Non-operative Management
Natural history
Arthritis
Risk
- PFJ OA secondary to increased forces across this joint
- medial compartment OA as medial femoral condyle subluxes posteriorly
- retrospective database review of 4,000 patients with PCL tear
- increased risk of meniscal tear, osteoarthritis, and TKA
- 48 isolated PCL tears followed for mean 12 years
- 6 x risk of symptomatic osteoarthritis compared to matched patients
- 3 x risk of TKA
Shelbourne et al. Am J Sports Med 2013
- 44 patients with isolated PCL injury
- mean follow up 14 years
- moderate to severe medial OA in 11%
- no difference based upon degree of PCL laxity
Non operative protocol acute isolated injury
PCL brace concept
Dynamic anterior drawer brace
- holds tibia reduced / stops tibia subluxing posteriorly with flexion
- PCL can heal as is extra-synovial
- don't want it to heal in a stretched position
Results
- bracing of 21 patients with acute PCL injury
- decreased mean sag from 7mm to 3 mm at 2 years
Agolley et al. Bone Joint J 2017
- 46 patients with acute PCL and grade II / III instability
- all semi-professional or professional athletes
- 91% return to sport at same level 2 years post injury
- mean return 4 months
Shelbourne et al. Am J Sports Med 1999
- 133 patients with isolated PCL injuries followed for mean of 5 years
- 1/2 returned to sport at same level of play
- 1/3 returned to sport at lower level of play
Protocol
JACK PCL brace protocol (Agolley et al. BJJ 2017)
- 2 - 3 weeks: locked in full extension in brace, partial weight bear
- 2 - 6 weeks: full weight bear in brace, passive ROM in brace, closed chain quads strengthening, no hamstring
- 6 - 12 weeks: open chain quads
- 12 - 16: begin hamstring strengthening
- > 16 weeks: remove brace, begin running program


Ossur Rebound PCL brace Jack PCL brace
Operative Management
Indications
1. Combined ligamentous injuries
- only 1/4 PCL injuries is an isolated injury
2. Displaced bony avulsion fracture
3. Symptomatic grade III PCL injury
- pain and swelling
- development of PFJ pain / medial pain
- instability
- inability to return to sport
4. Acute grade III injury in athlete
- MRI evidence of tibial / femoral peel off
- consider acute repair
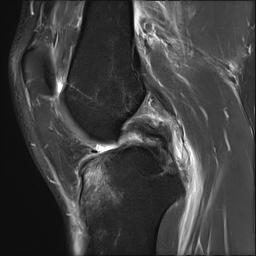
Acute femoral peel off of PCL
Acute Surgical Options
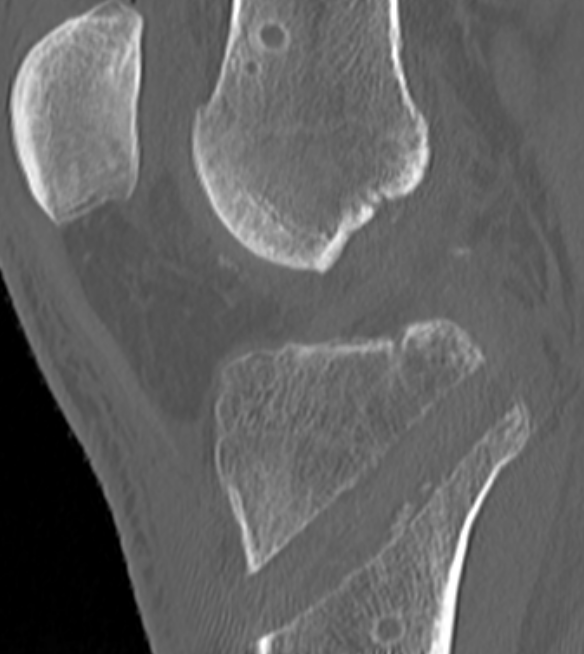
1. Repair bony avulsion
2. Acute suture repair of femoral peel off +/- augmentation
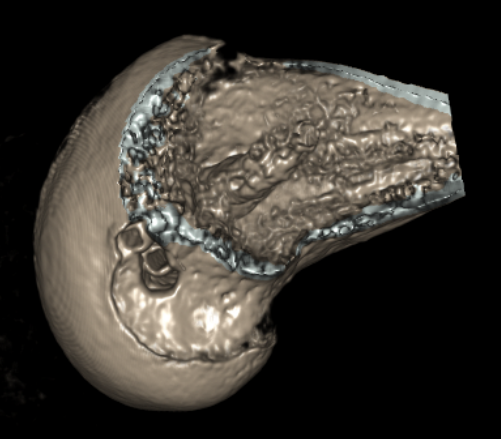
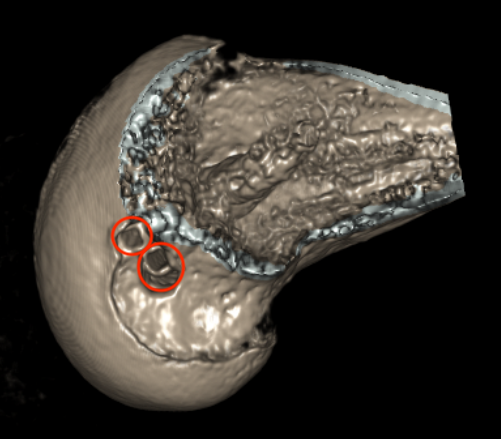
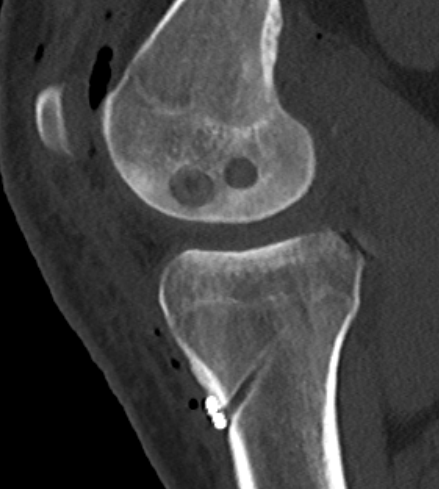
Repair Bony Avulsion
Options
Open posterior approach
- posterior approach
- Burks modified posterior approach
Arthroscopic
Results
Hooper et al. Am J Sports Med 2018
- systematic review of PCL tibial-sided bony avulsions comparing open and arthroscopic repairs
- 28 articles with 637 patients
- better functional outcomes with arthroscopic repair
- higher risk of stiffness in the arthroscopic group
Techniques
All arthroscopic bony avulsion surgical technique PDF
AO foundation open posterior approach
Vumedi video open fixation PCL bony avulsion
Acute repair of femoral peel off with suture tape augmentation
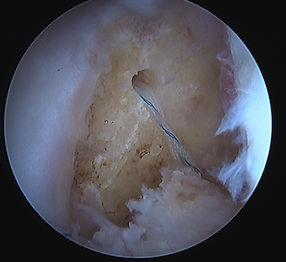
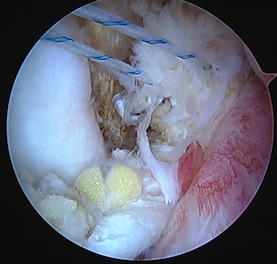
Indication
Femoral avulsion of the PCL
Acute injury
Technique
Repair to PCL to femoral insertion with sutures
Pass suture tape through tibial insertion to femoral insertion PCL to augment
Arthroscopic PCL repair surgical technique PDF
PCL Reconstruction
Issues
Outcomes of PCL Reconstruction
Kim et al. Am J Sports Med 2010
- systematic review of single bundle transtibial reconstruction
- review of 10 studies
- improves stability by 1 grade
- 75% patients resumed normal / near normal activity
- does not prevent OA
Devitt et al. Orthop J Sports Med 2018
- systematic review of 14 studies on isolated PCL reconstruction
- minimum 2 year follow up
- mean time injury to surgery 10 months
- 82% achieved IKDC A/B
- KT-1000 side to side difference mean 3.8 mm
- 44% return to sport
Failure rates
- Norwegian registry
- 185 isolated PCL reconstructions
- subjective failure rate at 2 years 50%
- subjective failure rate at 5 years 47%
- revision rate at 5 years 2%
Single v Double Bundle
Chahla et al. Arthroscopy 2017
- systematic review of single v double bundle PCL reconstructions
- 441 patients
- no difference in functional outcomes
- improved surgeon measured and Telos measured stability with double bundle
Transtibial PCL reconstruction v Tibial Inlay technique
- systematic review of 7 studies and 350 patients
- no difference in clinical outcome scores or recurrent laxity
- 25% of patients had significant residual laxity
Autograft v Allograft
Ansari et al. Arthroscopy 2019
- systematic review of 25 studies and 900 patients
- 600 autograft, 300 allograft
- no difference in functional outcome
- 2 comparative studies found reduced posterior laxity with autograft
- 2 comparative studies found no difference in posterior laxity between graft choices
Synthetic Ligaments
- systematic review of LARS for PCL reconstruction
- 7 studies for isolated PCL injuries with total 180 patients
- 3 retrospective cohort studies comparing LARS to hamstring autograft
- no difference in clinical outcomes or laxity
- synovitis rate 1%
- graft rupture rate 3%
Surgical techniques
Options
1. Trans-tibial
2. Tibial inlay
3. Double bundle
Trans-tibial Method
Technique
- tunnels in tibia and femur
- can be difficult to pass graft around back of tibia / killer turn
- concern that the killer turn of graft around the tibia can injure graft over time
Boneschool PCL reconstruction technique
Tibial Inlay Method
Technique
Open / arthroscopic placement of graft into tibial trough
- avoids 'killer turn' of graft in tunnel method
- soft tissue or bony graft into tibia



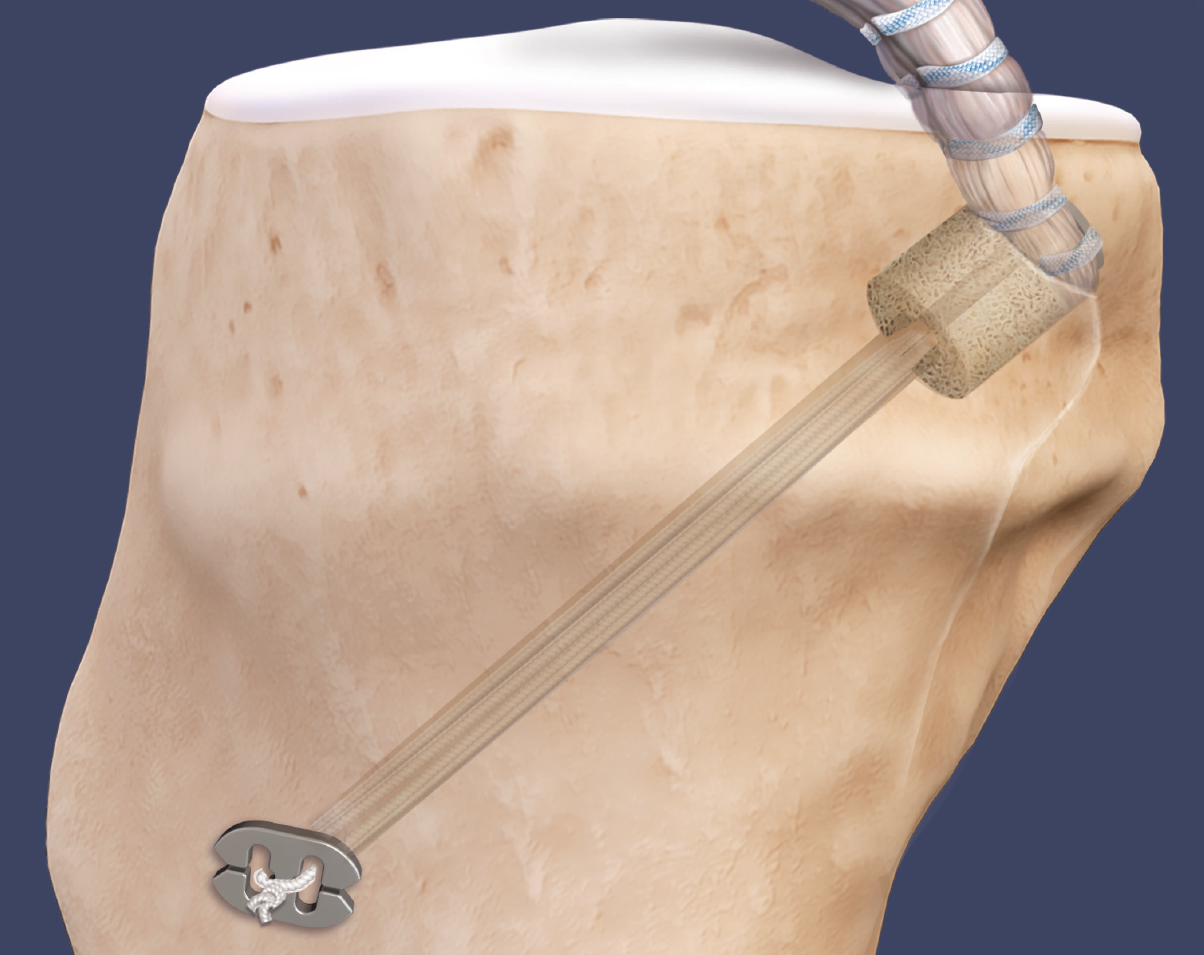
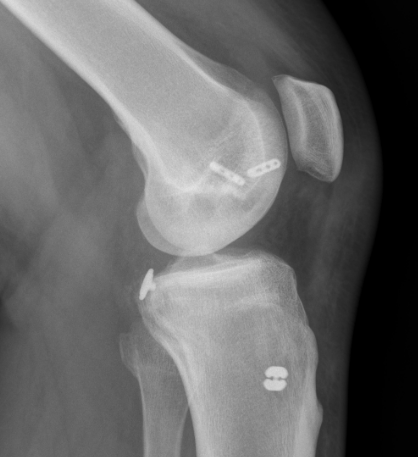

Arthrex tibial inlay technique using flip cutter to create bony socket arthroscopically
Open tibial inlay surgical technique PDF
Arthrex arthroscopic tibial inlay surgical technique PDF
Double bundle
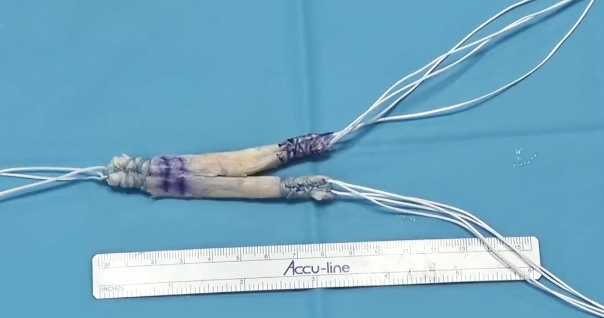

Technique
- single tibial tunnel
- 2 femoral tunnels
- use of a Y shaped graft
- divide tendon into two for the two femoral bundles
- AL bundle tensioned at 90o, PM bundle tensioned at 30o
Surgical technique double bundle PCL PDF
Arthrex double bundle PCL surgical technique
