Epidemiology
M:F =2:1
30-40 years
20% diabetic
50-80% identifiable source
Site
Lumbar (50%) > Thoracic > Cervical (<10%)
Pathogenesis
1. Haematogenous
- arterial rather than venous
Risk factors
- UTI (40% of all cases)
- IVDU
- elderly
- respiratory infection
- immunocompromised
- DM
2. Direct spread
- pelvis or psoas
- percutaneous or open spinal procedures
Organism
Staph aureus 60%
Streptococcus
Gm negative
- Ecoli, Proteus
- UTI / GUT procedures
Salmonella in sickle cell
Pseudomonas in IVDU
TB / Fungus
- in immunocompromised
- may require life long therapy
Patients
Elderly
IVDU
Immunocompromised
- steroids
- transplant
- DM, RA
Pathology
Initial focus at end plates
- septic emboli to end arterial circulation
- series of inter-metaphyseal artery allows infection of contiguous vertebrae
- spreads by direct extension to adjacent vertebrae unlike TB
Disc destruction
- disc is avascular
- allows infection to spread here as well
- forms collection / abscess
Deformity
- due to body and disc destruction
- kyphotic
Neurology
- compression from epidural abscess
- infarction of regional supply to cord
- pathological fracture fragments
- kyphosis
Clinical Presentation
Back pain / tenderness + fever + elevated ESR
Diagnosis often delayed 4-6/12 due to vague symptoms
90% back pain
- insidious, non-mechanical, night pain
- localised tenderness
50% fever
< 10% neurological deficit
Bloods
ESR elevated > 90%
- most sensitive test
WCC elevated 35%
Blood culture's
- often negative
- especially if low virulence
Urine culture
Malnutrition
- albumin / lymphocyte count
X-ray
Changes 4-6/52
Findings
- loss of disc height
- end plate irregularities/erosions
- vertebral destruction
- contiguous vertebrae
- collapse usually without severe kyphosis of TB
CT
Soft tissue involvement
Good for TB

Bone Scan
Localise area of problem if diagnostic dilemma
MRI

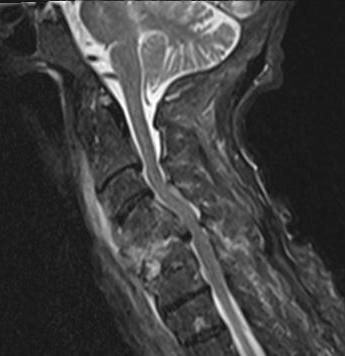
Investigation of choice
- 95% accurate
- diagnose vertebral osteomyelitis
- look for epidural abscess
Early
- T1 loss of distinction between disc and end plate
- T2 loss of normal disc intranuclear cleft
- specific for infection
Gadolinium T1
- ring enhancement
DDx
Tumour
- preservation of disc
TB
- no increased T2 in disc
CT guided biopsy
Indication
- If organism unknown
Technique
- aspiration if abscess
- bone biopsy otherwise
Results
- culture 75% of microbes prior to antibiotics
- only 25% after antibiotics given
Open biopsy
Indication
- if no CT available / unsuccessful
Technique
- posterior approach
- specimen obtained through pedicles
- T-spine through costotransversectomy
Results
- culture aerobic / anaerobic / AFB / fungus
- diagnostic in > 80% cases
TB VS Pyogenic
Pyogenic TB
Single focus Multisegments involved
Symmetric collapse Kyphosis
Spread bone Fascial planes
Disc destroyed Disc sequestered
Anterior column All 3 columns (posterior inv)
Epidural abscess Paravertebral abscess
More acute Insidious
Management
Non-Operative
Principles
1. Important to delay antibiotics until cultures taken
- BC's
- urine M/C/S
- CT biopsy
2. After biopsy
- most settle with antibiotics
- 6-8 weeks IV treatment (until ESR norm)
- continue orals 3-6/12
3. Immobilisation important
- Bed rest
- TLSO
4. Adequate nutrition important
- serum albumin
- WCC
- transferrin
5. Spontaneous fusion occurs in 60%
Operative Management
Indications
1. Biopsy for diagnosis and M/C/S
2. Failure medical management
- systemically unwell
3. Neurological deficit
4. Deformity / instability
Anterior approach & corpectomy
1. Adequate debridement crucial
2. Autograft preferred
- iliac crest, fibula, rib
- can use allograft
3. Instrumentation
- anterior +/- supplemental posterior
Results
Lu et al Neurosurgery 2009
- review of 36 patients treated with corpectomy + titanium cage
- nearly all patients required anterior + posterior instrumentation
- 2 infection recurrences, 1 each with autograft and allograft
- all had neurological improvement
- 81% pain free
