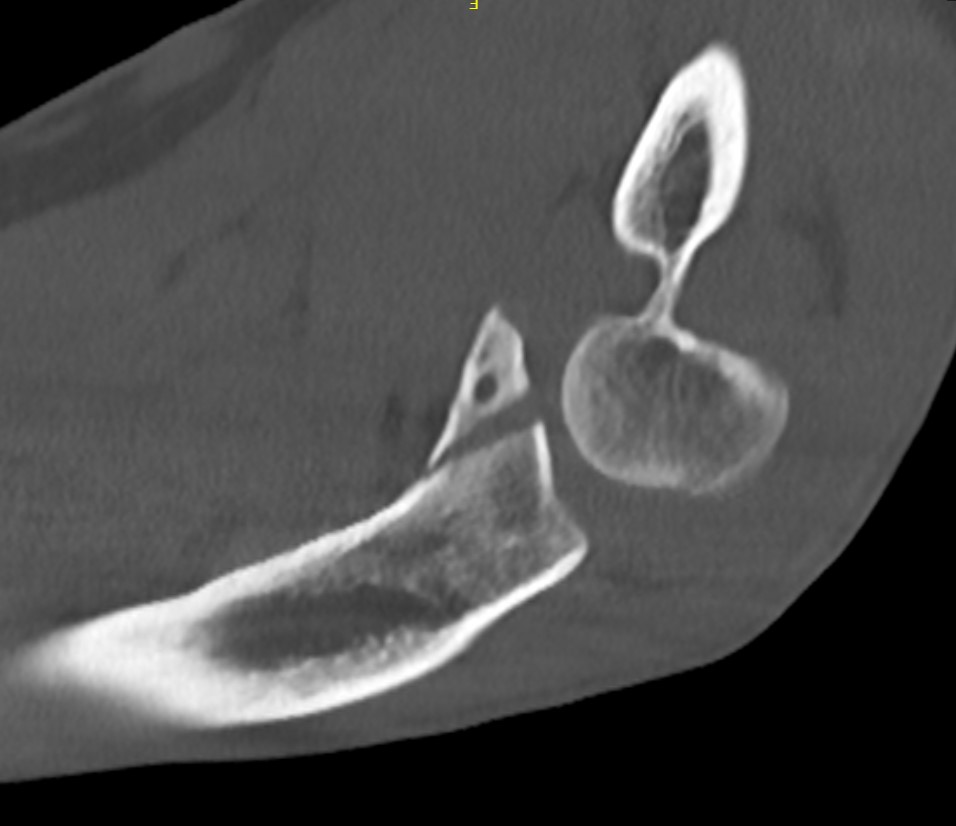
Radial head fragment nonunion
Results
- 56 patients with ORIF radial head
- 30 Mason 2, 26 Mason 3
- 13/14 patients with comminuted Mason 3 with > 3 fragments had poor outcome
- 15/15 patients with simple Mason 2 had good outcomes
- best results with 3 or fewer fragments
Radial Head Resection
Indication
Elderly patient
Coronoid intact
Contra-indication
Elbow dislocation
LCL / MCL / Interosseous membrane disrupted
Complications
Proximal radius migration
DRUJ instability and pain
Valgus instability elbow
Arthritis (deceased SA, increased contact stresses)
Results
- 26 patients < 40 treated with radial head resection
- minimum 15 year follow up
- 81% no elbow pain
- good or excellent results 92%
- all had xray evidence of arthritic change
- increased valgus / carrying angle in all
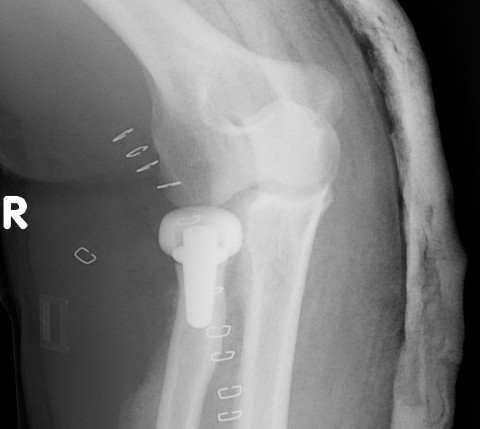
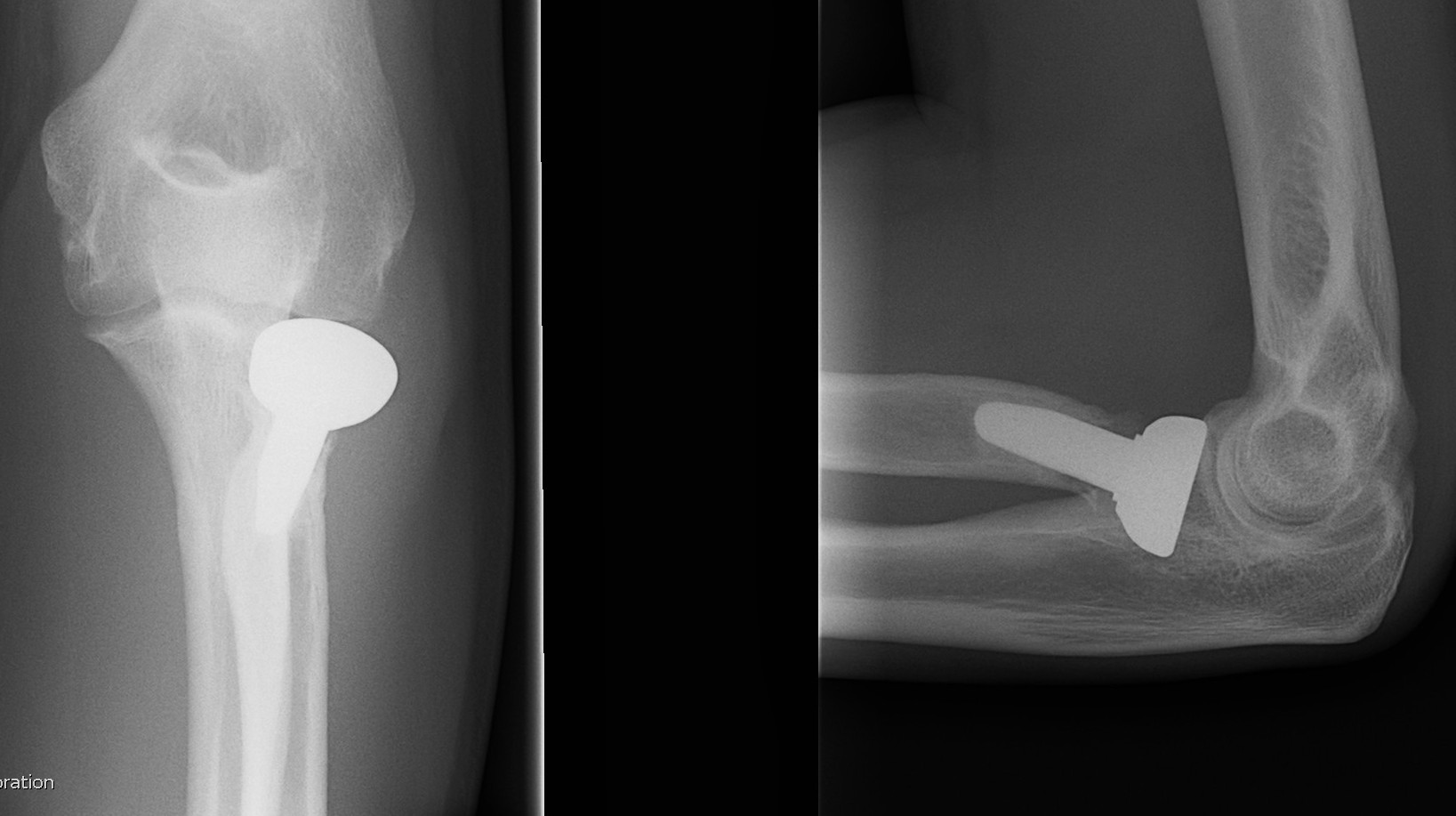
Radial Head Arthroplasty (RHA)
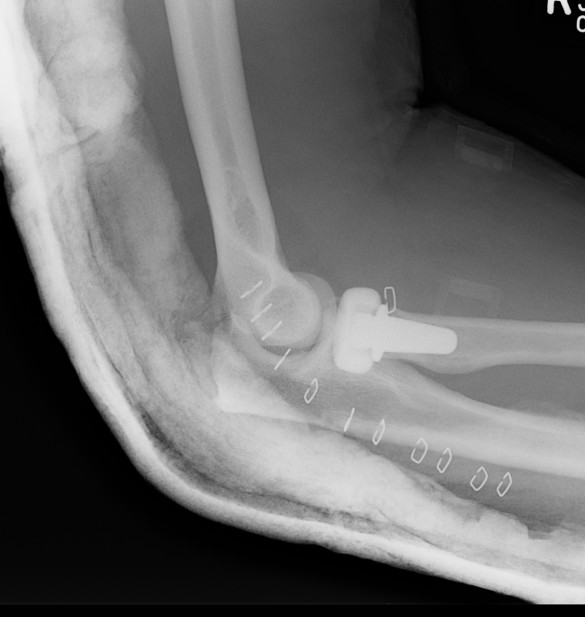
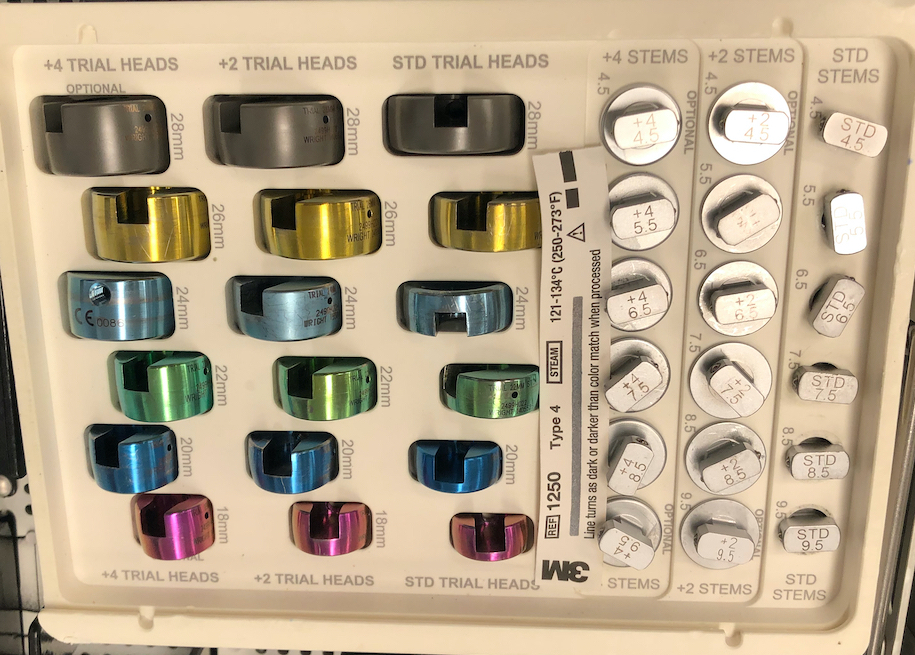
Options
Cobalt chrome / pyrocarbon / titanium
Modular
- allows various sizes of head diameter / thickness
- various stem sizes
- collars to build up radial neck if required
Press fit
- 16 press fit RHA
- 81% survival at 2 years
- high rates of lucent lines and subcollar osteolysis

Loose fit
Loose fit allows stem to rotate in medullary canal

Loose fit RHA
Overstuffing
Landmarks
1. Sigmoid notch of ulna

2. Gapping lateral ulno-humeral joint line
- cadaveric study
- increased medial ulno-humeral joint line gapping with overlengthening of 6 or 8 mm
- increased lateral ulno-humeral joint line gapping with overlengthening of 2 mm
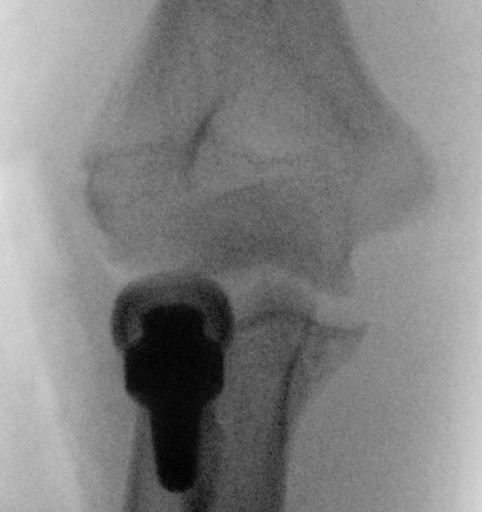
Increased lateral ulnohumeral joint space
Technique Modular Titanium Radial Head Arthroplasty
AO Surgery Reference Radial head arthroplasty
Vumedi Evolve Radial Head arthroplasty

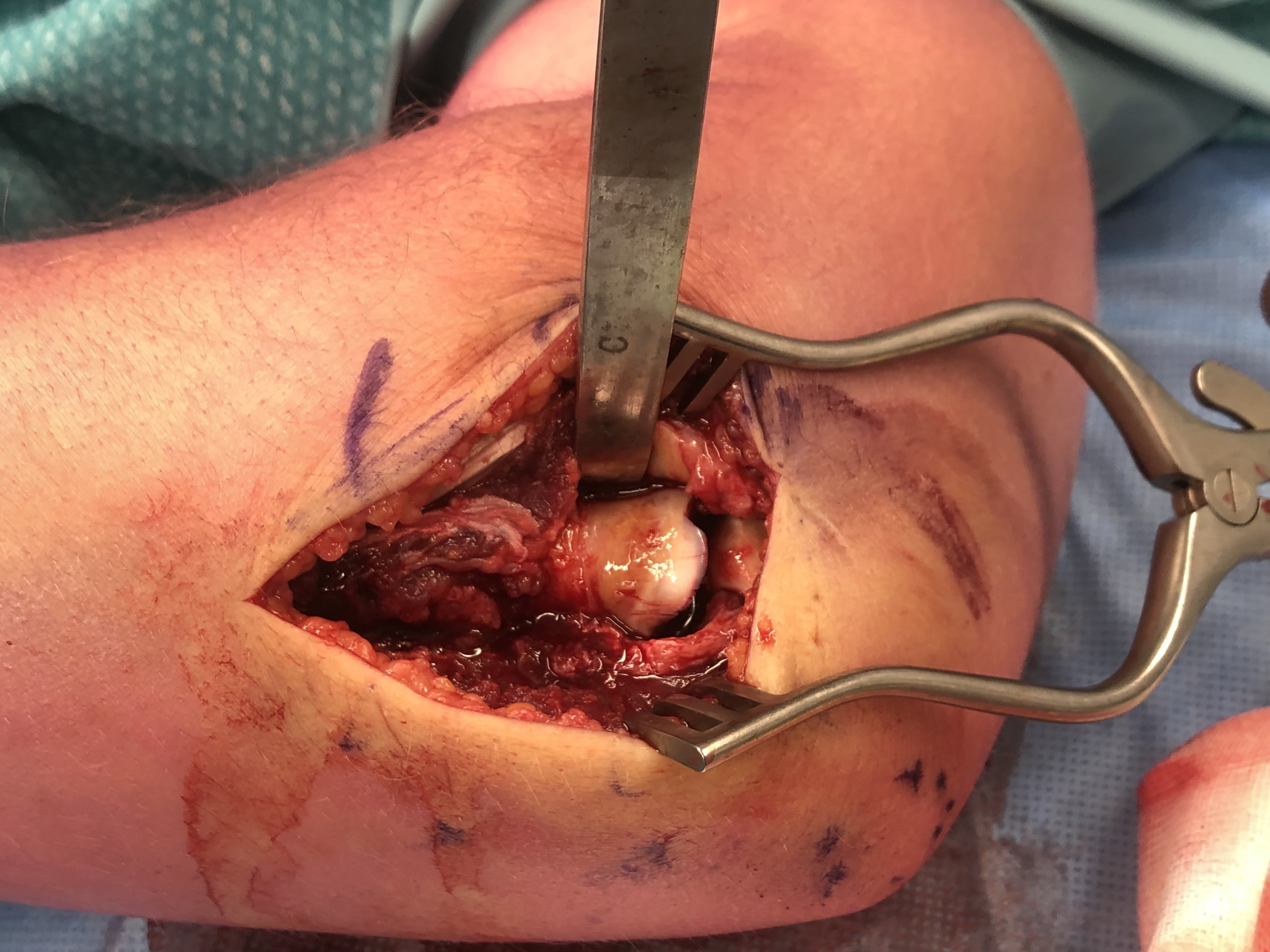
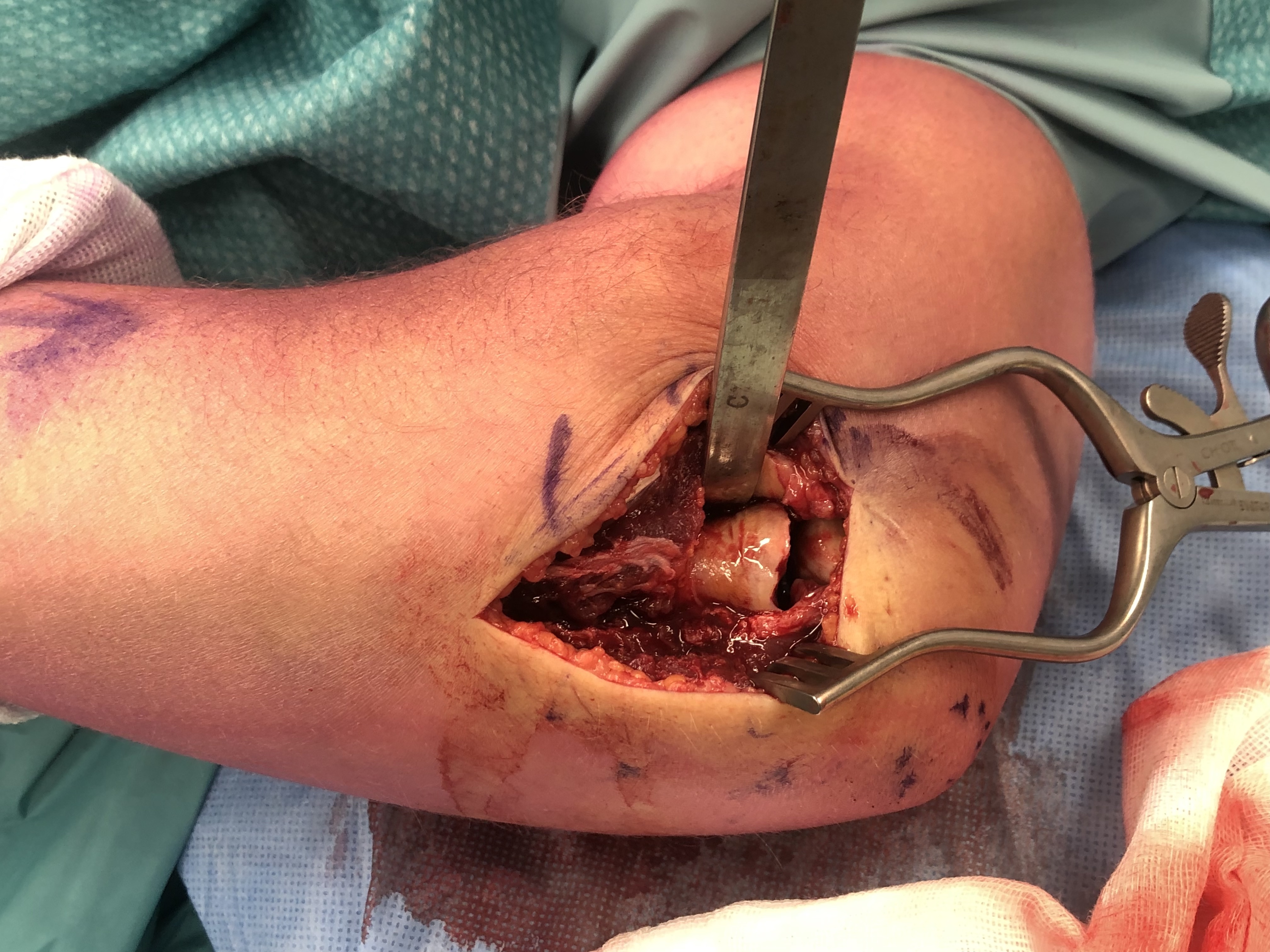
Lateral approach to elbow
- open capsule
- divide annular ligaments
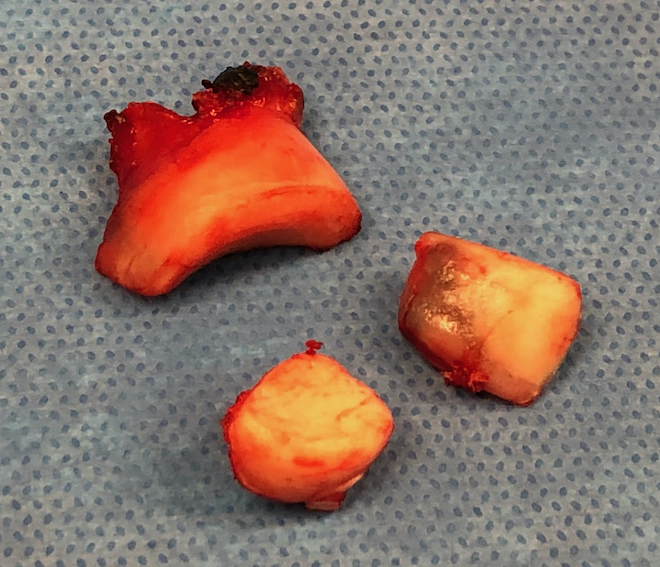
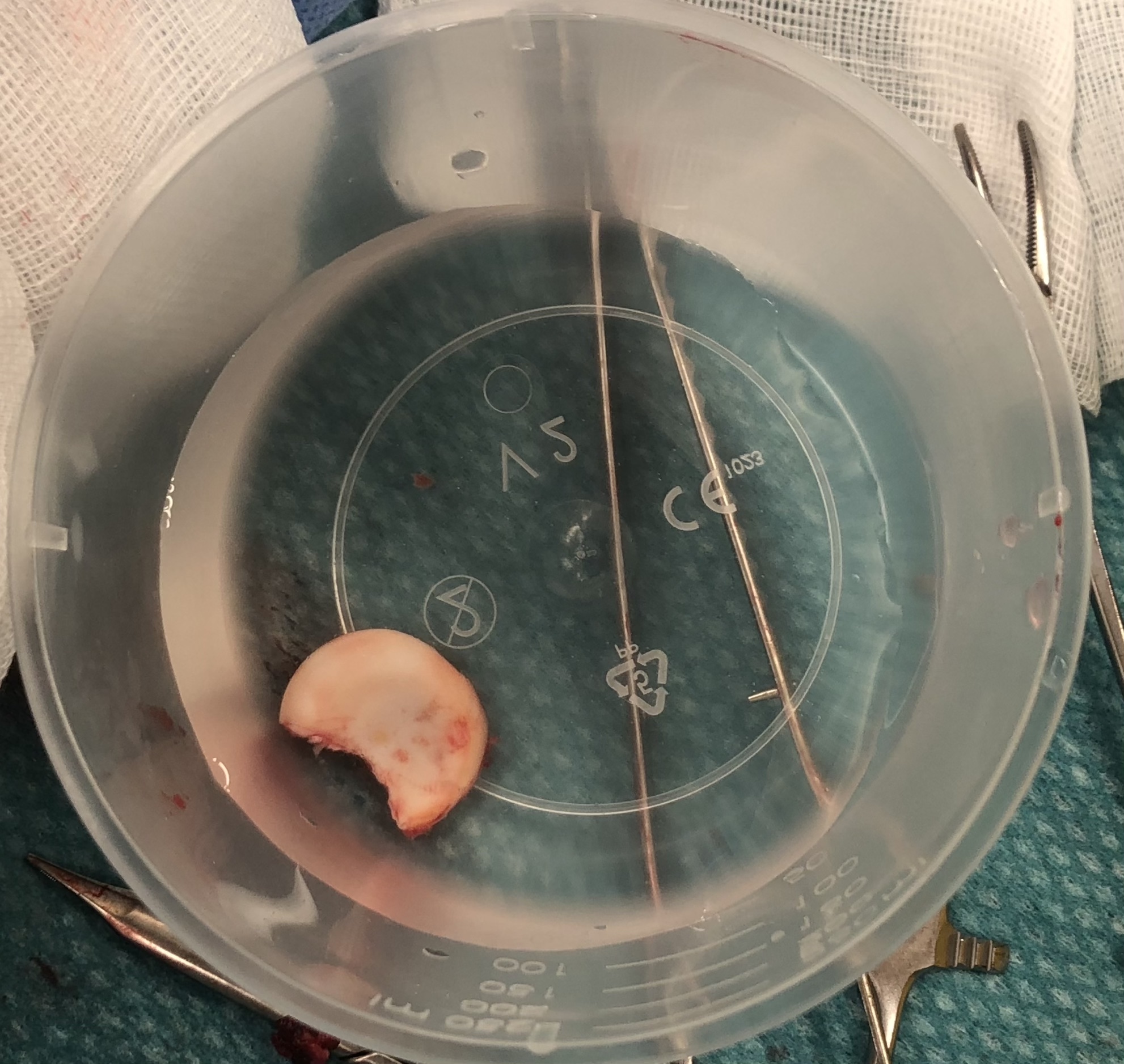
Excise radial head fragments
- use fragments to estimate diameter and thickness of radial head
- if in doubt, downsize
Deliver radial neck
- Hohman retractor safe posteriorly
- do not place Hohman retractor anteriorly to protect PIN
Ensure neck cut flat
- avoids maltracking
- need 60% contact of radial neck with prosthesis
Insert trial broaches into neck
- avoid valgus / causes maltracking
- insert trial head diameter and neck length
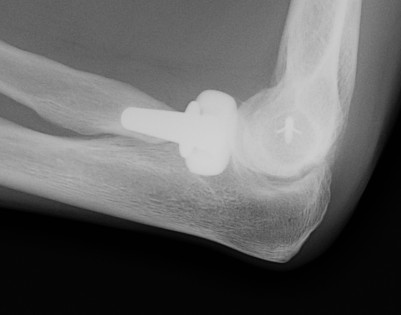
Check xray to ensure not overstuffed
- lesser sigmoid notch of ulna
- symmetry of ulnohumeral joint
Range elbow
Insert head and neck as one piece
Careful closure of annular ligament
Repair LCL as needed with suture anchors in centre of lateral capitellum
Results
- systematic review of radial head arthroplasty
- 30 articles with 727 patients
- 8% revision rate
- Mayo Elbow Performance Score: 85% good or excellent
- systematic review of minimum 8 year outcomes of RHA
- 10 studies with 432 elbows
- 86% minimal or no pain
- 9% loosening
- 27% degenerative change
- 3% RHA revision rate
- 15% removal of implants
- 450 cases
- revision rate 18% for terrible triad versus 10% isolated cases
- increasing radial head diameter associated with increasing revision rate
Complications
Stiffness
Over lengthening / over stuffing
Heterotopic ossification

Heterotopic ossification
Pain
Malposition
Loosening
Infection
Radiocapitellar OA
Radial arthroplasty malposition
Instability
Coronoid / LCL / MCL injuries
Radial neck fracture



Indications for surgery
> 30o angulated
Displacement
Approach
Incision annular ligament
Elevate supinator with arm pronated
Surgical Options
Headless Compression Screws
Low profile T plate
Intramedullary wire
Radial head replacement
Headless compression screws
Proximal to distal
Cross fracture site




T plate in safe zone



Technique
Distal limit is bicipital tuberosity
- pre-contoured low profile plates
- may need to lag articular surface first
- check ROM intra-operatively
- plates often bulky and may limit ROM
