Options
1. Always resurface
2. Never resurface
3. Selectively resurface
Decision Making
Controversial
- literature divided on issue
Historically
- poor outcomes due to poor implant design
- now improved designs
- non resurfacing also improved due to better design and improved techniques in regard to tracking and rotation
Advantages of resurfacing
Theory
- reduced anterior knee pain
- improved stair climbing
- reduced revision rate
Confounder
- patients with post operative pain and non resurfaced patellas
- are able to have a revision as a means of addressing their pain
- resurfaced patients are not
Disadvantage of resurfacing
Complication rate of ~10%
1. Implant failure
- early metal-backed high failure as thin poly & poor fixation poly to metal
- decreased incidence with all-poly components (1% of all revisions in AJR)
2. Fixation failure
- problem with overly aggressive bone resection & poor patellar preparation
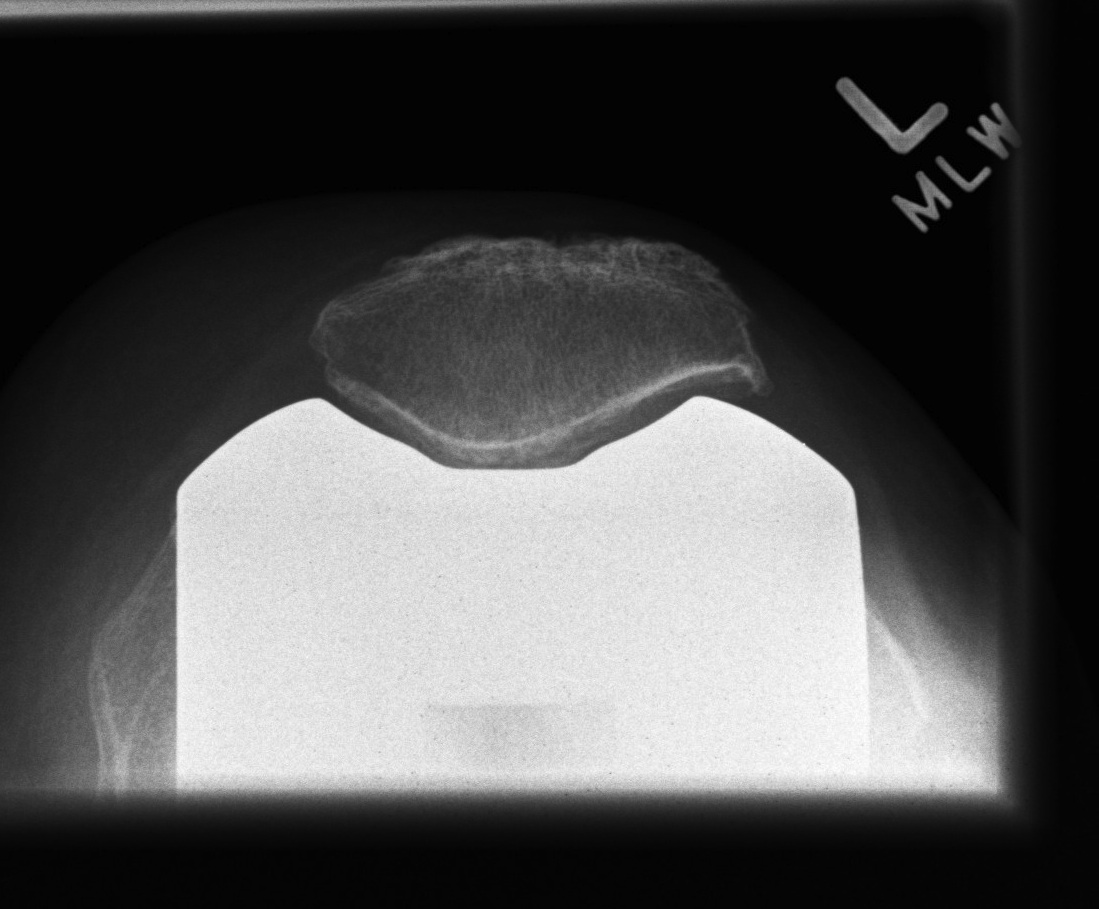
3. Patella fracture
- caused by excessive bone resection & holes in patella for fixation
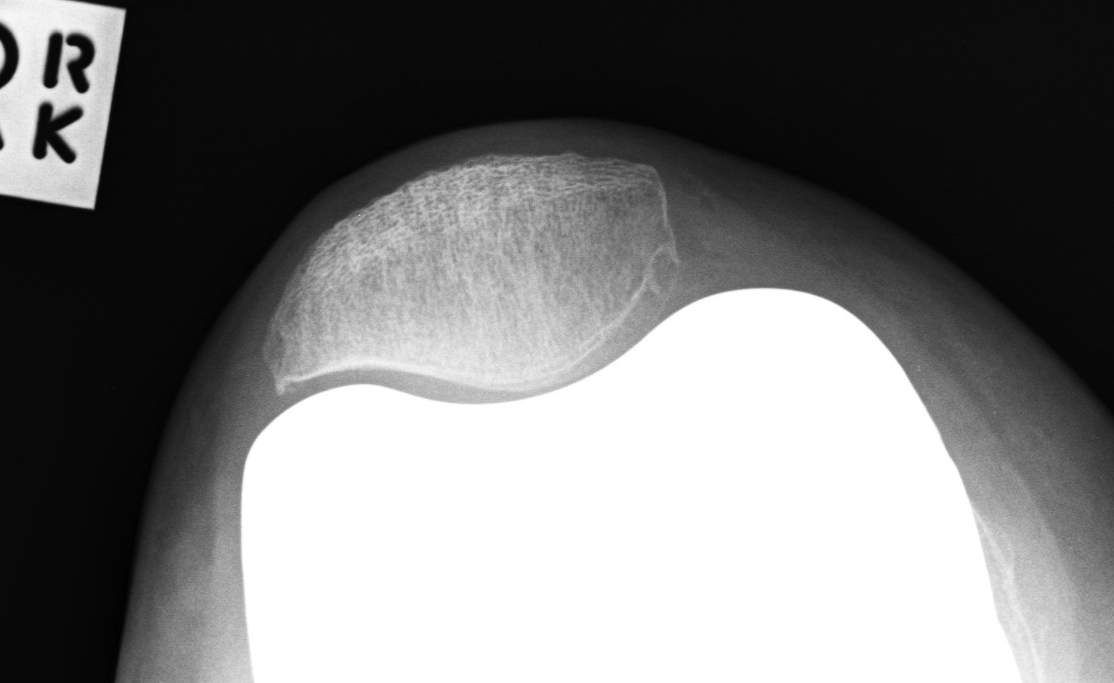
4. Dynamic instability
- instability 2° component malalignment & inadequate soft tissue balancing
- incidence of 4%
- mal-tracking / subluxation / dislocation
See TKR Complications / Patella
Resurfacing Indications
Absolute
- inflammatory arthritis
- mal-tracking
- PF OA as main indication for TKR
Relative
- severe OA (Gd 3/4) / pain PFJ
- elderly
- obesity
Non Resurfacing Indications
1. Young
- non inflammatory arthritis
- minimal OA changes
- normal tracking
- high risk of revision in future
2. Revision TKR with difficulty achieving fixation
3. Thin patella
- need at least 15mm post resection
Non Resurfacing Complications
PFJ Pain
Reported incidence of 10-25%
- poor stair climbing
- deterioration over time
- need for later resurfacing
Increased with
- inflammatory arthropathy
- poor tracking
- obvious OA
Selective Resurfacing
Resurface if
- Gd 4 PFJ OA
- abnormal tracking
- inflammatory arthritis
- old age
Patella Prosthetic Design
Metal Backing of Patella
- good fixation to bone
- but thin poly, getting wear and catastrophic failure
- poly can detach from metal
- out of favour
Anatomic patella
- no central plug
- femoral prosthesis deep conforming patellar groove & raised lateral flange
Central Dome
- most adaptive with least congruity
- button
- most common
Polyethylene
Cold Flow
- stresses measured exceed yield point of PE
- would predict much higher wear rates & loosening than observed clinically
- poly may experience "Cold Flow" which would change contact stresses over time
Soft tissue adaptation
- more likely explanation than change in shape of poly
- pseudo-meniscus of fibrous tissue often forms around the unloaded portion of patella component
- may transfer load to peripheral soft tissue
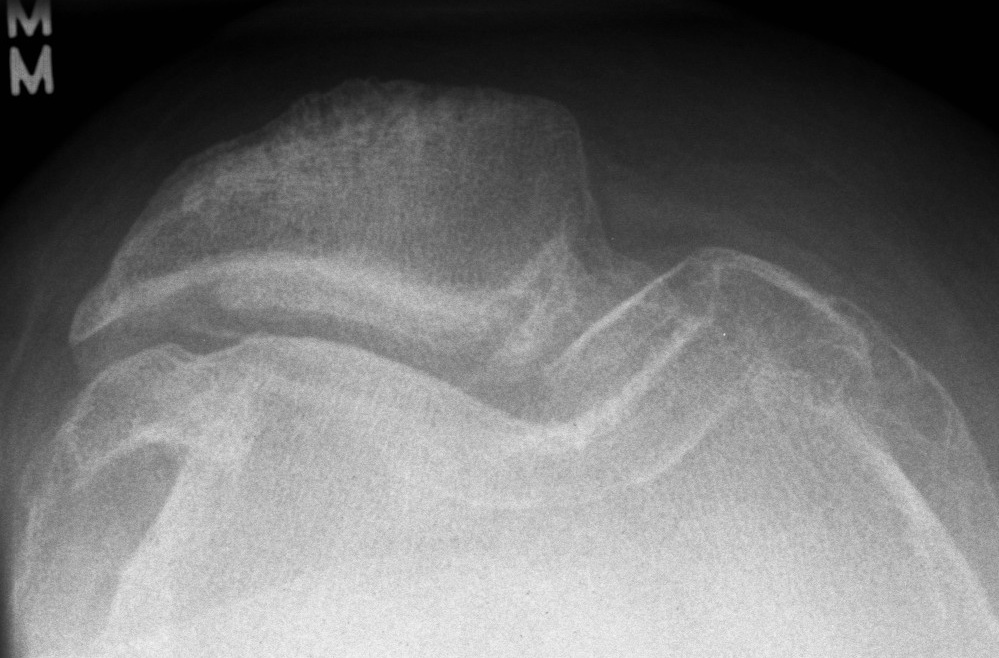
Femoral Design
Deeper trochlea groove
- provides patellar stability
Raising the lateral wall
- controls tracking
Increased congruency between patella and trochlea
Proximal extent of the anterior flange
- need adequate proximal extension
- minimises chance that the patella will ride off flange proximally in terminal extension
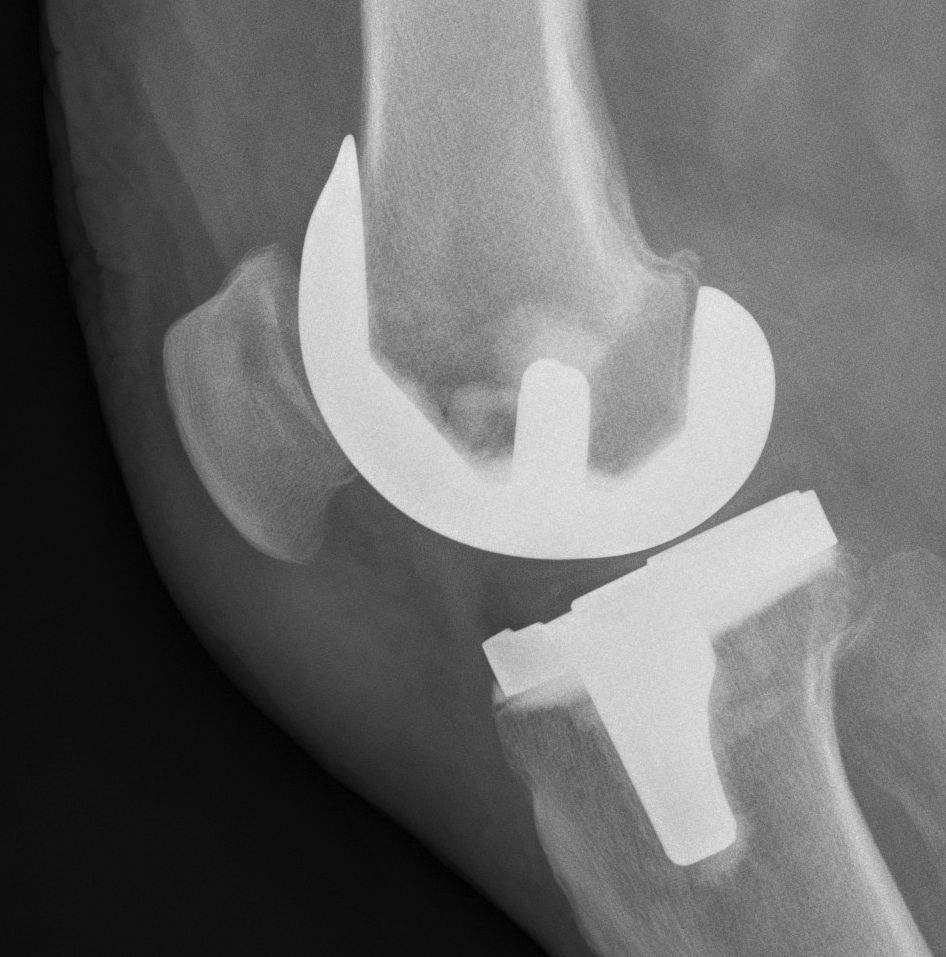
Inlay v Onlay
Onlay
- standard technique
- cut patella
- cement all poly patella
Inlay
- resect into the patella
- cement poly into patella
Surgical Technique
1. Appropriate component position
- femur 3o ER, lateral placement
- tibia slight ER, lateral placement
- restore mechanical axis
2. Restore thickness of patella
Under-resection
- overstuffs PFJ / anterior knee pain
- increases joint reaction force
- decreased flexion
Over-resection
- predispose to fracture
- ensure 15mm minimum
3. Avoid tilting patella
Symmetric bone resection
4. Ensure tracking well
Combination prosthetic positioning and soft tissue balancing
A. Patella button placement
- medialise component
B. Lateral Release
- assess tracking before retinacular closure
- perform lateral release if patella shows tilt or subluxation
- from "Inside Out"
- preserve LSGA if possible
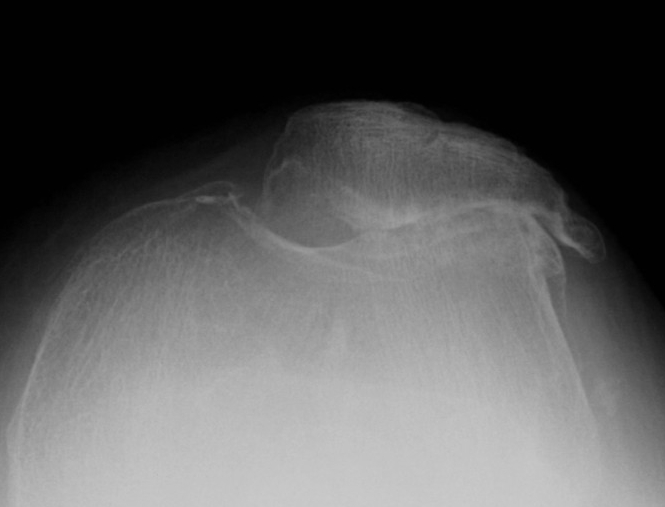
Patella Baja

Problem
- limits flexion
- due to patella impingement on tibia in flexion
Causes
- HTO
- tibial tuberosity transfer
- tibial fracture
Solutions
1. Lower joint line
- cut more tibia, distal femoral augments
2. Resurface patella and place button superiorly
- effectively lengthens the patella tendon
3. Shave anterior surface of PE
4. Trim but don't resurface patella
- resect
- shave off inferior aspect of patella
Results Resurfacing v Nonresurfacing
Burnett et al JBJS Am 2009
- ten year follow up of RCT in 118 knees
- no difference in ROM / function / global or anterior knee pain
- 7 patients (12%) had revision in non resurfacing related to PFJ
- 2 patients (3%) in resurfacing group relating to PFJ
Stirling et al JBJS Br 2006
- RCT of 100 knees with 10 year follow up
- 2 patients in non resurfacing had revision of PFJ
- 1 patient in resurfacing had a lateral release
- unable to recommend routine resurfacing
Waters et al JBJS Am 2003
- RCT of 500 knees followed up for 5 years
- AKP 25% in non resurfaced group
- AKP 5% in resurfaced group
Pakos et al JBJS Am 2005
- meta-analysis
- resurfacing had reduced reoperation rate of 4.6%
- would have to resurface 22 patella to prevent revising 1
- resurfacing had reduction of anterior knee pain of 13%
- have to resurface 7 patella to prevent AKP in 1
Australian Joint Registry 2010
9 year survival
- non resurfaced / CR 5.2%
- non resurfaced / PS 7.8%
- resurfaced / CR 4.3%
- resurfaced / PS 4.6%

