
Indications
RA
OA
AVN
Contra-indications
Infection
Charcot
Paralysis of deltoid
Torn rotator cuff
Insufficient glenoid bone stock
Requirements
1. Functioning / repairable rotator cuff
- maintain stability
- maintain centre of rotation
- early failure if cuff deficient due to rocking horse effect on glenoid component

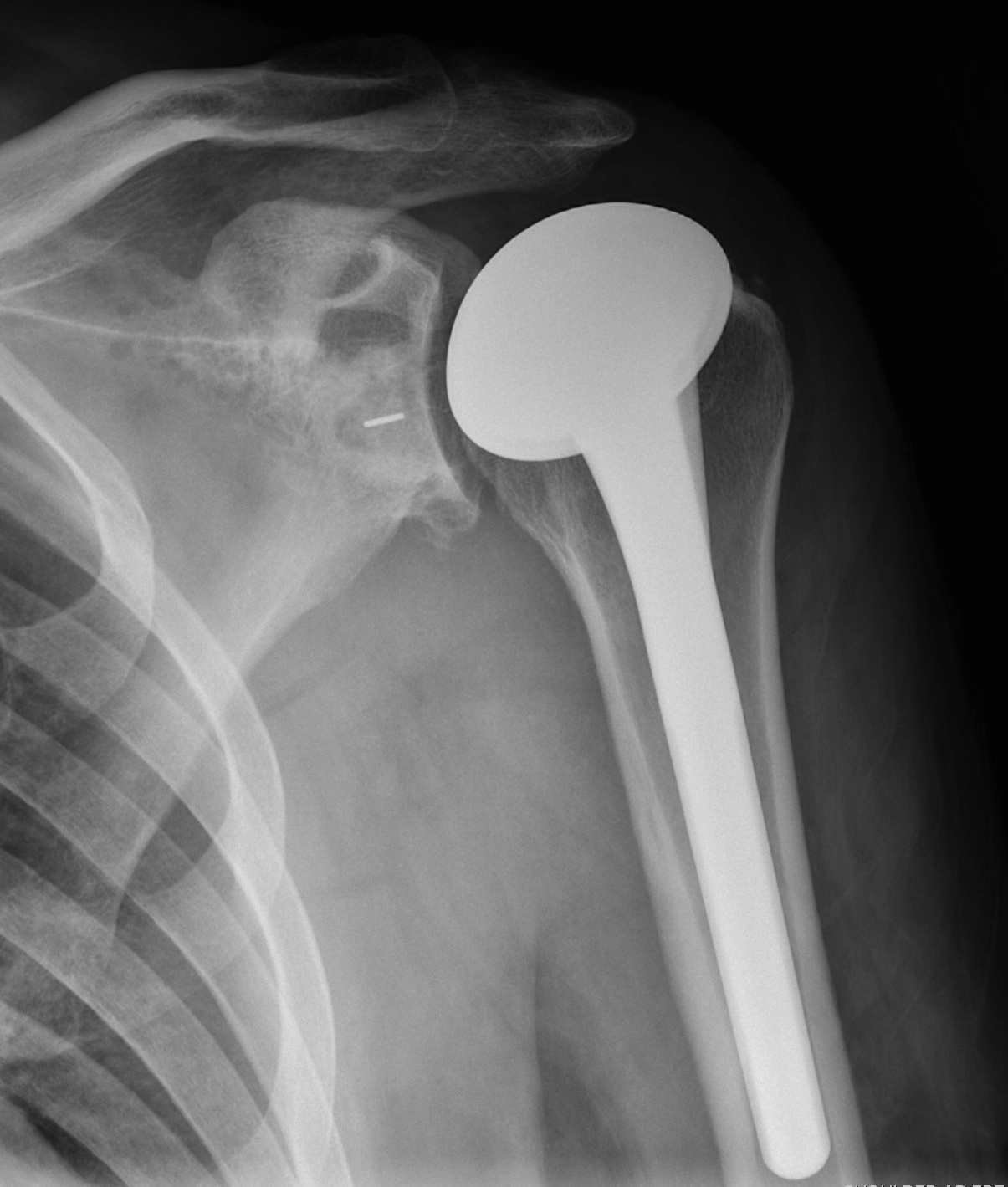
Repaired rotator cuff

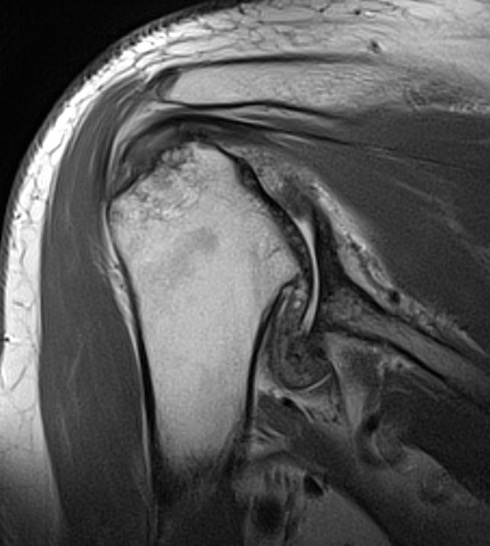
MRI demonstrating intact cuff
2. Intact Deltoid
3. Reasonable glenoid bone stock
- commonly posterior bone loss in OA
- glenoid component must be completely supported by peripheral bone rim or early failure
Anatomy
Glenoid
Pear shaped Elliptical Vault Superior inclination
Alashkam et al. Clin Anatomy 2021
- approximately 70% glenoids are pear shaped due to presence of glenoid notch anterior margin
- remainder elliptical
- glenoid height varies 30 - 50 mm (mean 35 - 40)
- glenoid width varies 17 - 40 mm (mean 22 - 30 mm)
- inclination superior 4 - 5o
Version
- CT scan 410 normal shoulders
- mean retroversion 1o +/- 3o
- wide range -9o to 13o
- increased glenoid retroversion in men > women, and in dominant arm
Humeral head and scapula
Scapula 30o anteverted from coronal plane
- humeral head retroversion mean 26o +/- 11o
- wide range -2 - 60o
- increased glenoid and humeral (both) retroversion in men > women, and in dominant arm
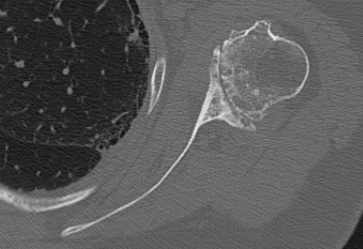
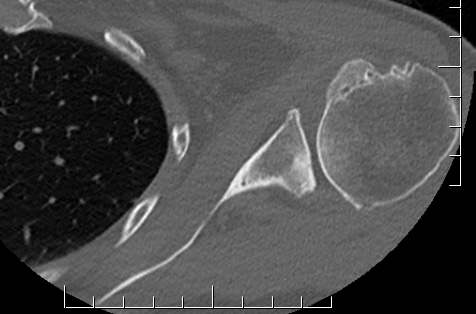
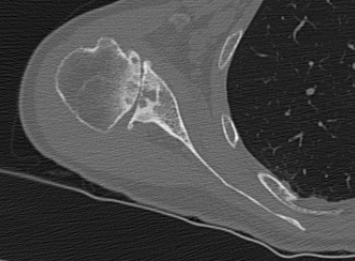
Glenohumeral OA Classification
Samilson-Prieto


Grade 2 Grade 3
Grade 1: Osteophytes < 3 mm
Grade 2: Osteophytes 3 - 7 mm with slight narrowing GHJ
Grade 3: Ostephytes > 7 mm with GHJ narrowing and sclerosis
Glenoid morphology, bone stock and version
Issues
1. What is the morphology?
2. Is there sufficient bone stock for glenoid replacement?
3. Does version need to be addressed?
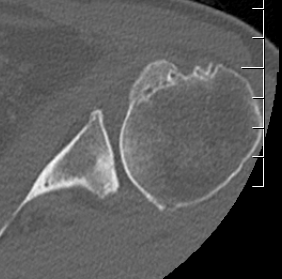
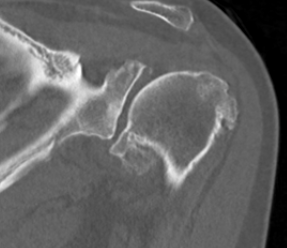
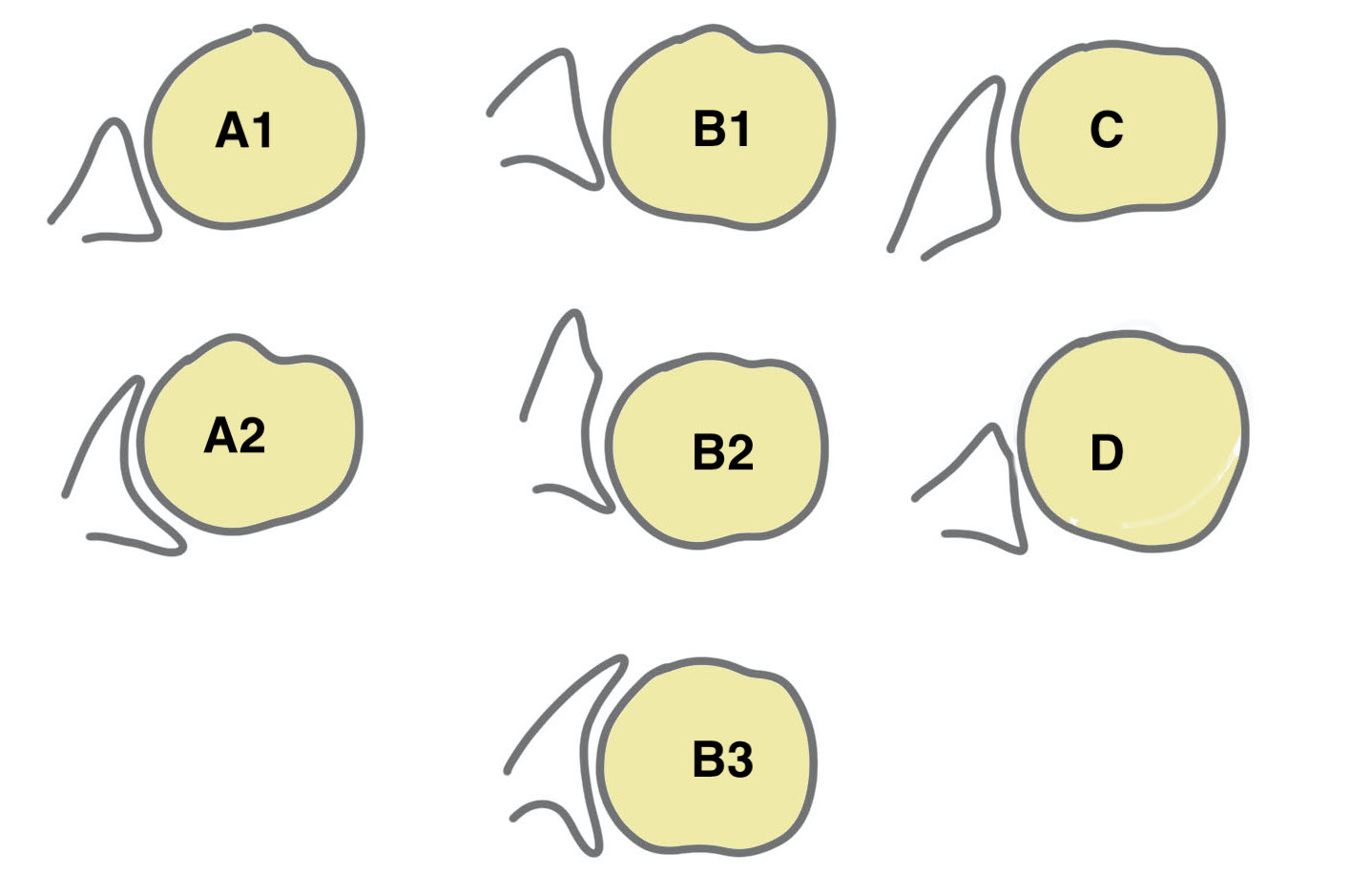
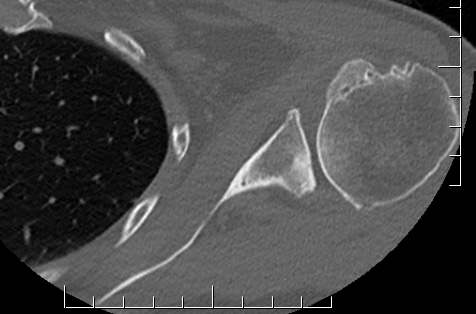
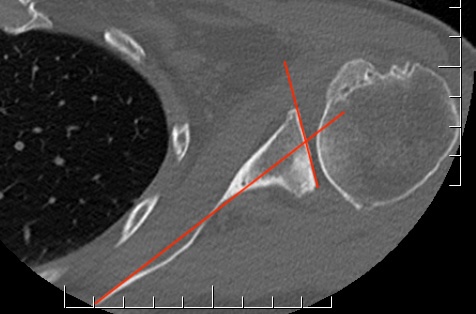
Walch classification glenoid morphology
Type A - centred humeral head, concentric wear, no humeral head subluxation
A1: minor central erosion
A2: major central erosion with humeral head protrusion
Type B - posterior subluxation of the humeral head, with biconcave glenoid and asymmetric wear
B1: narrowing of the posterior joint space
B2: biconcave glenoid with posterior rim erosion and retroverted glenoid
B3: monoconcave glenoid with > 15° retroversion or >70% posterior humeral head subluxation or both
Type C
C1: dysplastic glenoid with >25° retroversion
C2: biconcave, posterior bone loss, posterior translation of the humeral head
Type D: glenoid anteversion or anterior humeral head subluxation <40°
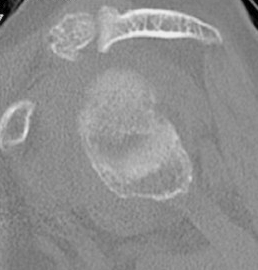
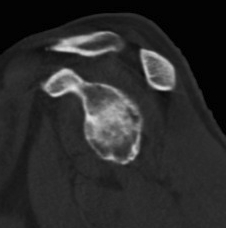
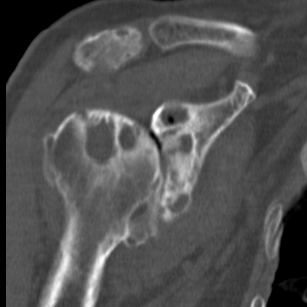
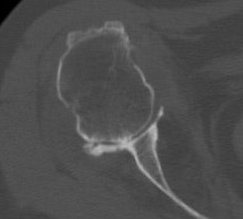
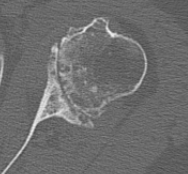
Type A2 Type B1
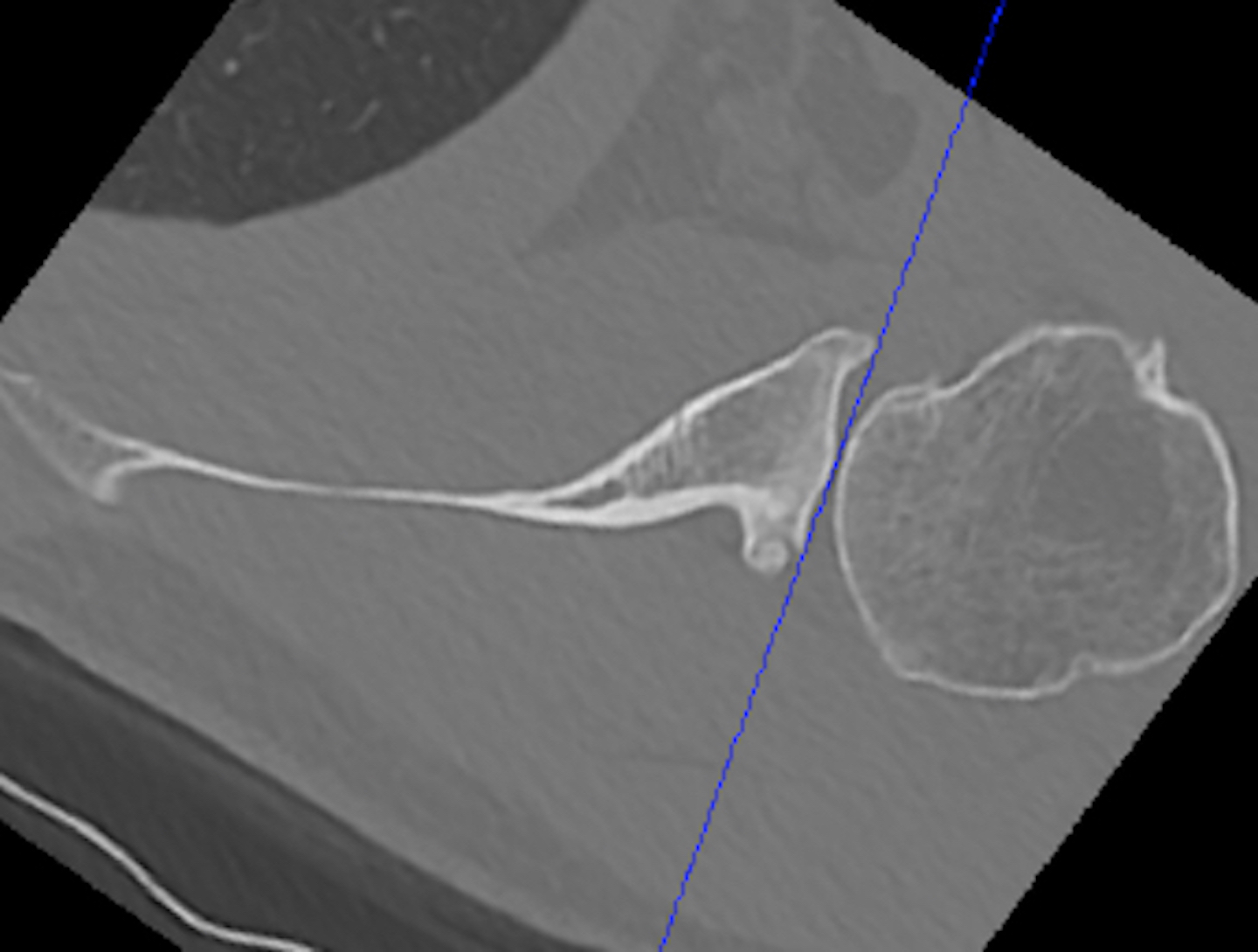
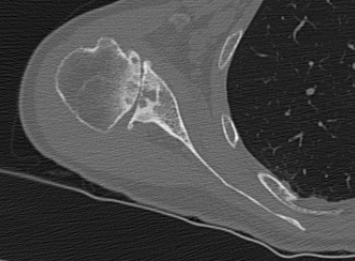
Type B2 Type B3
Type B3
Accuracy of Walch classification
- xray and CT of 100 shoulders with GHJ OA
- intra-observer reliability for xray and CT substantial (0.73)
- inter-observer reliability for xray and CT moderate (0.55, 0.52)
- CT v MRI
- largely comparable
- MRI less accurate at distinguishing between type B2 and type C
Progression over time
- 65 patients with shoulder OA with CT scans 2 years apart
- 8/42 type A progressed
- 17/19 type B1 progressed
Glenoid bone stock
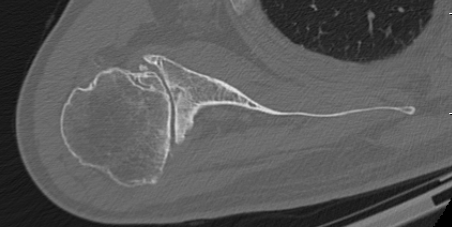
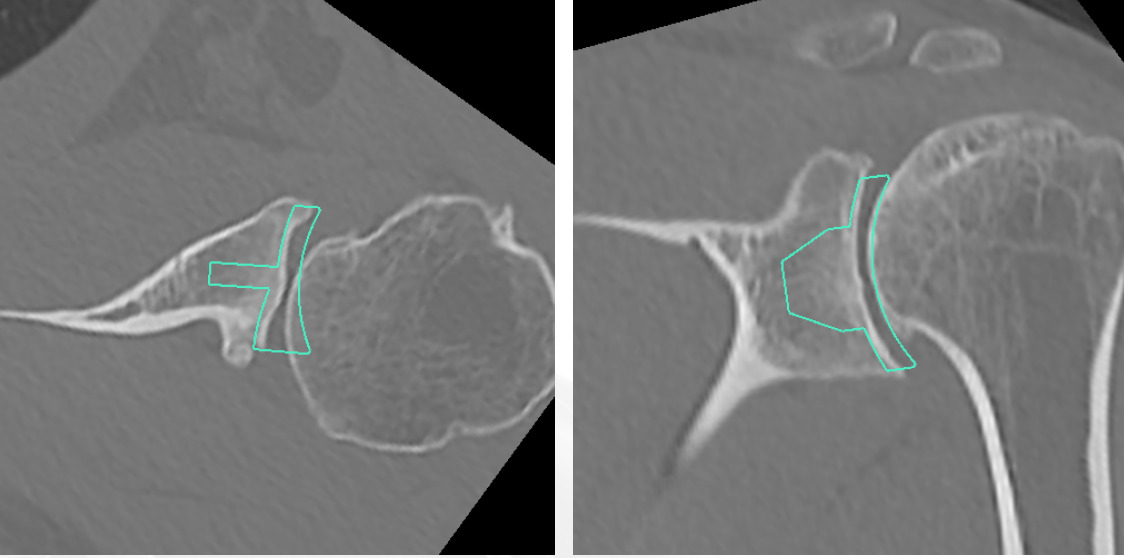
Glenoid version measurement
1. Xray v CT
- glenoid version axillary xray v CT
- glenoid retroversion overestimated on xray in 86%
- mean difference in measurements between xray and CT was 6.5o
2. Include scapula
Chalmers et al. J Should Elbow Surg 2017
- 14 B2 glenoids
- glenoid version measurement accurate if > 50% of the scapula width included
3. Measurement techniques
a. Friedman method
- tip of the medial border of the scapula to the midpoint of the glenoid fossa
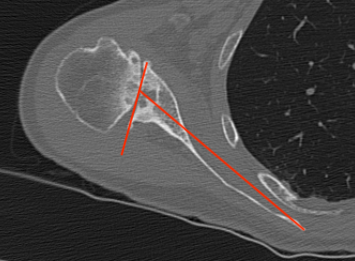
b. Scapula body method
- intersection of the scapula body axis and the glenoid surface
- 3o difference in measurement of glenoid version between the two
- excellent reliability for both measurement techniques
c. Glenoid vault method
- tip of scapula vault to centre of glenoid
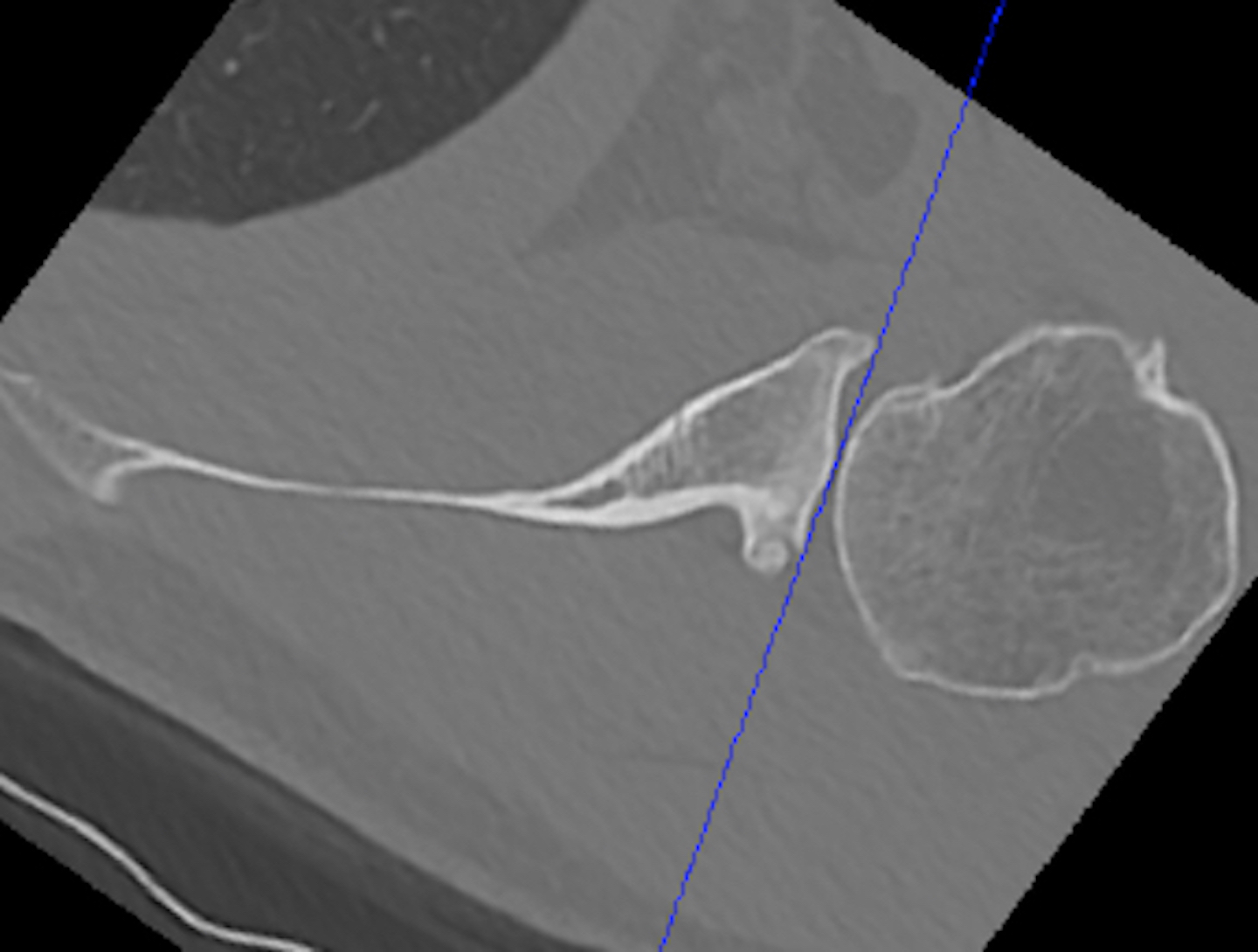
Automated 3D measurement of version
- automated software 3D measurement versus 2D Friedman method in 60 shoulders
- mean difference of 2o
- 3D software reliable and accurate

Anatomical Total Shoulder Design
Australian Joint Registry 2024
Revision rate
All diagnosis
| 5 year | 10 year | 14 year | |
|---|---|---|---|
| anatomic TSA stemmed n=7,800 | 8% | 13% | 17% |
| anatomic TSA stemless n= 4,600 | 4% | 5% | - |
| Reverse stemmed n=55,000 | 4% | 5% | - |
For diagnosis OA
| 5 year | 10 years | 14 years | |
|---|---|---|---|
| anatomic TSA stemmed n=7,400 | 8% | 13% | 18% |
| anatomic TSA stemless n=4,415 | 4% | 4% | |
| Reverse stemmed n=24,000 | 4% | 5% | 7% |
Reasons for revision anatomic TSA
Instability / dislocation 35%
Rotator cuff insufficiency 28%
Infection 15%
Loosening 12%
Pain 4%
Malposition 1%
Fracture 1%
Revision by age and gender
Higher revision rate with females (4.7% at 7 years) versus (4.1% at 7 years)
Higher revision rate with males < 55 (5% at 5 years) versus males > 65 (3% at 5 years)
Issues
Stems
Fixation
Glenoid component design
Glenoid position
Glenoid version
Constraint
Early highly constrained had high failure rates
Modern design
- high levels of glenohumeral mismatch and high levels of humeral head translation
- improved ROM and reduces rim stresses on glenoid
Stem
Stemmed versus short stems versus stemless


Australian Joint Registry 2024
- 12,000 aTSA for OA
- 10 year revision rate stemmed 13%
- 10 year revision rate stemless 14%
Willems et al EFORT Open Rev 2021
- systematic review and meta-analysis of 31 articles and 1944 stemless implants
- reduced intra-operative humeral fractures with stemless
Short stem


- systematic review of short stem TSA
- 13 studies with 823 shoulders at 33 month follow up
- 92% uncemented
- 2% humeral loosening, 1% revision for humeral loosening, 3% overall revision rate
Fixation

Werthal et al. Bone Joint J 2017
- 4636 shoulders (1167 cemented and 3469 uncemented)
- survival without loosening at 20 years 98% for cemented
- survival without loosening at 20 years 92% uncemented
Glenoid design
Cemented all poly versus uncemented metal back glenoid


Significantly higher revision rate will metal verus poly glenoids
- Australian Joint Registry
- 11,000 aTSA at 5 years follow up
- revision rate cemented glenoid 3.7%
- revision rate uncemented 17.9%
Peg v keel cemented all poly glenoid


Welsher et al. JSES All Access 2019
- meta-analysis of comparative studies
- higher rate of revision with keel v peg
- no difference in functional outcomes
Glenoid positioning
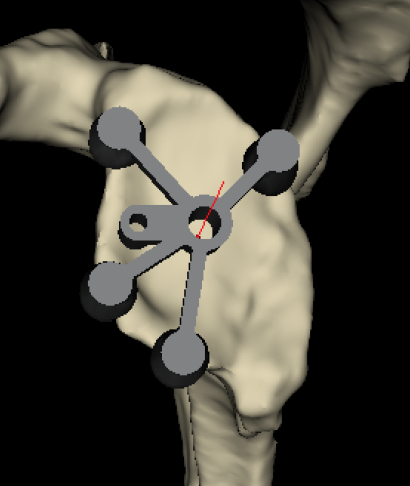
Standard PSI
Options
- standard instrumentation based upon identifying the glenoid centre point
- navigation
- PSI - patient specific instrumentation
Burns et al. Should Elbow 2019
- comparison standard v navigation v PSI
- both navigation and PSI improved glenoid positioning
- high rate glenoid malposition with standard instrumentation
Type B2 glenoids
Options
1. Eccentric reaming
2. Reduce humeral head retroversion
3. Bone grafting
4. Augmented glenoids
Eccentric reaming
Limit to 10o
- compromises anterior bone stock
- risk peg penetration through vault and glenoid fracture
- associated with glenoid loosening
- excessive glenoid reaming associated with radiological loosening of glenoid
Glenoid bone graft
Risks
- graft resorption / nonunion / migration / loss of fixation
- systematic review of glenoid bone grafting in aTSR
- 7 articles
- revision rate 5.4% at 6 years
Augmented glenoids
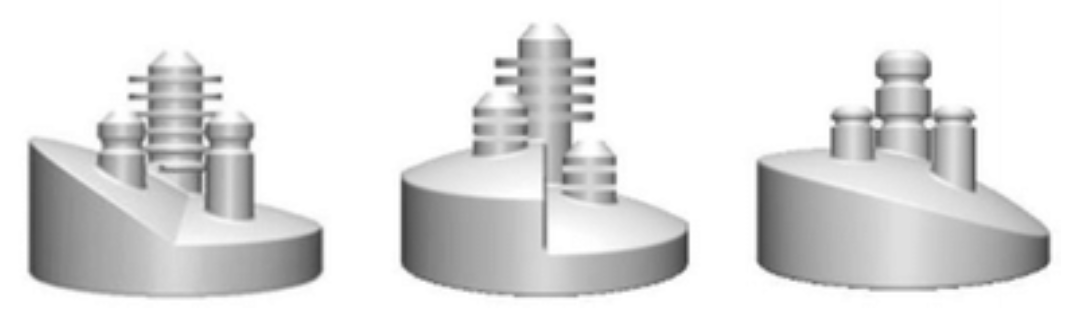
Posterior-wedged augment Stepped augment Full wedged augment
Advantages
- good version correction
- preserves bone stock
- CT evaluation of standard glenoid v posterior stepped augmented glenoid
- posterior stepped glenoid better at correcting version in type B2 and B3
- difficult to restore ML joint line position with both with central glenoid erosion i.e. type A2 or B3
Sheth et al. Should Elbow 2022
- systematic review of augmented glenoid components
- 9 studies and 312 patients
- good version correction
- increased radiolucency seen with 16 wedges and 5 mm steps
