

Johnson Classification
| Stage 1 | Stage 2 | Stage 3 | Stage 4 |
|---|---|---|---|
| T posterior tendonitis | T posterior rupture | Fixed deformity subtalar joint |
Varus angulation talus |
| Able to single heel raise |
Unable to single heel raise Correctable subtalar joint |
+/- subtalar OA | +/- ankle joint OA |
|
IIA: As above IIB: Forefoot abduction |
Management options
| Stage 1 | Stage 2 | Stage 3 | Stage 4 |
|---|---|---|---|
|
Orthotics
Tibialis posterior debridement +/- FDL transfer |
Medial displacement calcaneal osteotomy + FDL transfer
Lateral column lengthening
|
Triple arthrodesis |
Pantalar fusion |
Non operative management
Indications
Stage 1 Tendonitis
Stage 2 Flexible planovalgus
Options
UCBL
- worn inside the shoe
- ends under malleoli
- controls the heel (which must be flexible) & supports the arch
Operative management
Tibialis Posterior Synovectomy
Technique
Incision
- tip of medial malleolus to navicular
- open tendon sheath
- perform synovectomy +/- repair
+/- FDL transfer
FDL transfer
Technique
Incisions
- along entire length T posterior
- 10 cm proximal to medial malleolus
- to metatarsal cuneiform joint
Deep dissection
- abductor hallucis reflected plantarward
- Knot of Henry - crossover of FDL & FHL
- FDL plantar to FHL
- suture together and release proximal FDL
Expose navicular
- reinsert FDL into underside of navicular
- plantar to dorsal
- ankle in equinus & forefoot in varus
+/- repair spring ligament
Medial displacement calcaneal osteotomy

Technique
Lateral approach
- curve just behind peroneals
- homann in front of tendoachilles
- homann under calcaneum
Oblique osteotomy behind posterior facet
- 45o
- open with lamina spreader
- split periosteum medially with osteotome
- avoid damage to medial structures
- transfer medially 1 cm
- screw fixation

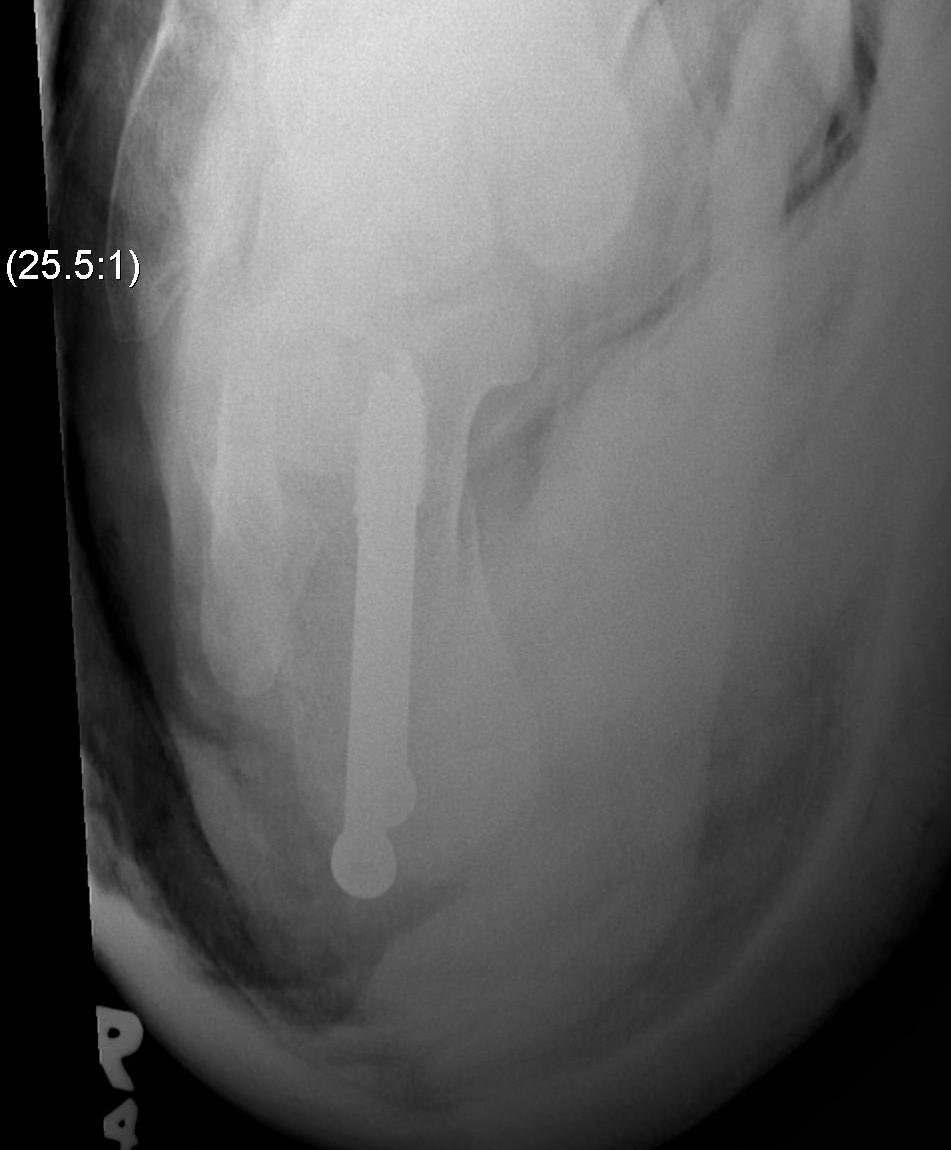
Evans Calcaneal Lengthening Osteotomy


Technique
Vumedi calcaneal lateral lengthening osteotomy video
Incision over anterolateral distal calcaneum
- sural nerve retracted plantar
- P longus retracted plantar
- identify CCJ
- Z lengthen P brevis
- homan retractor in sinus tarsi (between middle and anterior facets)
- homan retractor inferior calcaneum
- K wire into CCJ to prevent subluxation
Opening wedge osteotomy
- 1.5cm proximal to CCJ
- between middle and anterior facets medially
- begin with saw, complete with osteotome
- open 1 cm
- triangular / trapezoidal bone graft (allograft, iliac crest / mid fibular autograft)
- fixation with plate / staple / screw
+/- tendoachilles lengthening
+/- modified Kidner procedure (imbricate spring ligament, Tibialis posterior advancement)
Arthroereisis


Triple Arthrodesis
Indication
Fixed hindfoot deformity with lateral joint pain
Aim
Realign hindfoot with plantigrade foot
Issues
1. Fuse TNJ first
- this should passively align STJ
- need medial approach to reduce TNJ
2. Fuse STJ
- slight valgus not neutral or varus
- lateral approach
- may need large lateral bone wedge
- may have issues with lateral skin closure
