Definition
Biological response to particulate matter
- characterised by periprosthetic osteolysis
- stimulated by wear debris
- debris gains access to any area accessible by fluid
Sources of particulate debris
1. Wear
Mechanisms of wear
A. Adhesion
B. Abrasion
C. Fatigue
Modes of wear
1. Motion between 2 surfaces designed for motion
2. Primary bearing surface against an non intended bearing surface
- i.e. femoral head against acetabular shell when liner has worn out
3. Interposed third body particles i.e. bone or cement
4. Two non bearing surfaces together i.e. back sided fretting, morse taper fretting, screws
2. Corrosion
Electrochemical process releasing metal ions
- modular interfaces i.e. head neck
- metal on metal bearings
Types of wear particles
Polyethylene
PMMA
Cobalt alloy
Titanium alloy
Morphology of wear particles
Usually less than 1um in size
Biological response to wear particles
Small particles phagocytosed by macrophages
- unable to digest
- stimulate release of cytotoxic factors
- TNF
- aggregates more macrophages
- release TNF, IL1, IL6, PGE2
- stimulated osteoclastic bone resorption
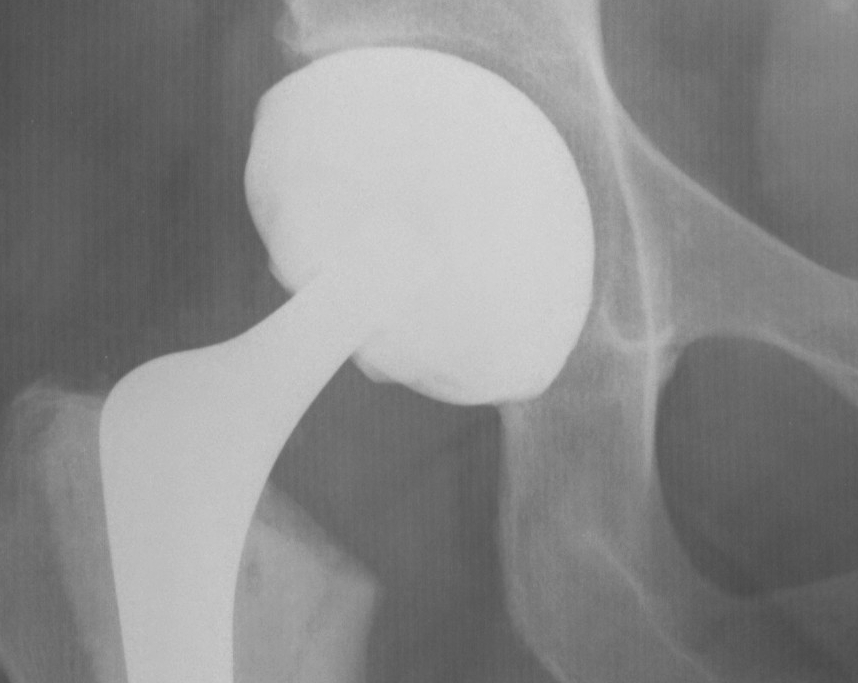
Poly wear

Lucent Zones
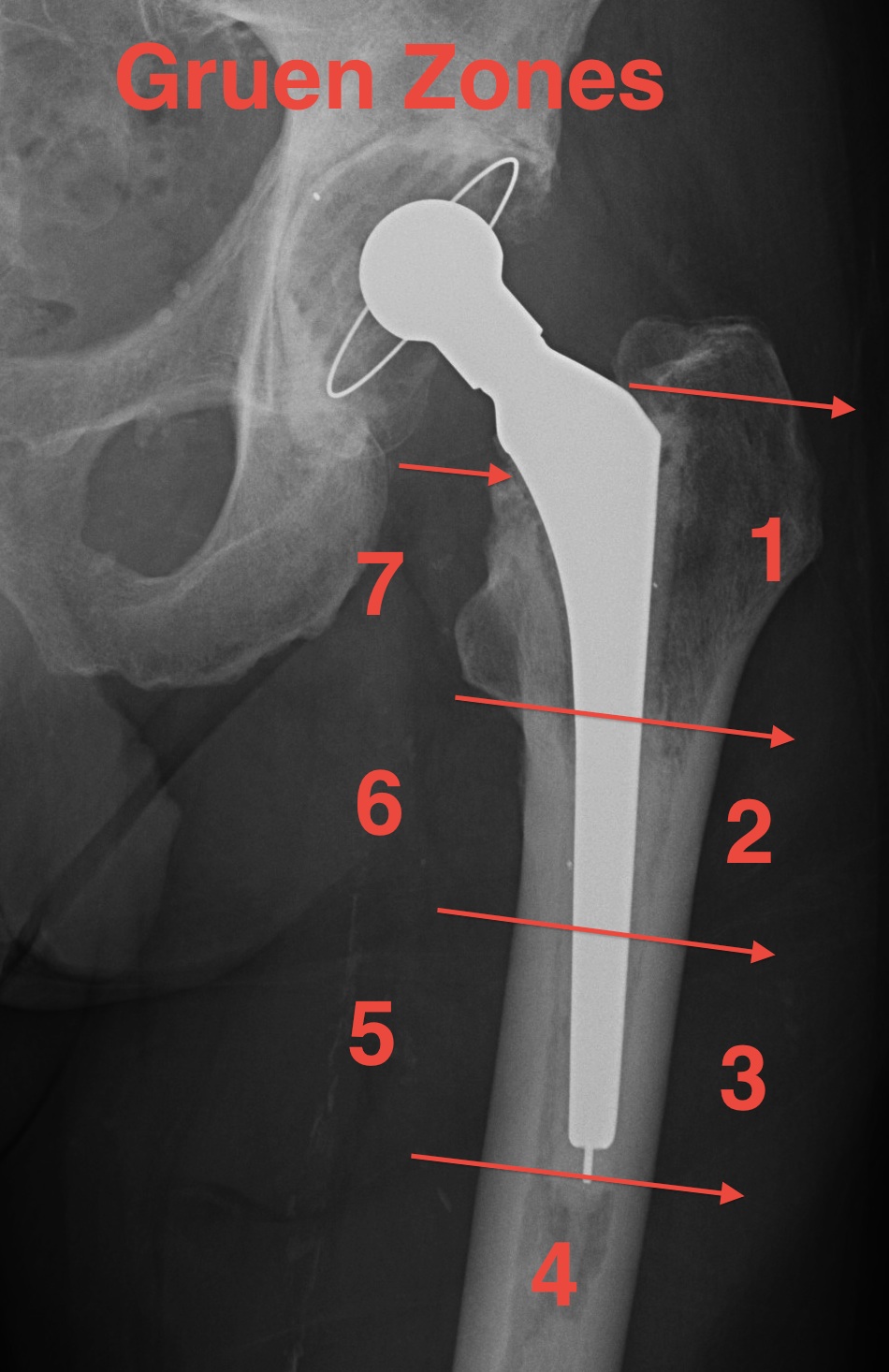
Femur: Gruen Zones
AP 1-7
Zone 1: Greater trochanter
Zone 4: Tip
Zone 7: Lesser trochanter
Lateral 8-14
Zone 8: Anterior-superior
Zone 11: Tip
Zone 14: Posterior-superior
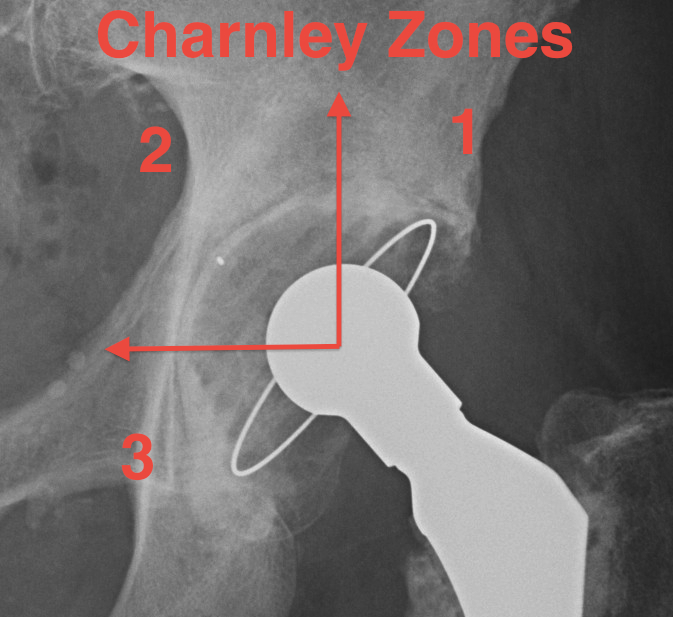
Acetabulum: Charnley Zones
Zone 1: Superior 1/3
Zone 2: Middle 1/3
Zone 3: Inferior 1/3
Loosening
Concepts
1. Easier to identify loosening in femur than acetabulum
- femur 90% accuracy
- acetabulum 65% accuracy
2. More difficult to identify in uncemented prosthesis
3. Lucent lines don't necessarily represent problem
- may be present in well-fixed prosthesis (retrieval studies)
- often due to remodelling
Cemented Femur
Signs of cemented femoral component loosening
O'Neil & Harris JBJS Am'84
1. Possible
Bone-cement lucency < 50% total
- may be due to poor cementing technique
- loosening if progressive
2. Probable
Cement-implant radiolucent line >2mm wide
- progressive

3. Definite
1. Cement fracture
2. Femoral stem fracture
3. New lucency cement - implant interface
4. Stem migration

A. Subsidence
- 1-2 mm normal in first year
- > 5 mm abnormal
- measure from tip GT to head neck junction
B. Medial midstem pivot
- pivots about midstem
- proximal medial, distal lateral
- poor cement superomedial or inferolateral
C. Calcar pivot / bending cantilever
- distal fix strong, but proximally loose
- breakdown of proximal cement
- bone destruction
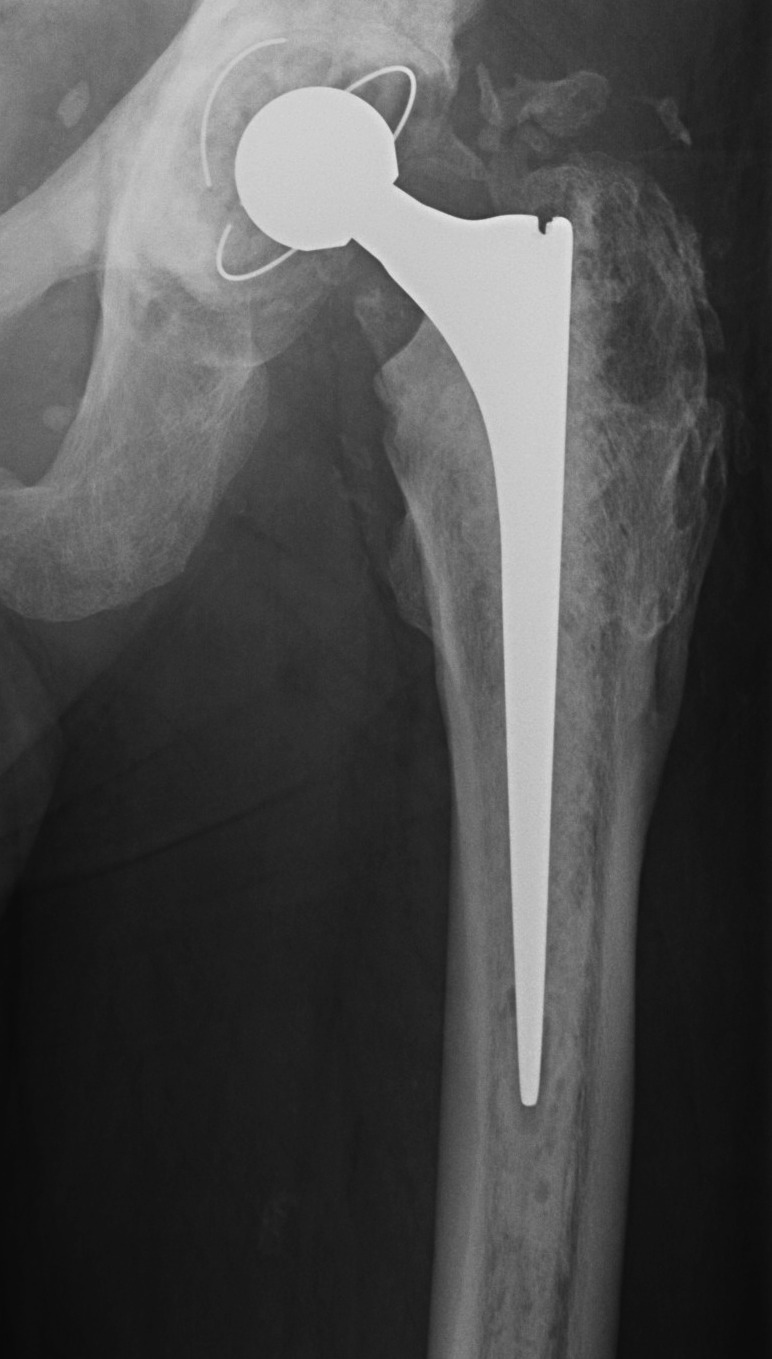
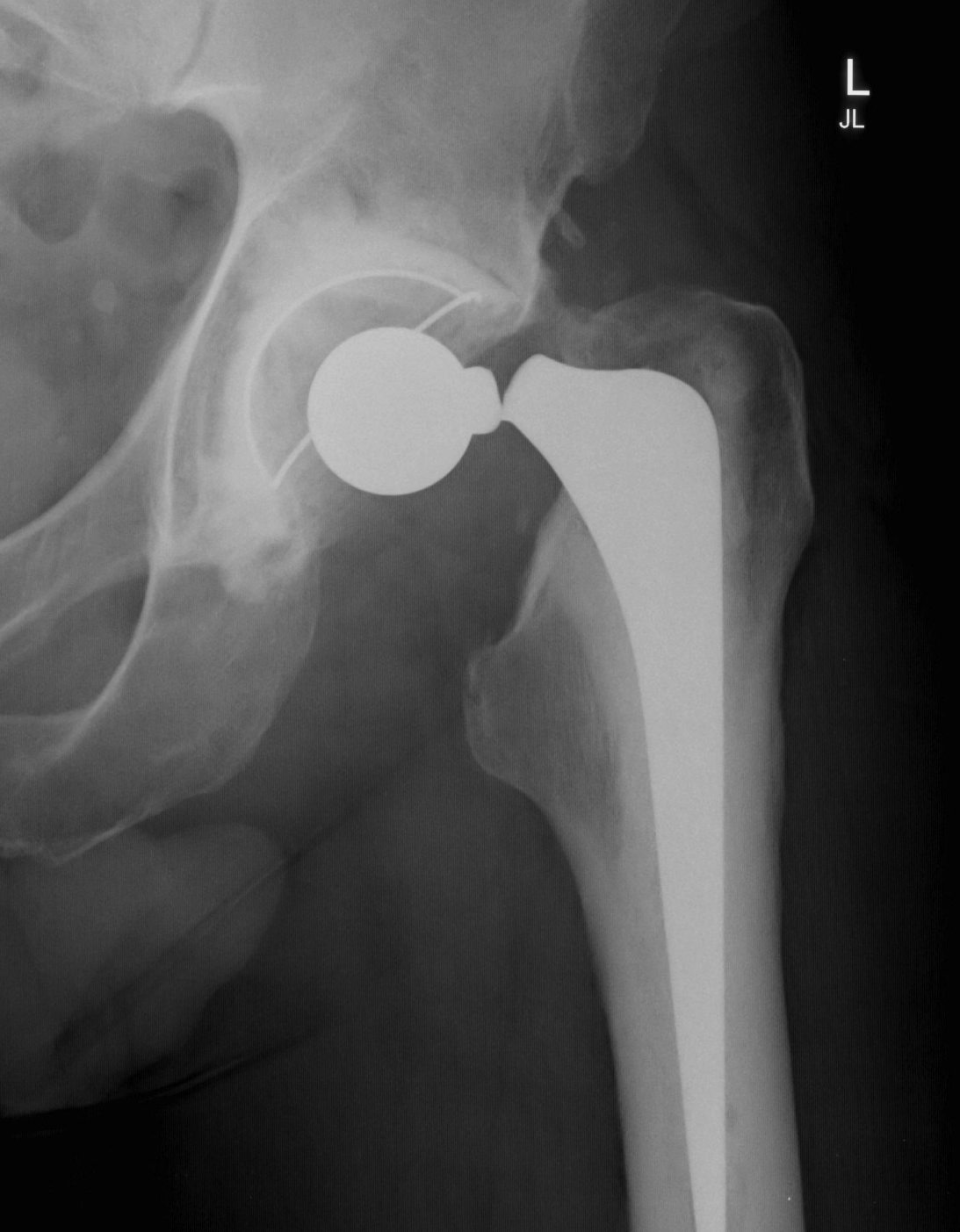
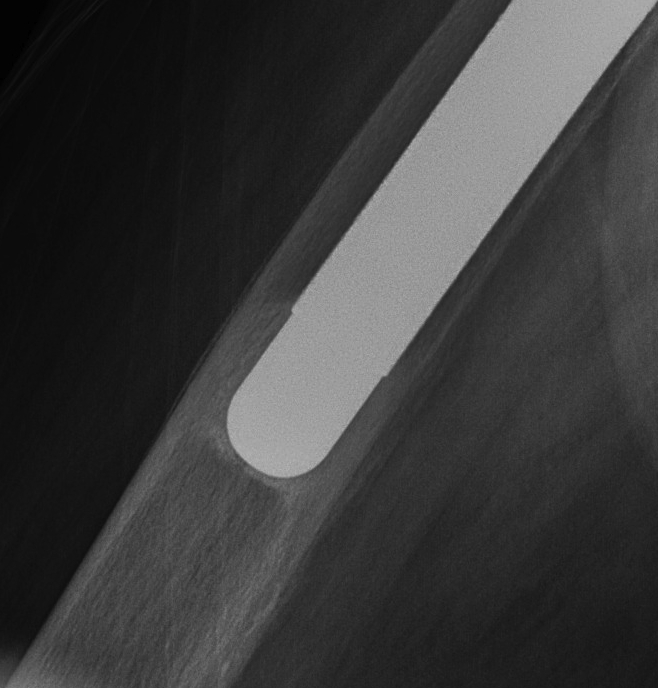
Uncemented femur
Engh classification
Types based on presence of radiolucent lines (RLL)
I. Stable bony ingrowth
Take one year to see
A. Spot welds at end of porous coating
B. Absence of RLL next to porous coating
- may have RLL next to non porous coated areas
C. Calcar atrophy secondary to stress shielding

II Stable fibrous ingrowth
A. No spot welds
B. Parallel sclerotic lines / RLL about porous coating
C. No migration

III Unstable fibrous ingrowth
A. Component migration
B. Progressive increase RLL
- divergent RLL
C. Pedestal formation (bony hypertrophy at tip)

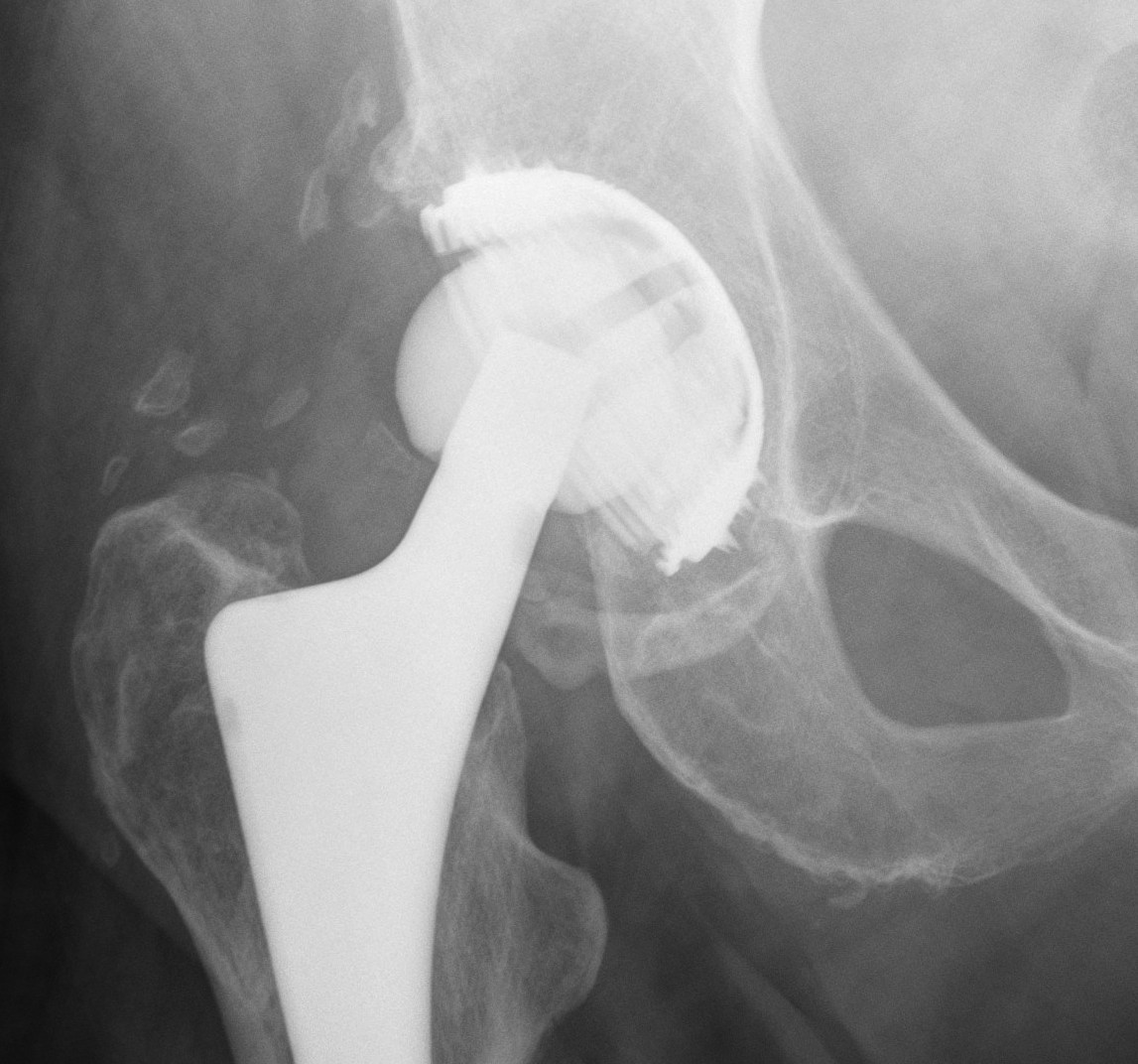
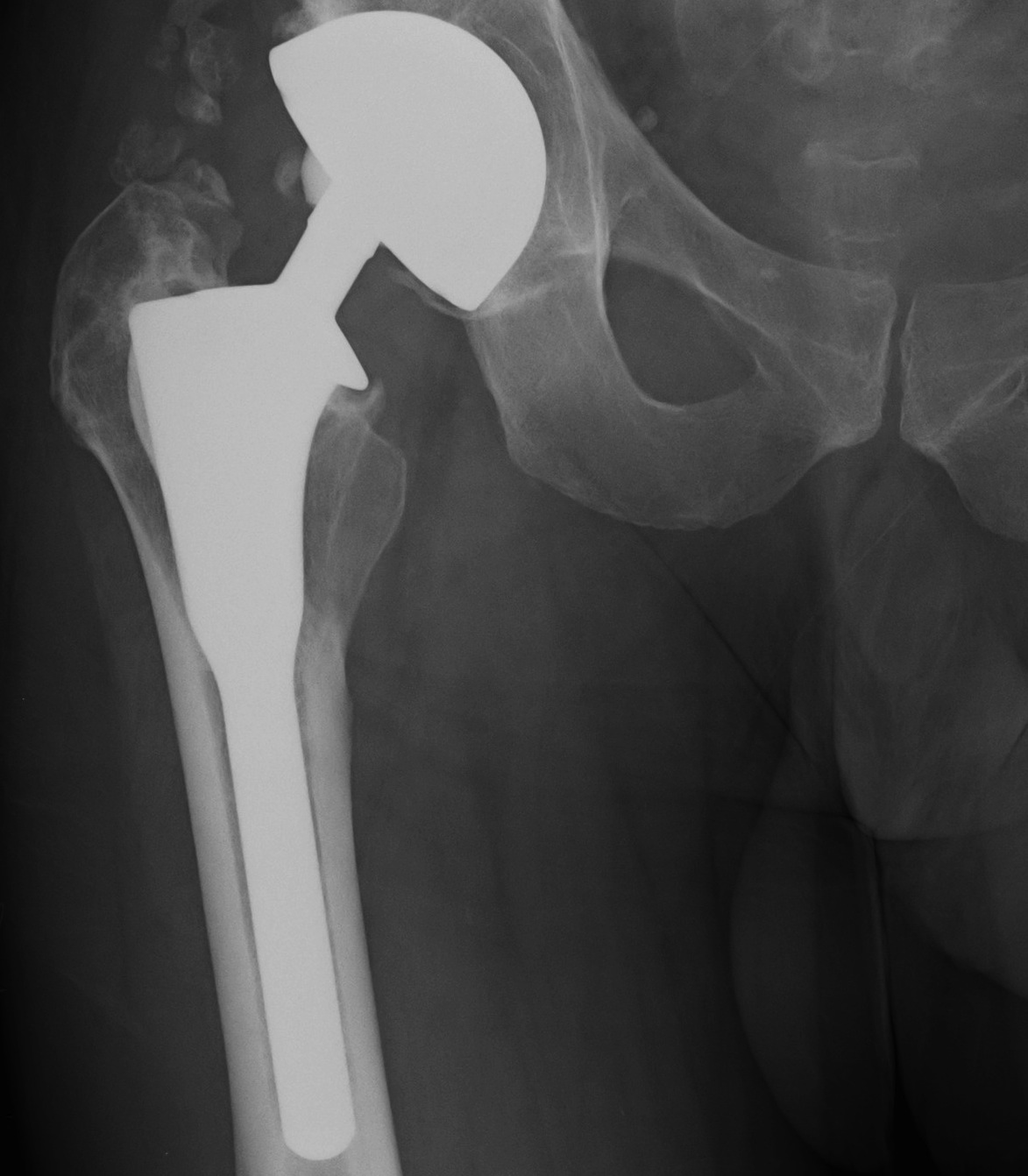
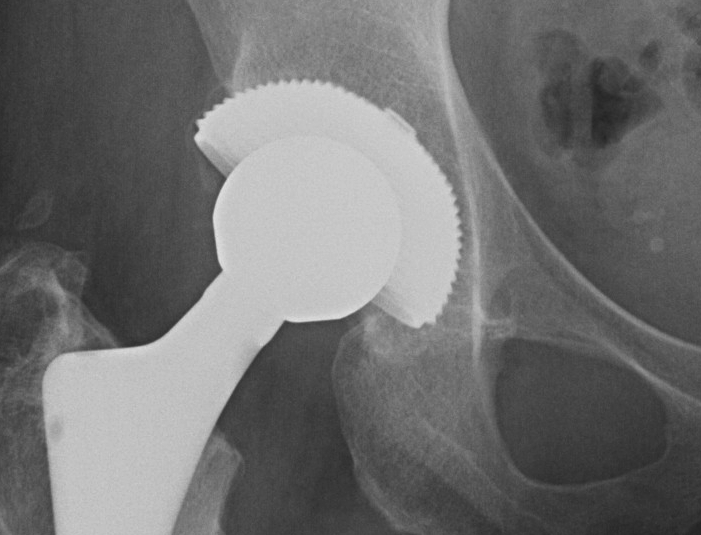
Uncemented Acetabular Component
Concepts
Bone ingrowth into component averages only 12%
- even with 84% bone contact
Non continuous radiolucent lines
- commonly found in press fit acetabular components
- are often not progressive
Radiographic signs of ingrowth fixation
Moore et al CORR 2006
- 3 or more 97% stable
- 2 or less, 83% unstable
Five signs
- absence of radiolucent lines
- presence of a superolateral buttress
- medial bone stress-shielding
- radial trabeculae
- inferomedial buttress

Radiographic signs of loosening
5 signs
- radiolucent lines that appear after two years
- progression of radiolucent lines after two years
- radiolucent lines in all three zones
- radiolucent lines 2 mm or wider in any zone
- migration > 2mm

Engh Classification
I Osse-ointegration
A No RLL
B One RLL zone 1 or 2
C RLL zones 1 & 2
II Stable fibrous ingrowth
- <2mm zone 3
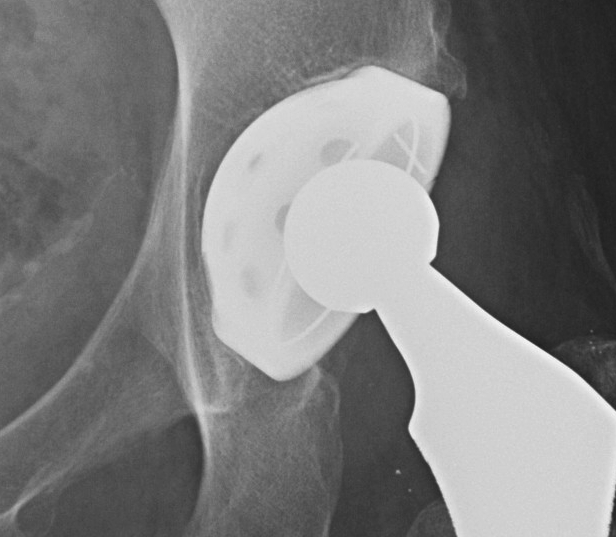
III Unstable fibrous ingrowth
- >2mm RLL in zone 3