Definition
Spinal cord dysfunction caused by extrinsic compression of the cord or its vascular supply
Epidemiology
Commonest cause of atraumatic spinal cord injury
C5/6 commonest level
Pathophysiology
A. Congenital / developmental stenosis
B. Degenerative
1. Degeneration - Herniated nucleus pulposis (HNP), osteophytes from facet and uncovertebral joints
2. Instability / spondylolithesis
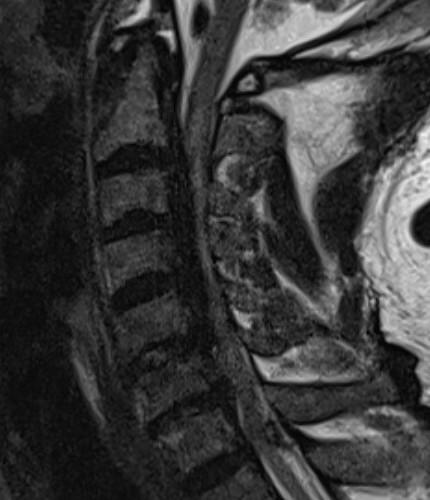
3. Kyphosis - stretches spinal cord over posterior vertebral bodies and discs
4. Ossification of PLL (OPLL) - more common in certain Asian populations i.e. Japanese
- MRI of 458 patients with myelopathy
- 90% spondylosis
- 60% enlargement of ligament flavum
- OPLL 10%
- spondylolisthesis 10%
- single level disc pathology 10%
History
Neck pain
Difficulty walking / unsteadiness on feet
Weakness
- upper > lower limb
- distal > central
- clumsiness of hands, difficulty with fine motor function
Parasthesia - upper limb, global, non dermatomal
Bladder dysfunction uncommon
Central cord syndrome (boneschool page)
- after an acute injury or fall
- typically hyperextension
- acute flaccid paralysis of upper limbs
Examination
Upper motor neuron (UMN) signs below lesion
Lower motor neuron (LMN) signs at level of lesion
Ataxia
- wide based gait
- unable to heel toe
Poor proprioception
- finger escape sign - deficient adduction or extension of ulnar digits of affected hand
- Romberg Positive
Hyper-reflexia
- Hoffman Reflex - flexion of ipsilateral IPJ of index and thumb when long finger DIPJ flexed
- Inverted Brachioradialis Reflex - spontaneous flexion of digits when BR reflex elicited
- Babinski Reflex
Nurick classification system
Grade 0: Signs or symptoms of root involvement but without evidence of spinal cord disease
Grade 1: Signs of spinal cord disease but no difficulty in walking
Grade 2: Slight difficulty in walking, which did not prevent full-time employment
Grade 3: Difficulty in walking preventing fulltime employment / ability to do housework
Grade 4: Able to walk only with someone else’s help or with the aid of a frame
Grade 5: Chair-bound or bedridden
DDx
Need to exclude other causes of neurological symptoms
- multiple sclerosis / motor neuron disease
- stroke / AVM / tumour / hydrocephalus
- metabolic or alcoholic encephalopathy
- syringomyelia / Tabes dorsalis
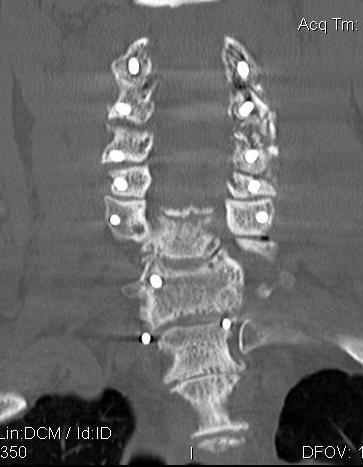
X-ray
Degenerative changes - C5/6 commonest level followed by C6/7
Alignment - lordosis v kyphosis


Ossification PLL

Flexion / Extension views show instability
- > 3 o
- > 11 mm
Torg-Pavlov's Ratio (A/B)
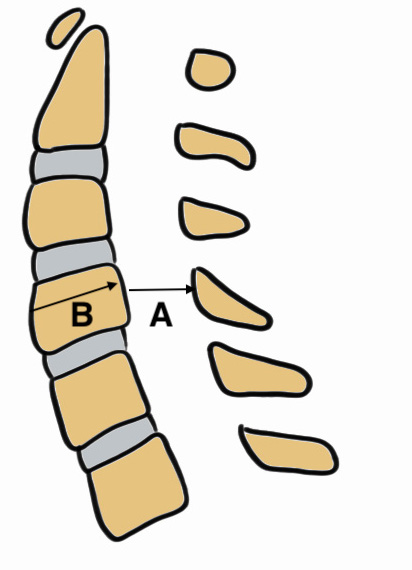
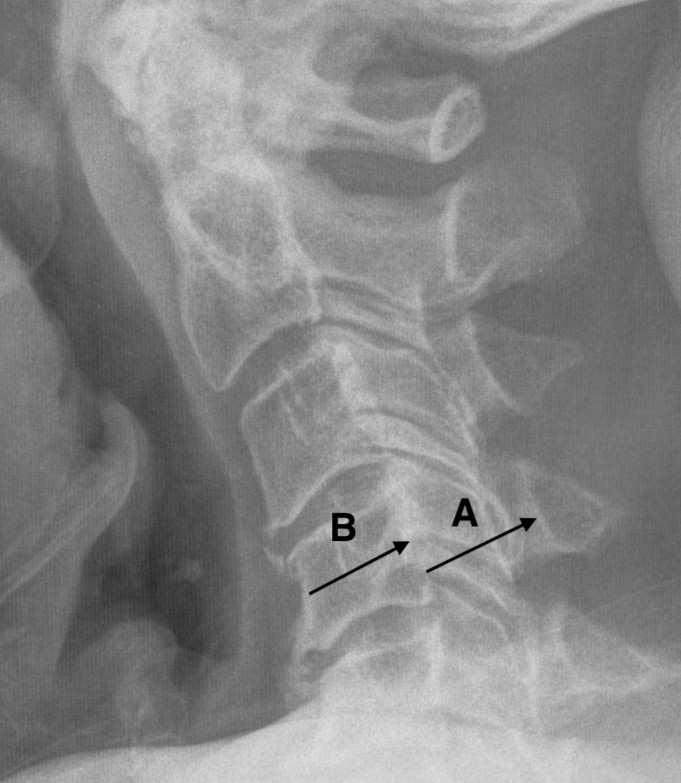
AP diameter of spinal canal (A) divided by the AP diameter of body (B) at same level
- should be 1.0
- < 0.8 is narrowed and stenotic
MRI
1. Space available for cord (SAC)
- Sagittal diameter of spinal canal - sagittal diameter spinal cord
- normal (17mm)
- relative (13mm)
- absolute stenosis (10mm)
Reduced by disc / osteophytes / OPLL / deformity / instability
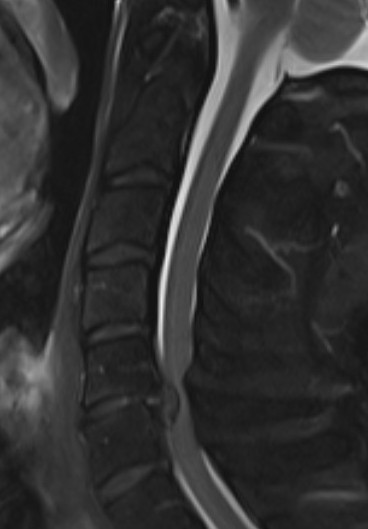


Single level stenosis Double level stenosis Multi-level stenosis
2. Compression Ratio
- banana cord
- divide the smallest AP diameter by largest transverse diameter at same level of spinal cord
- ratio of < 0.4 after decompression particularly with myelopathy > 6 months has poor prognosis
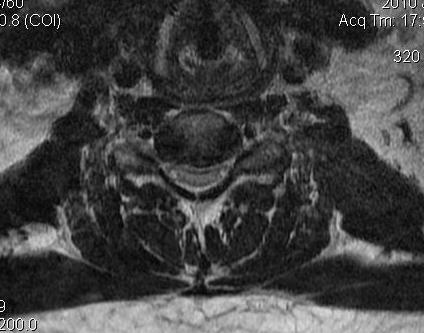
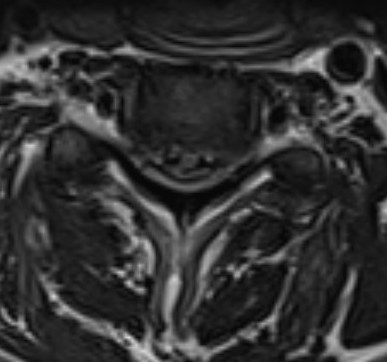
Banana shaped cord
3. Cross sectional area of spinal cord
- < 30 mm2 poor prognosis
4. Evidence of cord edema / spinal cord damage
- often seen after acute injury in setting of stenosis
- best seen on STIR MRI


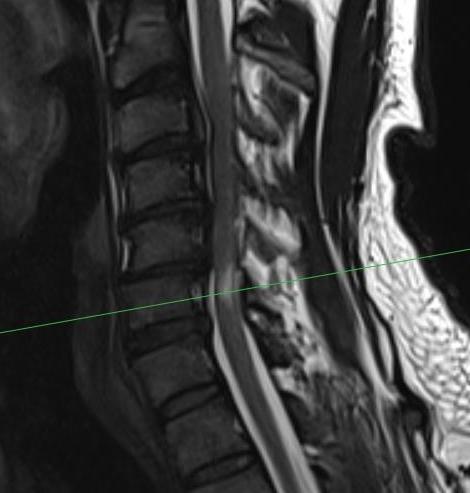
Spinal cord edema / injury
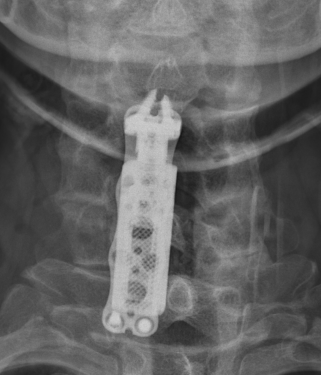
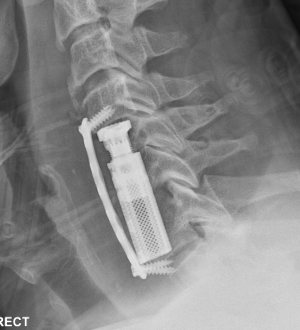
CT
Helps distinguish disc from osteophytes
- soft v hard disc
- diagnose OPLL

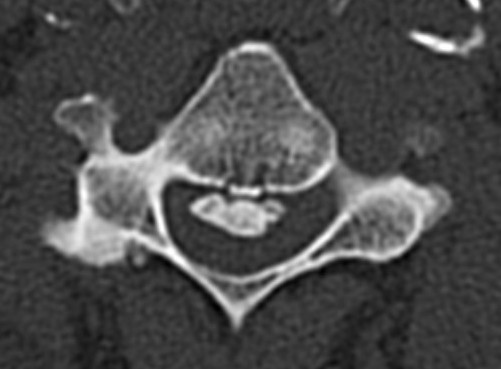
OPLL on CT

MRI and CT in same patient with OPLL
Natural History
Wilson et al Spine (Phila Pa 1976) 2013
- 8% of asymptomatic patients with MRI changes will experience myelopathy at 1y
- 23% at 44 mo
Management
Non operative
Simple analgesics - NSAIDS
Physiotherapy with isometric strengthening
Traction and manipulation contraindicated
Counsel them to the risks of trauma
Operative
Absolute Indications
Progressive neurological deficit
Relative indications
Debilitating symptoms
Acute central cord syndrome
Compression parameters on imaging
- compression ratio < 0.4
- transverse spinal cord diameter of < 40 mm2
- increased signal intensity of cord on T2 of MRI
Lumbar and cervical stenosis
The patient with cervical and lumbar stenosis
- should have the cervical spine decompressed first
- risk of intubation damage to cervical spine
- reduces need for lumbar surgery
- leg symptoms may improve after the cervical decompression
Preoperative Considerations
Positioning should avoid hyperextension of the cervical spine
- may need awake fibreoptic intubation
Options
Anterior approach
Techniques
- ACDF
- corpectomy
Advantage
- restore or maintain lordosis
- disc removal
Disadvantage
- more difficult to decompress neural foramina
- difficult in setting of OPLL
- swallowing trouble in elderly patients
Posterior approach
Techniques
- laminectomy and fusion
- laminoplasty
Indication
- OPLL
- severe multilevel stenosis > 3 levels
Contra-indication
- kyphotic deformity
Results
Anterior versus Posterior surgical approaches
- 264 patients in prospective study
- 169 anterior approach and 95 posterior approach
- anterior approach patients younger and with milder myelopathy
- equivalent efficacy
Laminoplasty versus laminectomy / fusion
- prospective study of 266 patients
- 100 laminoplasty and 166 laminectomy / fusion
- minimal statistical difference between two groups
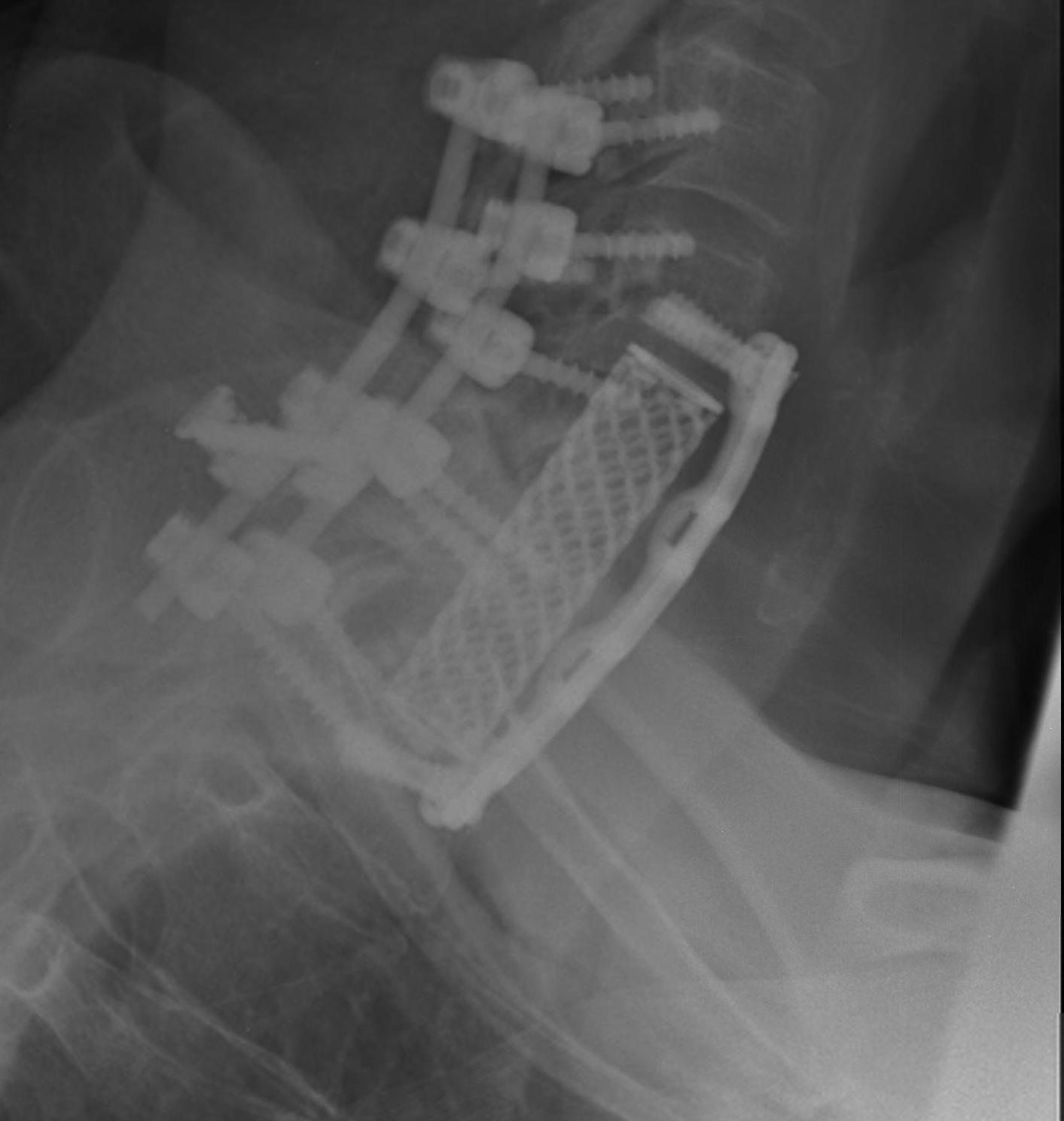
ACDF versus corpectomy
- multilevel ACDF versus anterior cervical corpectomy and fusion
- meta-analysis of 8 studies and 878 patients
- ACDF had better postoperative angles and fusion rates, and reduced blood loss and complications
Ossification of Posterior Longitudinal Ligament (OPLL)
- prospective study of 135 patients with OPLL undergoing decompression
- no difference in outcomes compared with those without OPLL
- higher risk of complications
ACDF



Indication
Anterior cord compression
Single or double level compression
Kyphotic deformity
Advantages
Removes entire disc
Maintain / restore lordosis
Disadvantages
Difficulty decompressing the nerve roots in foramen
Difficult to decompression vertebral bodies
Relatively contra-indicated with OPLL
Corpectomy
Concept
Can remove body with disc above and below and decompress multiple levels



Indication
- multilevel disease
- soft and hard disc causing compression
- kyphotic deformity
Complications
Risk of graft extrusion / hardware failure - fewer points of fixation
Laminectomy and Fusion


Concept
Posterior decompression is an indirect technique
- requires posterior shifting of the cord in the thecal sac
Indications
Lordotic cervical spine / no kyphotic deformity
Ossification of PLL
- dura may be adhered
- high risk of irreparable dural tears with anterior approach
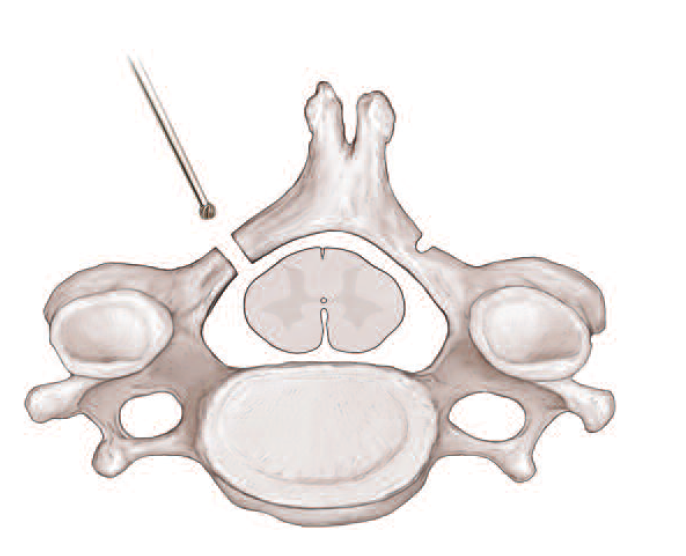
Technique
Posterior approach
- prone
- Mayfield head tongs in neutral
- protect eyes / elbows (ulna nerve) / knees (CPN)
- pneumatic compression stockings
- IDC
- infiltration of skin with adrenaline solution
Decompression
- wide laminectomy +/- foraminotomy
Instrumentation
- avoids progressive kyphotic deformity
- lateral mass screws
Complications
Postoperative instability / kyphosis
- > 50% facet resection
- avoid by fusion or laminoplasty
Increased risk wound issues
Laminoplasty
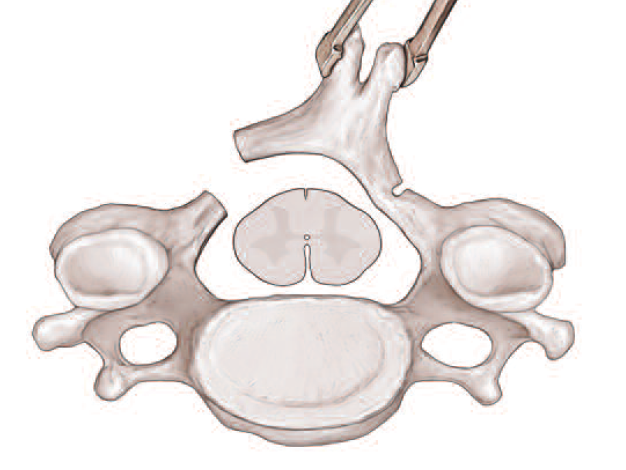
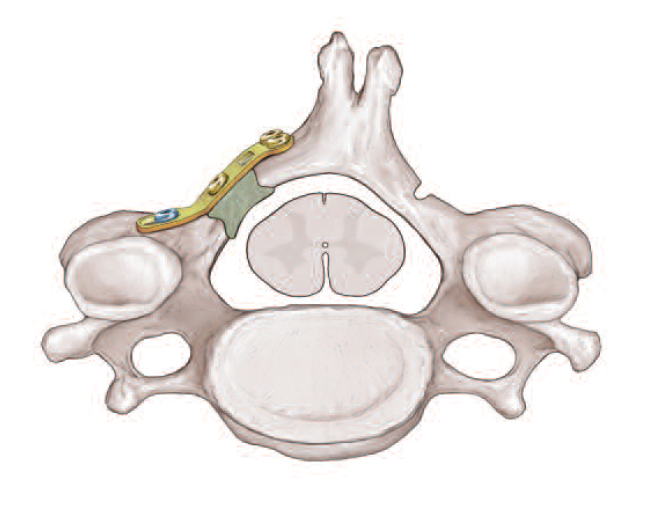
Concept
Divide lamina unilaterally and insert device to keep lamina elevated
Motion preserving
Contra-indications
Kyphotic deformity
Neck pain - otherwise need fusion
Instability
Combined anterior and posterior


Indication
Severe deformity
Poor bone quality
Instability
Complications
Fehlings et al J Neurosurg Spine 2012
- 302 patients from the AOSpine North America Cervical Spondylotic Myelopathy Study
- 30 day complication rate of 16%
- late complication rate of 4%
- worsening of myelopathy 1%
- minor cardiopulmonary event 3%, dysphagia 3%, surgical wound infection 2.3%
- higher infection with posterior approach (4.7%) than with anterior approach (0.6%)
- higher dysphagia with anterior approach (2.3%) than with posterior approach (0.9%)
- increased risk with age / operative time / combined anterior and posterior approach
Anterior approach (boneschool link)
- transient sore throat - superior laryngeal nerve
- dysphagia
- recurrent laryngeal nerve paralysis
- injury vertebral artery
- Horner's syndrome
Dural tears
Increased risk with OPLL
- fibrin glue, fascial patch
Pseudoarthrosis
Jiang et al Arch Orthop Trauma Surg 2012
- systematic review of 12 studies
- multilevel ACDF versus corpectomy
- nonunion rates for 2 level ACDF 18% and 3 level ACDF 37%
- nonunion rates for single level corpectomy 5% and for two level corpectomy 15%
C5 nerve palsy
Postoperative deltoid and biceps weakness
- associated with C5 foraminal stenosis
- 1001 cases of anterior and posterior decompression
- overall C5 palsy incidence of 5%
- incidence 1.6% anterior approach and 8.6% posterior approach
- associated with older age, corpectomy, and posterior C4/5 laminotomy
- improved in 6 months of 75% of anterior approach and 89% posterior approach
- meta-analysis of 79 studies and 13,000 patients
- overall incidence 5%
- typically unilateral, more common in males
- most common in laminectomy & fusion (11%)
- lease common in ACDF (3%)
Treatment
- foraminotomy
- nerve transfer
Progressive kyphotic deformity
Associated with posterior approach without fusion
Hardware failure
