Epidemiology
Sciatica > 2/52 1.6%
M:F = 1:1
Most common L4/5
L5/S1 inherently stable
Risk factors
Sedentary lifestyle
Smokers
Frequent driving
Heavy lifting
Anatomy
Annulus Fibrosis
- circumferential, multilayered rim
- type 1 collagen fibres at 30o to horizontal
- peripheral nerve endings
- high resistance to torsional and axial loads
Nucleus pulposis
- hydrophilic PG + 70% water
- type 2 collagen
- resist axial compression
Avascular
- nutrients diffuse from the end plate
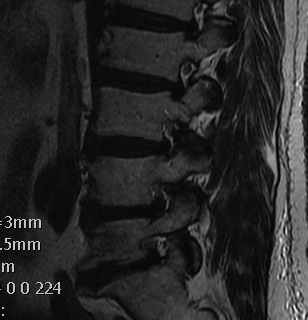
Wiltse Classification
1. Bulge
- annulus diffusely extends beyond the plane of the disc space
- annulus intact / nil focal protrusion
2. Protrusion
- focal bulging within margin of annulus
- diameter of base is greater than diameter of tissue displaced beyond disc space
3. Extrusion
- under PLL
- mass of discal tissue of greater diameter than the aperature through which it has passed


4. Sequestration
- free disc in canal
- fragment with no continuity with tissue in disc of origin

Anatomical Classification
1. Central

2. Lateral Recess / Posterolateral
- between dura and foramina
- anterior: disc (annulus) and vertebral body
- posterior: facet joint, lamina, ligamentum flava
- lateral: foramen, L5 pedicle

3. Foraminal
- anterior: body of L5, L5/S1 disc
- posterior: pars, apex of superior facet of S1
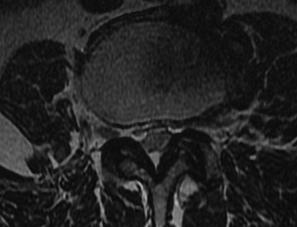
4. Extra- Foraminal / Far Lateral
Pathophysiology Nerve Root
Compression
Poorly resistant to compression
- dural sheath instead of perineurium
- tethered between dura and foramen
- compression impairs blood flow to nerve
Problem
- asymptomatic nerve compressions
- studies suggest that normal nerve roots do not generate pain when compressed
Biochemical
Chemical factors
- make nerve root more susceptible to effects of compression
Anatomy
L4/5
- traversing nerve root is L5
- exiting nerve root is L4
Posterolateral disc
- compresses traversing nerve i.e. L4/5 disc hits L5 nerve root
- this is most common situation
Foraminal disc
- compresses exiting nerve root i.e. L4/5 disc hits L4 nerve root
- require partial medial facetectomy / stand on opposite side of table
Far Lateral / Extra-foraminal disc
- compresses nerve root already exited i.e. L4/5 disk hits L4 nerve root
- Wiltse approach or complete facetectomy / follow nerve out
Symptoms
Typical patient 20-45 year old male
Pain
- leg in dermatomal distribution
Neurology
- numbness / parasthesia / weakness
Cauda Equina Syndrome
- saddle anaesthesia / urinary incontinence / weak EHL
Signs
Tension signs
1. SLR / Straight leg raise / Lasegue's Sign
- elevate leg from hip with knee straight
- reproduce pain below knee
- L5 / S1 nerve roots
Deville et al Spine 2000
- meta-analysis
- SLR very sensitive 90% but lower specificity 26%
- crossed SLR low sensitivity 29% but more specific 88%
2. Femoral nerve stretch test
- patient prone, knee flexed, extend hip
- reproduces pain
- L4 nerve root
Neurology
| Pain | Sensation | Weakness | Reflex | Test | |
| L2 | Lateral thigh | Lateral thigh | HF | ||
| L3 | Medial knee | Medial knee | Quads | ||
| L4 | Anteromedial knee | Medial Malleolus | T Ant | Knee Jerk | Femoral Stretch |
| L5 | Dorsum foot | First webspace | EHL | SLR | |
| S1 | Sole / lateral foot | Sole / lateral foot | FHL | Ankle Jerk | SLR |
DDx L4 nerve root
- CPN / DPN palsy
- test peroneals, tibialis posterior
DDx L5 nerve root
- CPN / DPN / Sciatic palsy
- test peroneals / abductors
DDx S1 nerve root
- tibial nerve
- test tibialis posterior
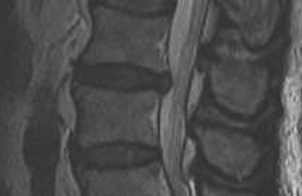
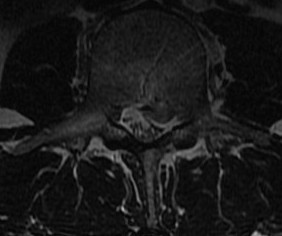
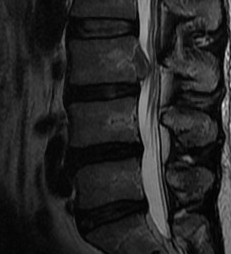
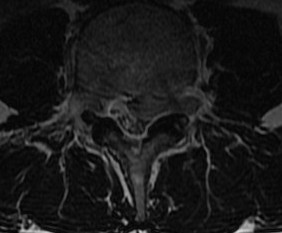
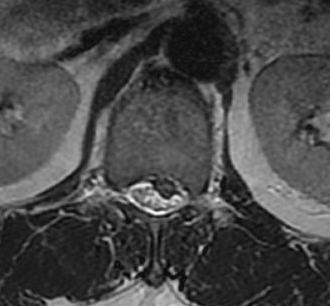
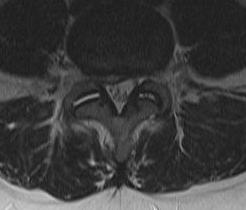
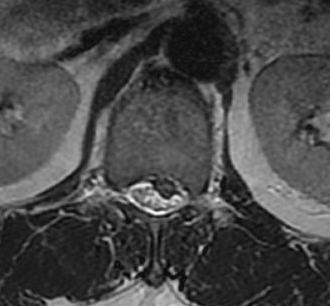
MRI
T2 Sagittal - myelogram

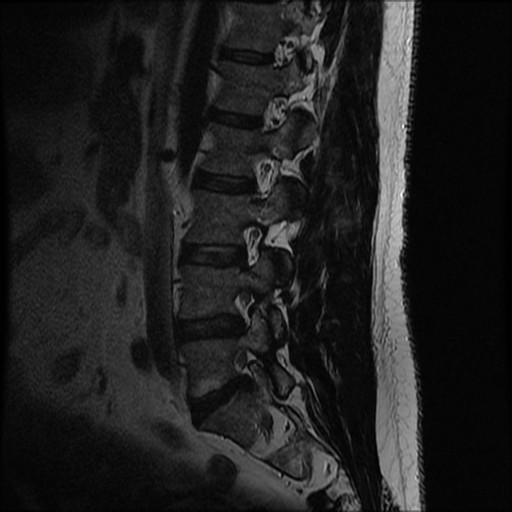

T1 Axial - see nerve root against white fat
DDx
Infection / Tumour / Fracture
Management
Non-operative Management
NHx
Recovery
- 80% improve after 6/52
- 90% improve after 3/12
- 95% improve after 6/12
Weakness just as likely to resolve as pain
Results Operative v Nonoperative
Peul et al BMJ 2008
- RCT of conservative treatment v microdiscectomy
- symptoms 6 - 12 weeks
- earlier symptomatic relief in surgical group
- no difference at one or two years
Options
Medications
- NSAIDs / opiates / steroids / tricyclic antidepressants
Physiotherapy / lumbar stabilisation exercises
Traction
Chiropractic manipulation
Epidural steroids
Price Health Technol Assess 2005
- multicentred RCT placebo control
- 220 patients with unilateral sciatica
- minimal and transient value over placebo at 3 weeks
- no difference after 6 weeks
- not cost effective / drain on resources
Arden et al Rheumatology 2005
- WEST study
- exactly the same findings
Transforaminal CS / Nerve Root Injections

Riew et al JBJS Am 2000
- RCT of patients with unilateral nerve root compression
- all considered suitable for operative intervention
- effectively prevented need for surgery in more than half of the patients
- LA + steroid more effective than LA alone
Operative Management
Absolute Indications
Cauda Equina Syndrome
Relative Indications
Failure of non operative treatment
Severe debilitating anatomical leg pain
Progression neurological deficit
Prediction of good operative outcome
6/6 Nachemson
1. Leg > back pain
2. Symptoms consistent with root irritation
3. Signs consistent with root irritation
4. Tension signs / positive SLR
5. Imaging consistent with Symptoms & Signs
6. Pain > 6 weeks
Options
Chemonucleolysis
Standard Discectomy
- open
- microdiscecotmy
Percutaneous / Endoscopic Discectomy
Chemonucleolysis
Mechanism
- chymopapain dissolves nucleosus pulposis
- older technique largely out of favour
Results
Muralikuttan et al Spine 1992
- RCT of discectomy v chemonucleolysis
- inferior short term results with chemonucleolysis
- no difference at one year
Discectomy
Advantage
- suitable for noncontained disc
Results
Dewing et al Spine 2007
- prospective followup of 183 single level lumbar discectomies
- average age 27
- 85% satisfied with surgery
- recurrent disc herniation in 3%
- better outcomes in L4/5 than L5/S1
- better outcomes in sequestered / extruded discs than contained discs
- poorer outcomes in smokers and patients with predominance of back pain
Righesso et al Neurosurgery 2007
- RCT of open v microdiscectomy
- no difference in outcome
- longer scar and inpatient stay in open group
- longer surgical times in microdiscectomy
Percutaneous Discectomy
Indications
- contained disc
Technique
- image guidance / endoscopic techniques
- interlaminar or transforaminal
- discectomy with cutting / suction probe
Advantage
- minimal scar
- rapid recovery
Results
Ruetten et al Spine 2008
- RCT of endoscopic interlaminar and transforaminal v microdiscectomy
- 82% relief of leg pain, no difference in each group
- 6% recurrence, no difference in each group
- reduced back pain and complications with improved rehab in endoscopic group
Complications Discectomy
Wrong level surgery
Neural injury
- paraplegia 1: 25 000
- nerve root injury
- cauda equina 0.2%
Dural tears
A. Intraoperative Management
- head down
- stop ventilating / hand ventilate / anaesthetic valsalva
- ensure free abdomen
- CSF can make nerve root in danger / protect with patty
- attempt primary repair with 6.0 prolene non cutting needle
- supplement with Tisseel glue
- +/- fat graft / thoracolumbar graft
- subfascial drain
- bed rest 2 days
B. Postoperative CSF leak
- ensure no meningitis symptoms
- glucose / microscopy test to confirm
- adequate fluids / head down / quiet room / bed rest
- antibiotics controversial
- MRI: small leak or large leak
Non operative Management
- insert drain below conus
- decreases CSF pressure
- bed rest / leave drain for 5 - 7 days
Operative Management
- failure nonoperative / large leak
- thoracolumbar fascia / synthetic graft repair
Incomplete decompression / failure to relieve symptoms
Infection 2%
Thromboembolism 1%
Arachnoiditis / Intradural fibrosis
Incidence 5%
MRI changes
1. Central root clumping
2. Empty sac appearance
3. Soft tissue mass in subarachnoid space
HNP recurrence
Incidence
- life long 6 - 7%
- second time 50%
- third time 90%
Investigation
- gadolinium MRI
- scar enhances but recurrent HNP does not
Management
- disc resection +/- fusion
- Retrospective cohort study 733 lumbar discectomies
- 12% recurrence rate over 5y
- Smoking was the major independent risk factor, HR 2.12
