Epidemiology
>65
Third most common fracture after hip and distal radius
Anatomy
Neck shaft angle 130o
Head retroverted 20o relative to shaft
Anatomical neck (junction of head and metaphysis)
Surgical neck (junction of diaphysis and metaphysis)
Blood supply
Gerber JBJS Am 1990 December
Anatomical cadaver study
1. Anterior humeral circumflex
Major supply
- gives anterolateral branch
- runs in intertubercular groove lateral to biceps
- becomes arcuate artery
- supplies GT / LT / entire epiphysis
Nearly always disrupted in fractures
2. Posterior Humeral circumflex
Small contribution posterior head
- allows head to survive with both tuberosities fractured
3. Rotator cuff
Supplies blood to tuberosities in fractures
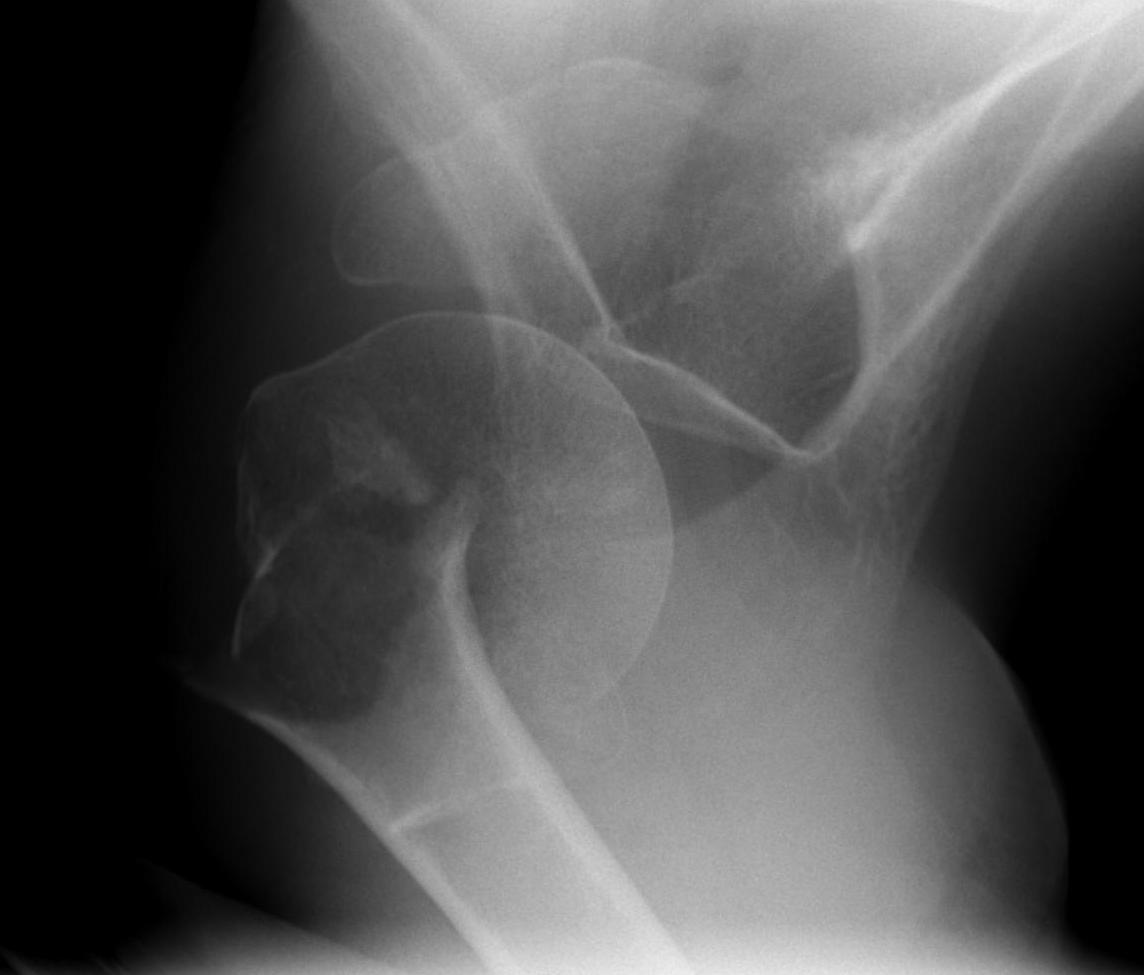
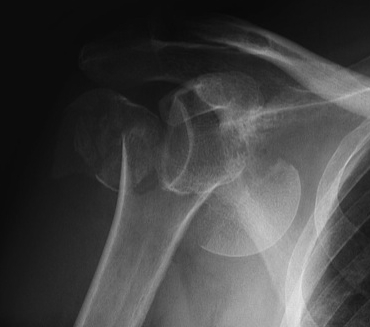
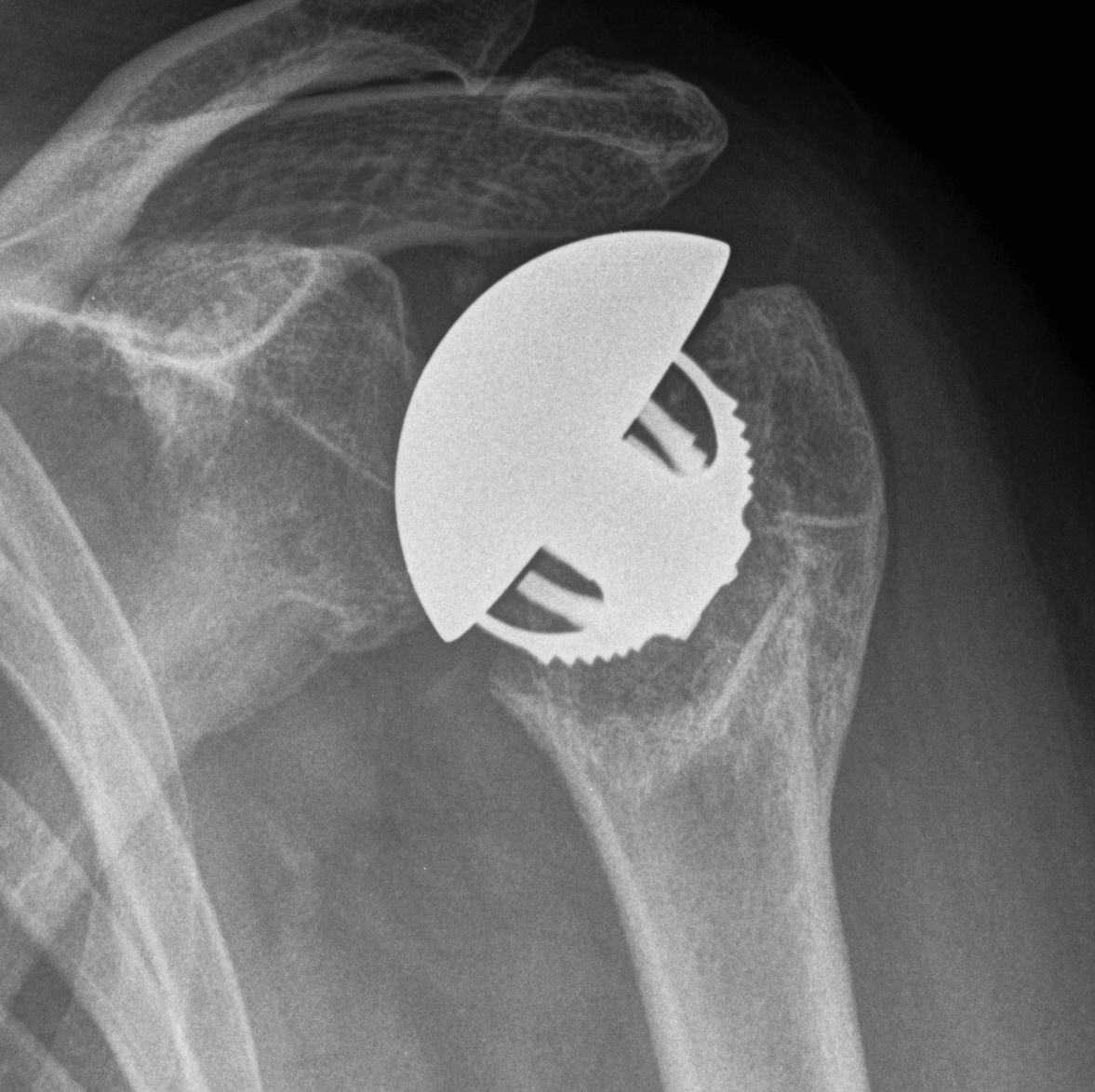
Neer Classification 1970
Displaced
Any fragment
- > 1cm displaced
- > 45o angulated
Number of displaced fragments
- 2 part (head/shaft, GT, LT)
- 3 part (head/shaft/GT, head/shaft/LT)
- 4 part (head/shaft/GT/LT)
Fracture / dislocation
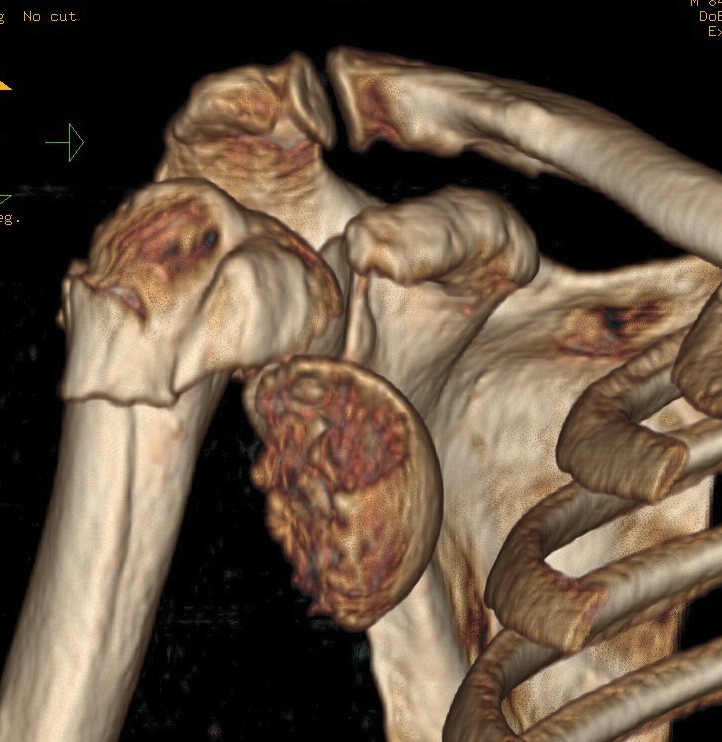


Head splitting fracture


Anatomical Neck Fracture
Avascular necrosis

Risk AVN
In most fractures, arcuate artery is disrupted, but head survives
- posterior circumflex artery is sufficient
- risk increases with amount of displacement
4 part fracture 30%
3 part fracture 15%
Hertel Radiographic criteria
Hertel et al J Should Elbow Surg 2004
https://pubmed.ncbi.nlm.nih.gov/15220884/
2 criteria to predict ischaemia
A. Metaphyseal head extension < 8 mm
B. Medial hinge displaced > 2mm
97% positive predictive of ischaemia if both factors present
Aetiology
FOOSH - mostly elderly patients with osteoporotic
Young patients - high energy MVA
Deforming Forces
2 part fracture
- pectoralis major displaces shaft medially
- head internally rotated by SSC

Greater tuberosity fracture
- fragment pulled postero-superior
- combination of SS / IS / T minor


Lesser tuberosity fracture
- displaced medially by subscapularis

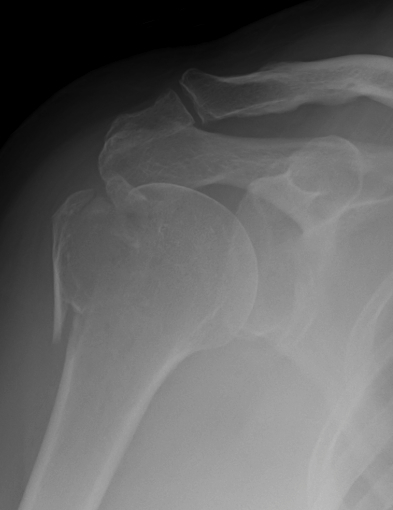
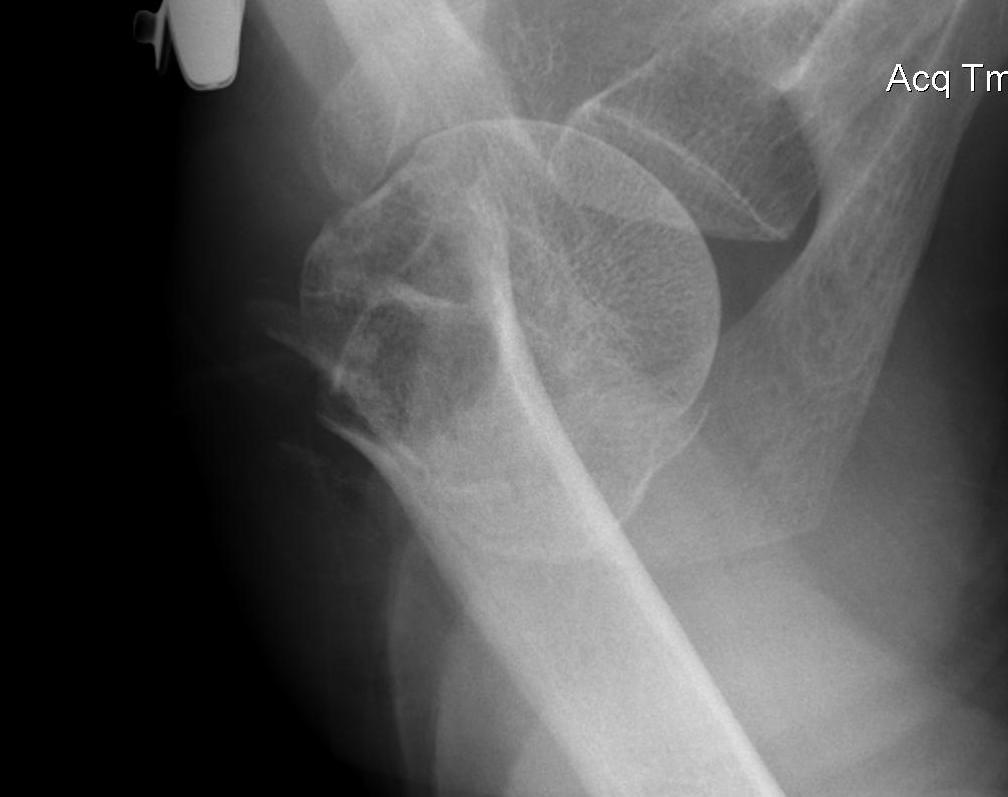
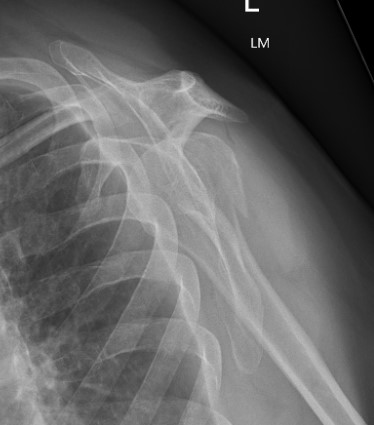
X-rays
AP / Scapula Lateral / Axillary lateral
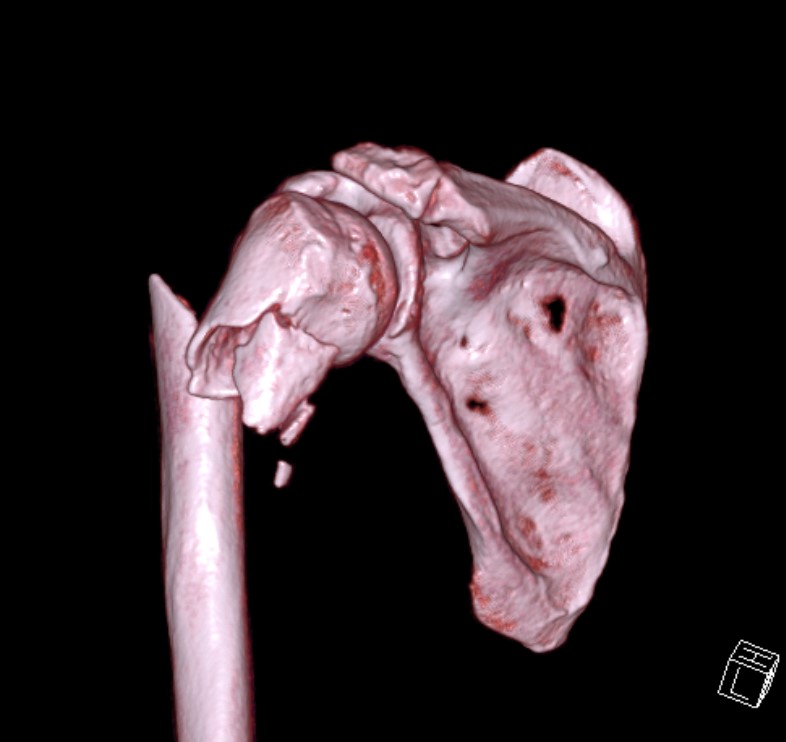
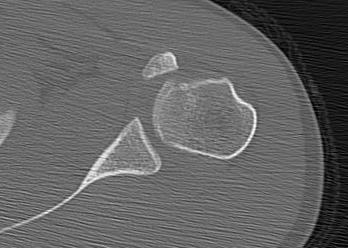
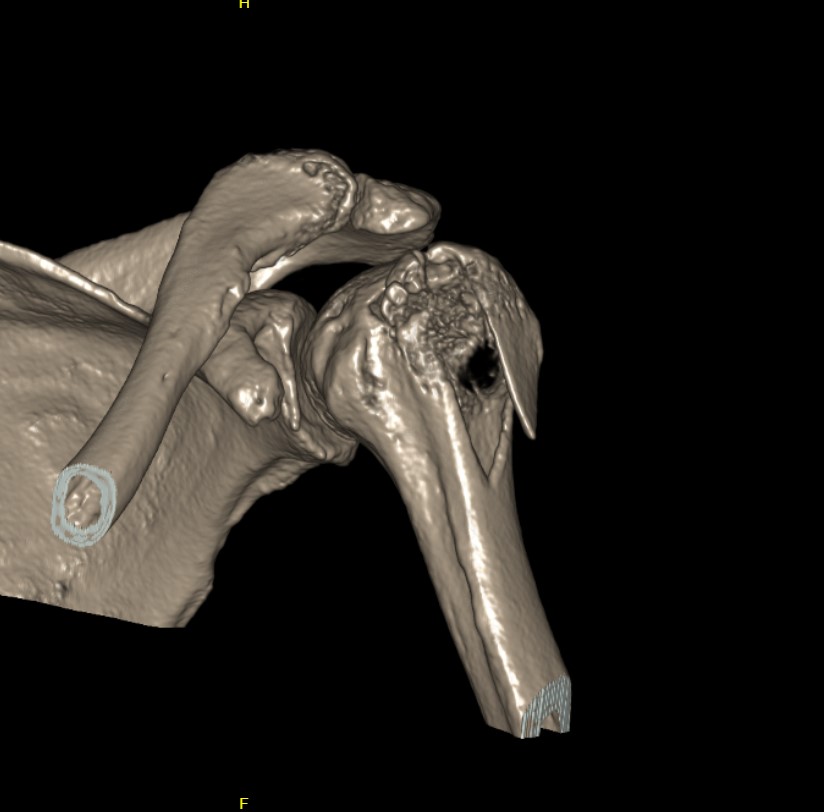
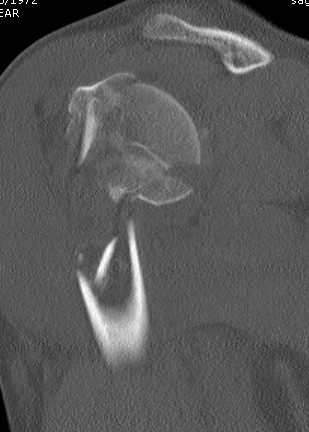
CT
Assess
- number of fracture fragements
- degree of displacement
- head splitting fracture
- is there sufficient bone in humeral head to consider ORIF?



Associated Injuries
Axillary nerve
- most commonly injured as close proximity
- relatively fixed by posterior cord brachial plexus & deltoid
Axillary artery
- in young patient with high speed injury
- can have collateral circulation and pink hand
Management
Non operative
Indications
Minimally displaced
Elderly / low functioning patients
Results
Koval et al JBJS Am 1997
- 104 patients minimally displaced fracture as per Neer
- < 1cm displacement and <45o
- 90% no pain, 77% good or excellent result
- ROM approximately 90% of the other side
- 10% moderate pain and 10% poor result
- poor function and ROM associated with phyio started > 14 days after injury
- poor function associated with pre-existing cuff problems
Olerudet al JSES 2011
- RCT nonop v hemiarthroplasty for displaced 4 part
- 55 patients, average age 77
- 2 year follow up
- significant advantage of hemiarthroplasty
Complications of nonoperative treatment
Non-union
Uncommon
- associated with AVN
Malunion OA


TSR / consider resurfacing if significant deformity
- can be difficult surgery due to abnormal anatomy
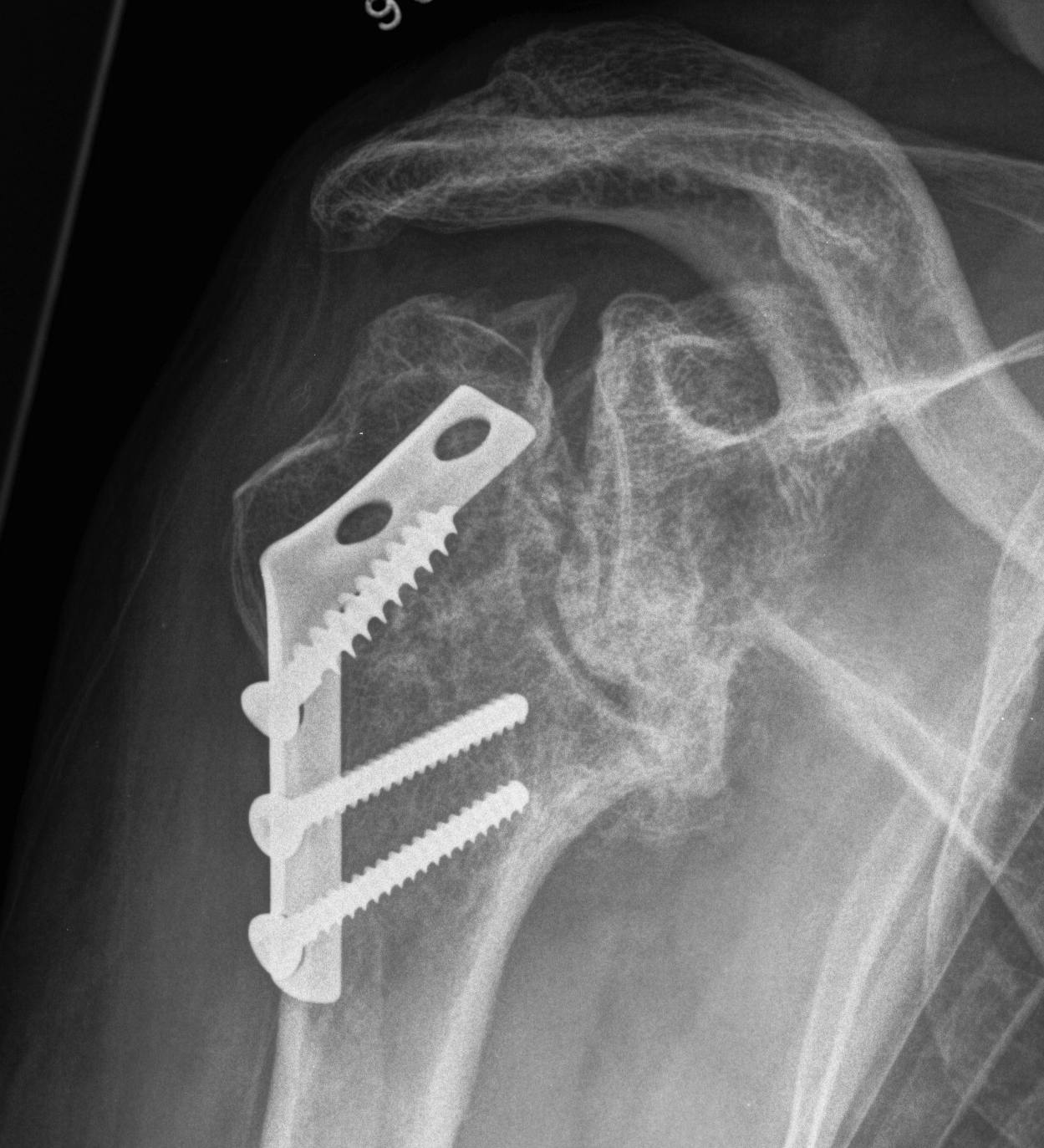
Operative Management
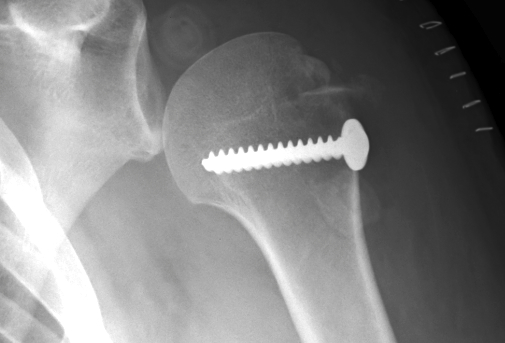
1. Two Part Fractures
A. Surgical neck of humerus
Indications
- >1 cm displaced or > 45o angulation


ORIF with proximal humerus plate
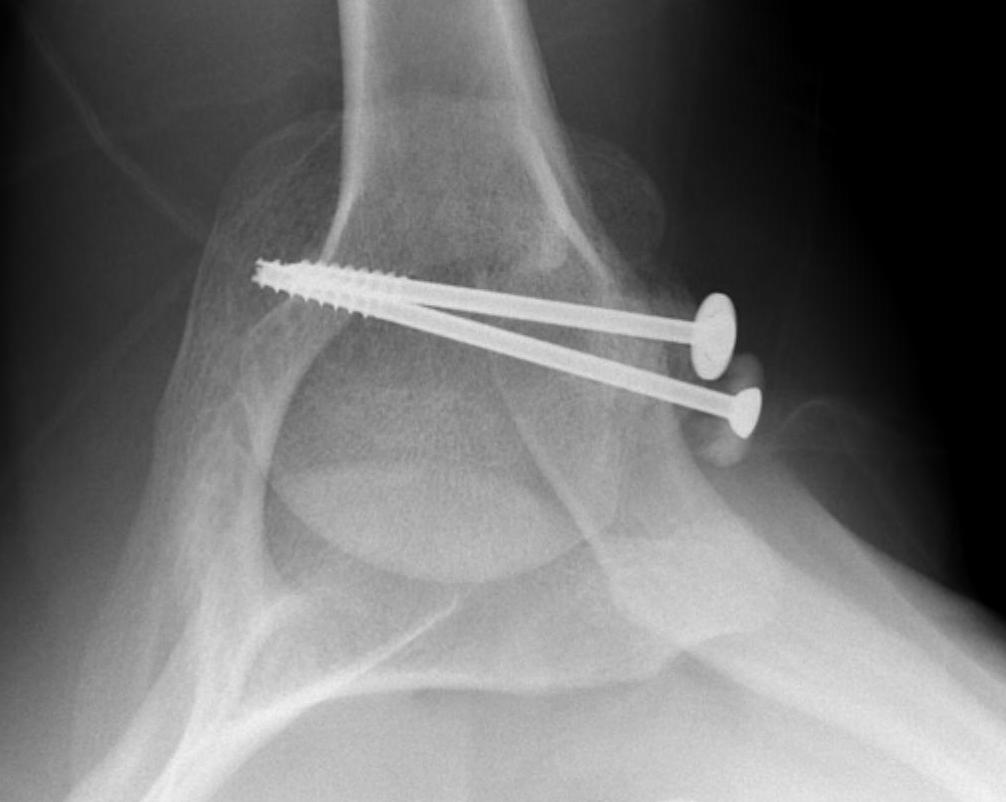
B. Displaced fractures of the greater tuberosity
Issues
- > 5 mm displaced needs ORIF
- superior displacement will cause impingement
- up to 25% associated with cuff tear
- repair of cuff important step




Options
Suture and repair over distal screw
Lateral plate
Technique
Deltoid splitting approach
- young patient can ORIF with screw
- in elderly insert Mason Allen no 2 suture in cuff and tie over screw
- repair rotator cuff
C. Lesser tuberosity fractures
Soft tissue washer and screw


2. Three and Four part fractures
Options
ORIF
IM nail
Hemiarthroplasty
Reverse TSR
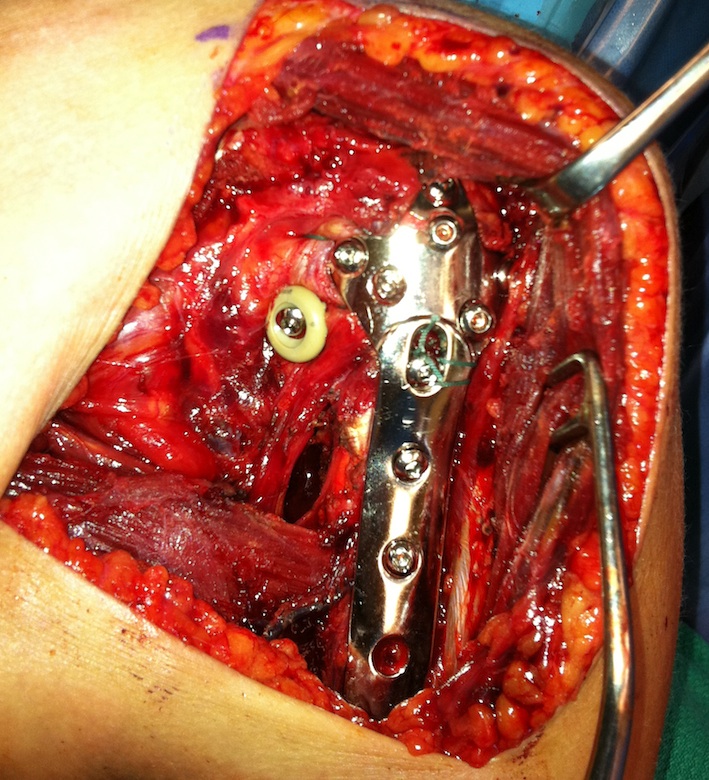
ORIF with plate

Indications
Young patient
Sufficient bone quality
Results
Surgical technique

Set up
- GA, IV antibiotics, lazy beach chair
- mark anatomy
- ensure adequate flouroscopy images
Deltopectoral approach
- cephalic usually taken laterally
- Hawkins Bell retractor/ blunt gelpies
- divide clavipectoral fascia to expose SSC
- release lateral edge of conjoint tendon
- place retractors deep to tendon
- release adhesions from undersurface of deltoid
Extensile approach
- release CA ligament
- release proximal pectoralis major
- can release anterior deltoid insertion from clavicle if needed (intra-osseous repair latera)
Dangers
- protect musculocutaneous nerve under conjoint, minimal retraction
- protect the axillary nerve on inferior border of SSC medially
Identify structures
- identify and release biceps tendon
- identify and tag greater and lessor tuberosities with Mason Allen sutures
- remove hematoma
- reduce head onto shaft (head is displaced posteriorly)
- use elevator and lever it forward
- provisionally fix with 2 mm k wire
- check provisonal fixation with fluoroscopy
Apply plate
- lateral to biceps with single cortical screw in oblique hole
- check fluoroscopy aain to avoid having plate too high
- keep head out of varus to avoid cutout
- long inferomedial screws / kickstand screws

Complications ORIF
Cutout
- medial support very important
- must avoid varus malreduction
Plate impingement
- need to ensure place plate low on the head
Screw perforation of humeral head
- most common complication
AVN
- fortunately uncommon


Vascular Injury
Axillary / MCN / Brachial Plexus
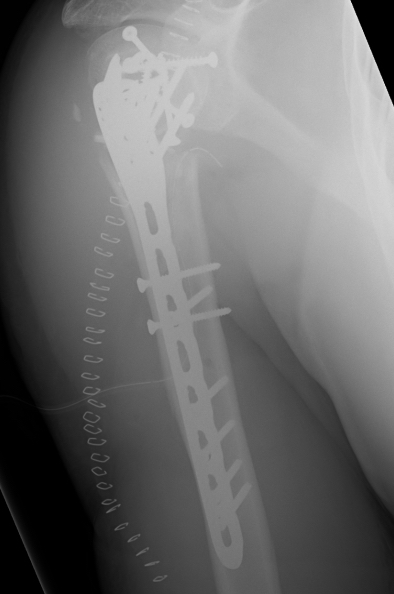
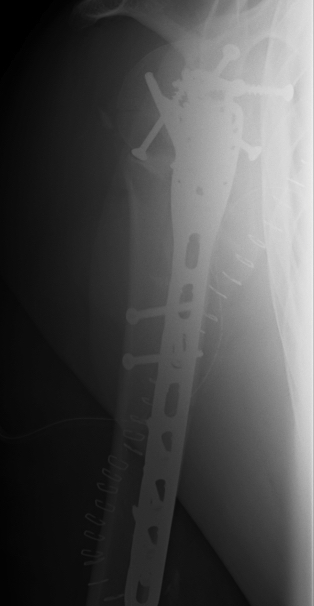
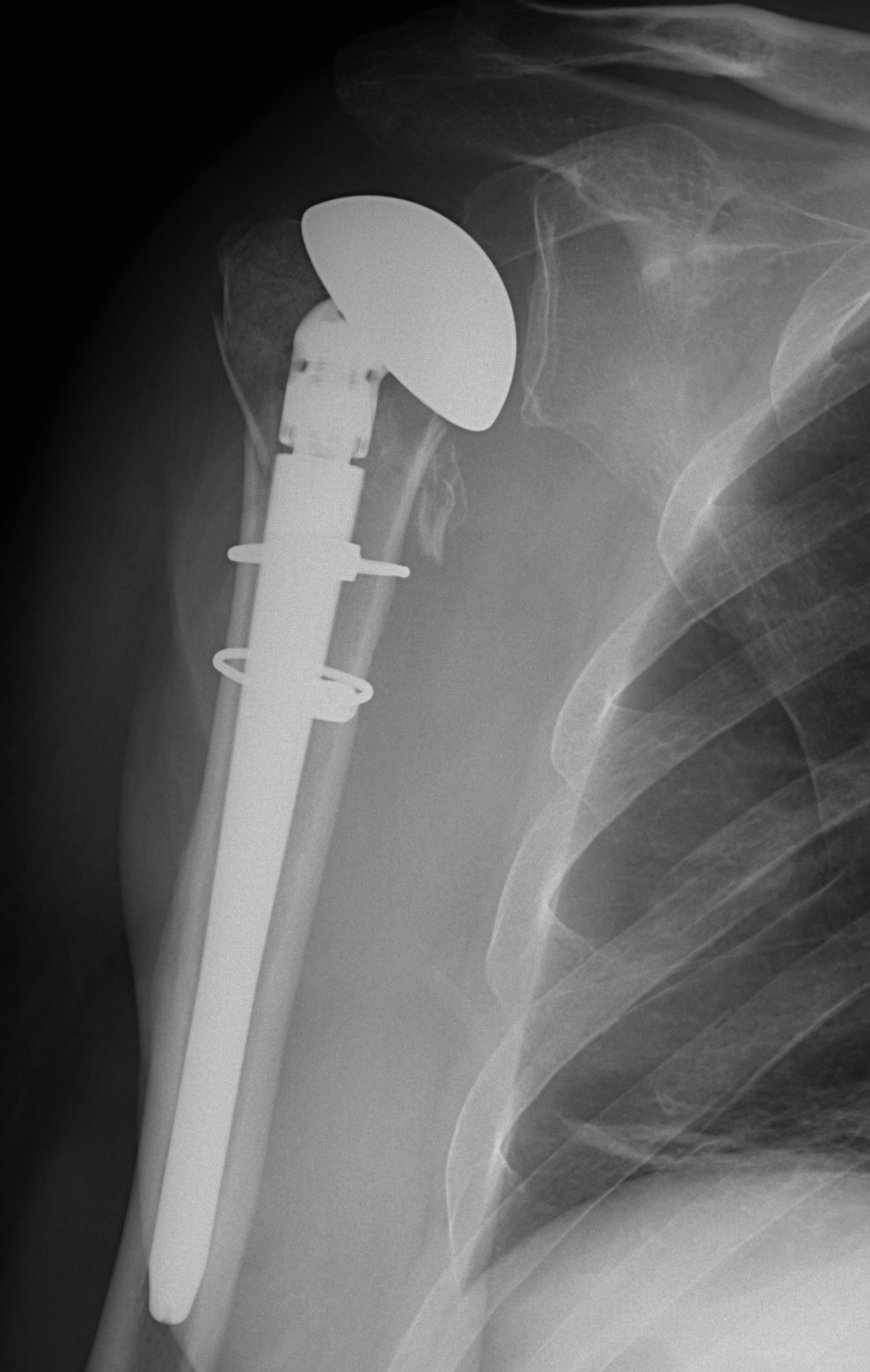
B. Intramedullary Nail
Results
Agel et al J Should Elbow Surg 2004
- 20 patients treated with polaris nail
- 2 proximal failures requiring revision
- 5 delayed unions
C. Hemiarthroplasty / Reverse TSR
Indications
Unreconstructable
Elderly
4 part fractures
Head splitting fractures


Hemiarthroplasty

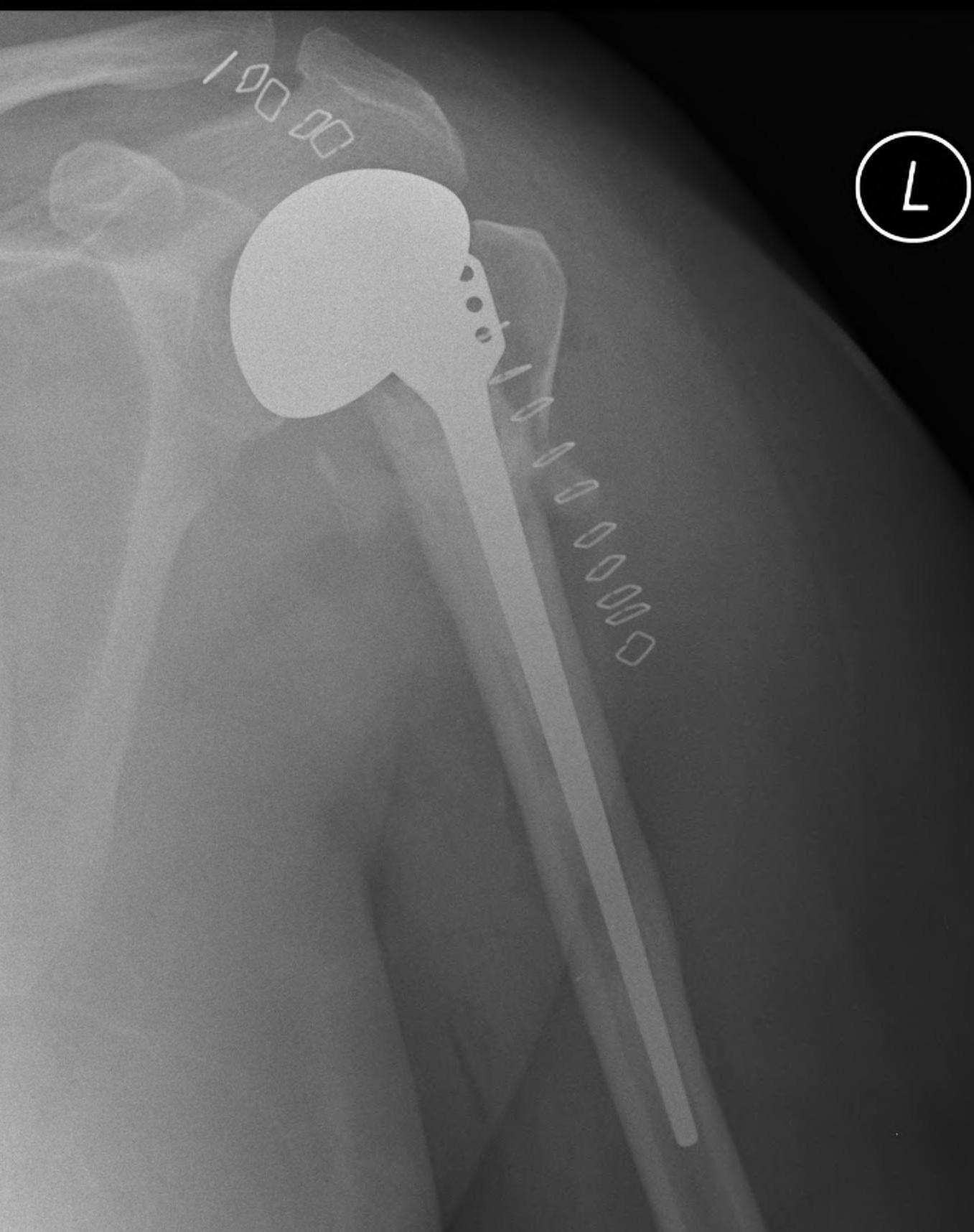
Issues
Must ensure tuberosities heal
ROM often poor / rarely > 90o
ROM
Atuna et al J Should Elbow Surg 2008
- 57 patients with 5 year follow up
- average age 66
- active forward elevation 100o
- 16% moderate or severe pain
Caiet al Orthopedics 2012
- RCT of ORIF v hemiarthroplasty in 4 part fractures elderly
- 32 patients, average age 72 years
- 2 year follow up
- minor advantages in pain relief and ROM with shoulder hemiarthroplasty
Technique
Preoperative template
- often missing proximal neck
- x-ray of other side for reference
- template size, attempt to judge height
Set up
- need to be able to extend humerus to insert stem
- arm over side
- lazy beachchair
- head firmly secured on ring
- 500ml saline back between shoulder blades
Deltopectoral approach
Remove and tag tuberosities
- identify AXN first
- Mason Allen sutures, 2 in each
- often useful to debulk tuberosities
Remove and size anatomical neck
- identify diameter and thickness
- remove bone graft from head for tuberosity fixation
Ream humerus
- trial stem
- important to assess height
- trial with arm hanging to replicate weight
- will usually need to leave stem proud from fracture
- should be able to anatomically restore tuberosities
Need retroversion of 30o
- most prosthesis (i.e. Depuy Global Shoulder system) have an anterior fin
- position to the bicipital groove
- the prosthesis will be retroverted 30o
Need drill holes in humeral shaft
- medial 2 for LT sutures
- lateral 2 for GT sutues
- anterior 2 to pass through both
- no 2 fibre wire
- keep them gliding as the cement sets
Cement with low viscosity Abx cement
- cement restrictor
- nil pressurisation or will fracture
Place on head with 12/14 taper
Repair tuberosities
- use any bone graft available
- 2 x additional sutures through anterior fin
- 1 x additional suture through medial hole
Biceps tenodesis
Close over drain, rehab as above
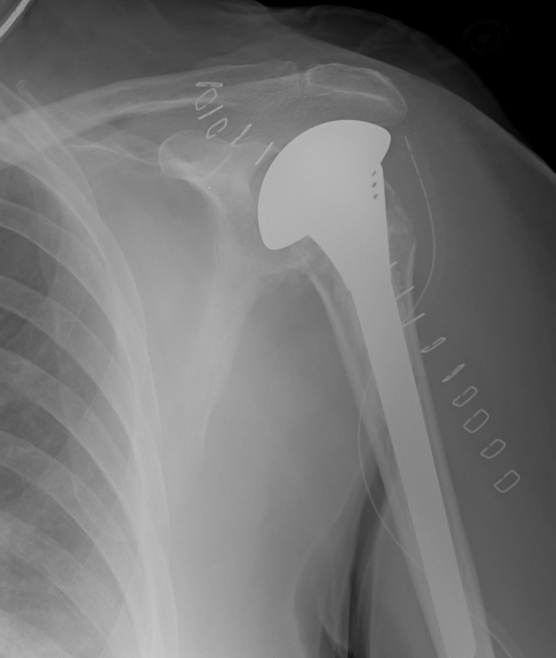
Reverse total shoulder
Indication
- elderly patient
- poor cuff
- poor chance of tuberosity healing
Problems
- reverse has more serious complications (i.e. dislocation)
- techically more difficult to do
- results are not outstanding
Results
Gallinet et al J Orthopaedics and Traumatology
- 21 patients hemiarthroplasty, 19 in reverse group
- forward flexion (90o v 60o) and abduction (90o v 53o) better in reverse
- rotation better in hemiarthroplasty