Epidemiology
Rare
- 2% of acute dislocations
Often missed
- < 1/ 52 25%
- < 6/52 25%
- < 6/12 25%
- > 6/12 25%
Aetiology
Usually secondary major trauma
- MVA
- Seizures
- ECT
- Electrocution
- Alcohol-related injuries
Examination
Loss of ER
Arm kept IR
- Hold arm across chest
Beware of young patient with arm across chest & limited ROM
- don't think frozen shoulder only
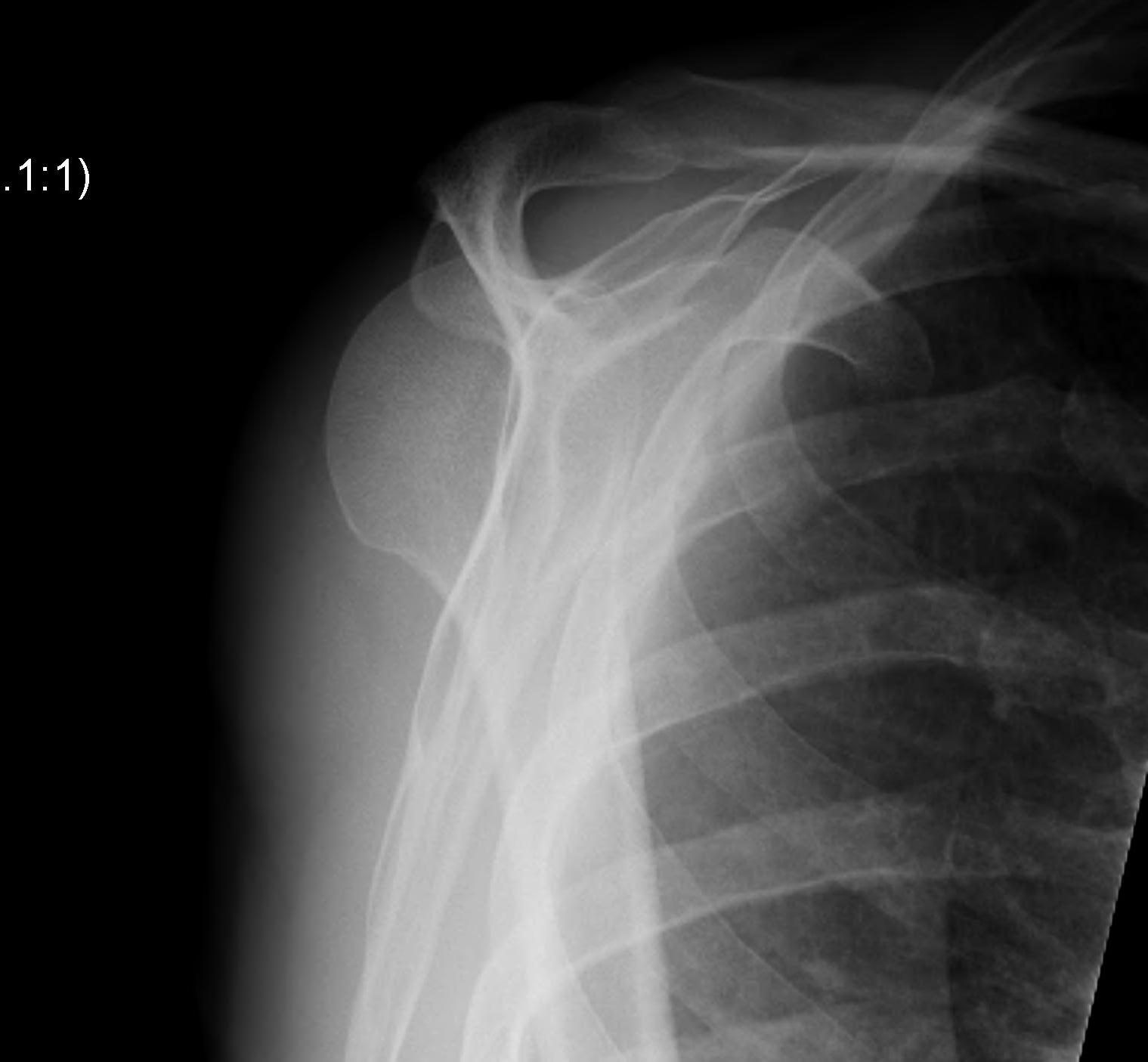
AP Xray
1. Light-bulb sign
- globular head 2° IR

2. Vacant Glenoid Cavity
- > 6 mm space between humeral head and anterior rim of glenoid

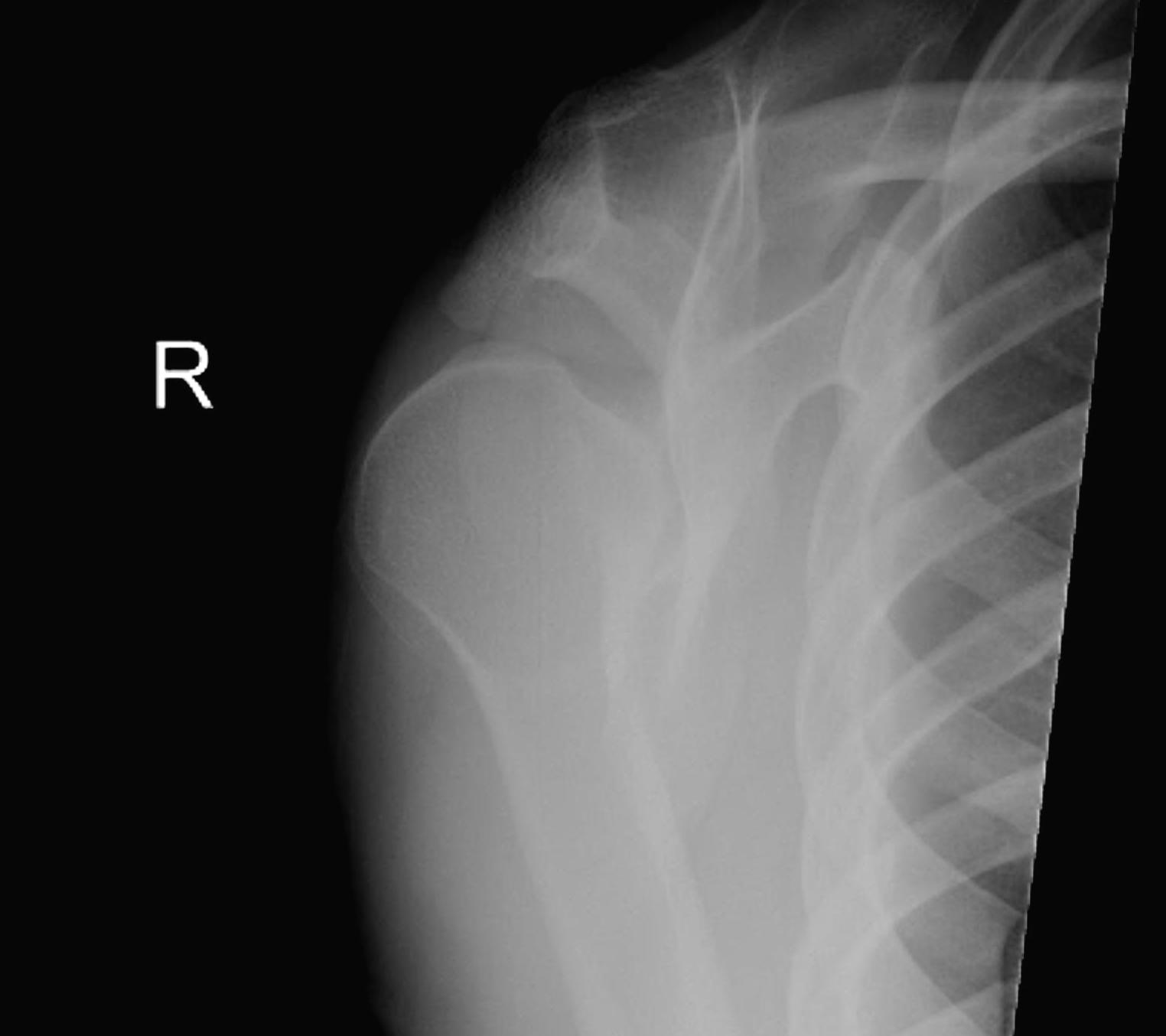
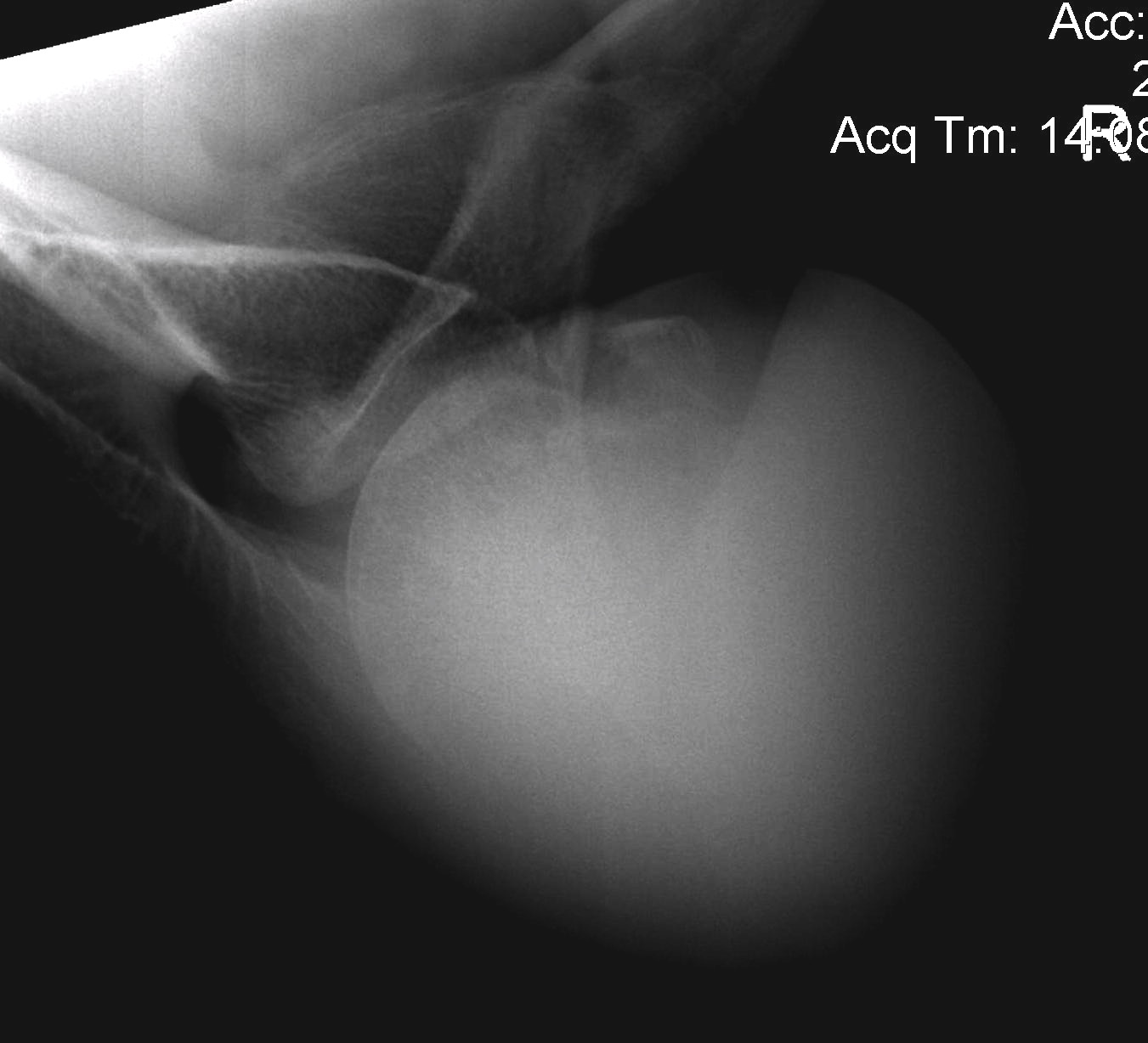
Axillary Xray
Diagnostic
- humeral head posterior to glenoid
Look for reverse Hill- Sachs

Scapular lateral
Can be missed if any obliquity to Xray
- centre of the humeral head must be centred on the Y / Mercedes
- Y is formed by coracoid anteriorly / scapular spine posteriorly / scapula body inferiorly
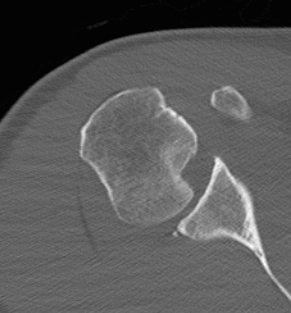
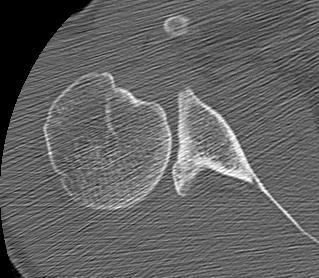
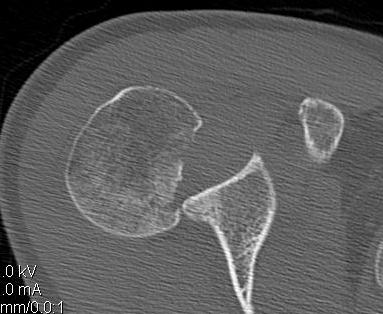
CT scan
A. Confirms dislocation



B. Quantifies humeral head defect
- very important to decide management if locked / chronic / unstable
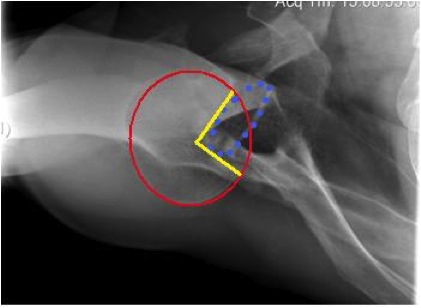
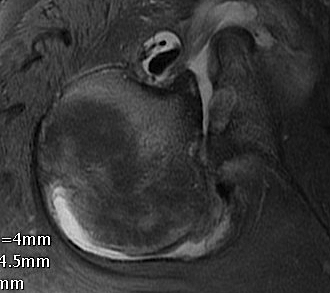
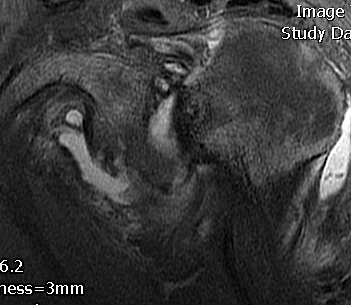
Humeral Head Defect
Quantification
- measured as a percentage of the articular surface
Case 1


Case 2


MRI
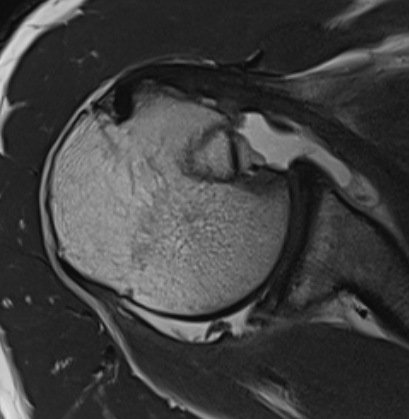
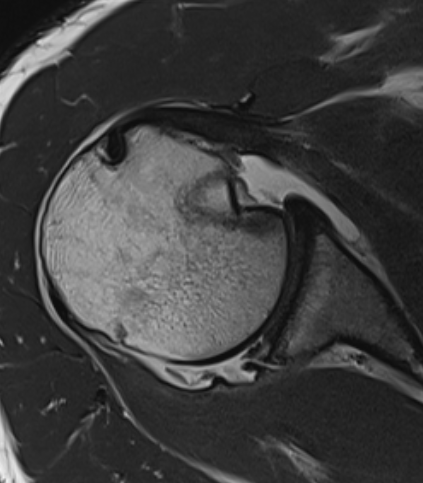
Beware Chronic Case
Management
Closed reduction
Beware
- injury more than 6 /52 ago
- large posterolateral defect locked on glenoid rim
- > 40% defect (will be unstable)
Technique
Consent for
- open reduction
- +/- bone grafting
- +/- McLaughlin procedure
GA
- arm adducted
- arm flexed to 90o
- increasing IR first to unlock head
- traction
Unstable closed reduction
- may have to use gun slinger cast
- arm abducted 90o and ER
Post Reduction
Assess anterior Hill Sachs

Open reduction
Indication
- failure closed reduction
- inability to maintain reduction in gunslinger
- chronic posterior dislocation
Technique
1. Anterior deltopectoral approach
- reduce humeral head
2. Address instability / manage anterior humeral head defect
Humeral head Defect Management
1. HS < 25%
Options
- treat non operatively if stable
- may be able to elevate and bone graft acutely in young patient
- +/- posterior labral repair
2. HS > 25%
Options
- transfer SSC +/- LT
- osteochondral allograft young patient
- hemicap / resurfacing older patient

3. HS > 40%
Options
- hemiarthroplasty / TSR (older patient)
- osteochondral allograft (younger patient)
SSC +/- LT transfers
Options
SSC transfer / McLaughlin
- makes defect extra-articular
SSC + LT / Neer modification
Indications
- best for small defects = 25%
- young patient
Problem
- may weaken IR
Osteochondral Reconstruction




Results
Diklic et al JBJS Br 2010
- 13 patients with anteromedial defects between 25 and 50%
- all chronic / missed injuries
- open reduction
- SSC divided 1 cm from insertion, separated from capsule
- posterior labral repair / posterior plication if required
- femoral allograft inserted and fixed screws
- ER brace post op
- 9 patients pain free, 1 developed AVN, other 2 mild pain
Hemiarthroplasty / TSR
Indication
- older patient
- humeral defect > 40%
Issues
- may get recurrent posterior instability
- may have posteror glenoid bone defect
Technique
- anterior SSC Z lenthening
- posterior capsular plication +/- advancement IS / Tm
- glenoid poly insertion if posterior glenoid wear
- decreasing humeral head retroversion to 20o
- gunslinger post op for 6 weeks
Results
Sperling et al J Should Elbow Surg 2004
- 12 patients, average age 55 years, average 26 months since dislocation
- mix of hemiarthroplasty and TSR depending on state of glenoid
- some posterior plications performed
- 2 patients had recurrent posterior instability
- one patient had advancement of IS / Tm and posterior capsular plication
- one hemi was revised to TSR with plication
