Definition
Symptoms & signs due to compression of median nerve in carpal tunnel
Epidemiology
Middle aged female
- F:M 2:1
- peak age 40-50 years
- often bilateral
Aetiology
Underlying process is decreased microvascular perfusion
- normal press in CT is 2.5mmHg
- most CTS > 30 mmHg & > 90 mmHg with palmar flexion
Commonest cause in tenosynovitis
Anatomical
1. Decreased size
- bony abnormality / thickened TCL
2. Increased contents
- hypertrophic synovium / fracture callus / hematoma
- neuroma / lipoma
- abnormal muscle bellies / persistent median artery
Physiological
1. Neuropathic Conditions
- diabetes / alcoholism / proximal lesion of median nerve (Double Crush)
2. Inflammatory Conditions
- tenosynovitis / RA / infection / gout
3. Altered fluid balance
- pregnancy / eclampsia / OCP
- thyroid problems / CRF / acromegaly / obesity
Patterns of Use
1. Repetitive flexion / extension
- manual labour / typing
2. Weight bearing with wrist extended
- paraplegia (weight bear on palms) / long-distance cycling
3. Vibration
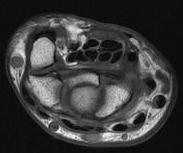
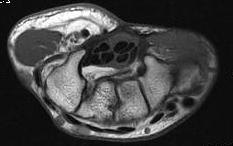
Anatomy
Transverse carpal ligament / TCL
- tuberosities of scaphoid and trapezium laterally
- pisiform and hook of hamate medially
- distal volar wrist crease proximal limit
- Kaplan's line (apex of interdigital fold between thumb and IF) distal limit
Carpal tunnel
- FCR in separate tunnel with FPL separate and below
- median nerve radial to 4 FDS
- IF / LF below MF / RF
- 4 FDP at base
- FPL separate
Motor Branch of Median nerve
Most important structure at risk / location can vary
1. Extraligamentous Recurrent / 50%
- branches distal to TCL with recurrent course to thenar muscles
2. Subligamentous / 30%
- branches beneath TCL / lies close to median nerve
- recurrent course to thenar muscles distal to TCL
3. Transligamentous/ 20%
- branches beneath TCL and pierces TCL to enter thenar muscles
4. Other
- proximal division
- branch from ulnar border of median nerve
- nerve superficial to TCL
Palmar Cutaneous Branch of Median Nerve
- arises in distal 1/3 of forearm from palmar-radial side of median nerve
- usually 5 cm proximal to wrist
- Pierces deep fascia between FCR & PL
History
Often diverse
Classic
- pain & numbness radial 3± digits
- nocturnal wakening with relief from shaking
- worse with driving
Examination
Look
- thenar wasting
Feel
- abnormal thenar sensation suggests higher compression
- decreased sensation lateral 3 1/2 digits
Move
- APB weakness
Augmented Phalen's
- elbow extended & supinated
- wrist held flexed 60° 2 fingers for 30 seconds
- sensitive 80% / specific 99%
Tinel's
- percussion of the median nerve at wrist
- paresthesia in distribution of median nerve indicate a positive test
- sensitive 75% / specific 95%
DDx
EJ compression
- more proximal pain / AIN weakness
T1 lesion
- check interossei power
C6/7 lesion
- similar sensory loss
- check wrist extension / triceps
NCS
SNAP
Stimulate proximally
- measure in IF and MF (sensory only from median)
- measure latency / conduction velocity / amplitude
Conduction velocity
- compare to ulna nerve
- usually > 50 m/s
- median nerve slightly slower
- should be within 0.2 / 0.3 m/s
- can compare to tables or to contralateral median nerve (may be bilateral pathology)
Latency
- > 3.5 ms = Abnormal
- > 1 ms between sides
Results
90% sensitive
10% false negative rate
- intact conduction in a small number of fibres will give normal conduction velocity for whole nerve
- normal study does not rule out CTS
EMG
Denervation activity (late change)
- spontaneous depolarisation
- fibrillations
Re-innervation
- large polyphasic AP
X-ray
Exclude wrist arthritis / tumour
Management
Non-operative management
Options
Splint
Wrist in neutral / Night splints
NSAID
HCLA
Risk
- must avoid intraneural injection
- can cause chronic pain and disability
Pregnancy
Incidence
- 2%
- most recover 6/52 after delivery
- very rarely require decompression
Management
- splints
- HCLA
Operative Management
Indications
Failure non operative management
Permanent numbness / weakness
- indicates nerve damage which may not resolve
Options
Open carpal tunnel release
Endoscopic carpal tunnel release
Neurolysis
Open Carpal Tunnel Release
Effect
1. Increase volume carpal tunnel by 25%
2. Increases Guyon's canal
- may relieve compression ulna nerve / LF numbness
- Guyon's canal goes from triangular to circular
Technique
LA infiltration over site of release
- incision in line with radial side ring finger
- parallel to and ulna side of thenar crease
- if cross wrist, ulna side of PL to avoid palmar branch of median nerve
- divide palmar aponeurosis which has longitudinal fibres
- divide TCL which has transverse fibres
- ensure released proximally and distally
- inspect for ganglion etc
Endoscopic CTR
Issues
- transection of recurrent branch median nerve
- especially with abnormal anatomy and inexperienced surgeons
Technique
GA, Tourniquet
Proximal transverse incision at wrist crease
- insert spatula
- under TCL, feel it, clear soft tissue
- insert cannula
- exits in palm through distal incision
- wrist DF over bump with strap
Insert camera looking up at TCL
- must see transverse fibres in full for entire length
- clean with Q tip, or with probe if needed
- ensure nerve branches not crossing plane
- cut with hook knife under vision
Results
Trumble et al JBJS Am 2002
- RCT of 192 patients open v endoscopic
- better grip strength in first 3 months
- less scar tenderness and earlier return to work
- no complications from endoscopic technique
Complications
Incorrect diagnosis
Incomplete decompression
Division of palmar branch
Palm dysaesthesia with is difficult to salvage
- sensitivity often precludes use of hand
- avoid by always staying ulnar to thenar crease
Diagnosis
- confirmed by LA block
Management
- explore and bury nerve ending
Hypersensitive Scar
- much more common if cross wrist crease
"Pillar Pain"
- 4% at 10 months post surgery
RSD
- decreased with minimal nerve trauma & avoiding neurolysis
Division of recurrent branch
Management
- operative repair
Tenderness / sensitivity of median nerve
Cause
- due to superficial course post op
Management
- if a real problem needs soft tissue to cover
- proximally can use pronator quadratus
- distally use hypothenar fat graft on vascular pedicle
Flexor tendon bowstringing or adhesions
- Bowstring tendons 2% of open CTR
Persistant numbness
- may take 12 months for all symptoms to resolve
- loss of Schwann cells resulting in persistent conduction block
Recurrence
History
- symptom free interval
- usually due to scar
