Definition
Heterogeneous group of diseases characterised by
- hyperuricaemia
- recurrent attacks of acute arthritis
Diagnosis confirmed by
- crystals of Monosodium Urate in synovial fluid
- tophi ("Porous stone") urate in soft tissues
- renal urate stones
Epidemiology
Adult men
- M:F = 20:1
- peak 40-60 years
Part of metabolic syndrome
- obese / HTN / high cholesterol / diabetes
Often have positive FHx
Physiology
Prerequisite is hyperuricaemia at some stage
- determined by balance between production & excretion
Production
- breakdown of nucleic acids
- oxidation of Purine bases (Guanine & Adenine)
- converted Inosine > Hypoxanthine > Xanthine > Uric Acid
Excretion
- 2/3 excreted into urine
- 1/3 into GIT
- uric acid filtered at glomerulus
- reabsorbed in PCT
- secreted in subsequent PCT
Classification
A. Overproducers ~ 10%
Primary
Disturbance of Purine biosynthesis secondary to heritable error of metabolism
- usually idiopathic
- some specific enzyme known eg Lesch-Nyhan syndrome
Lesch-Nyhan Syndrome
- rare
- X-linked recessive
- absence of enzyme in purine pathway HGPRT
- leads to excessive uric acid formation & gout
- young boys with mental retardation and self-mutilation
Secondary
Diet high in purines
- alcohol / meat / seafood
Myeloproliferative disease
- leukaemia
Chronic hemolysis
Chemotherapy
Drugs eg salicylates, thiazide diuretics
Starvation, ketoacidosis
Alcoholism
B. Under-excretors ~ 90%
Secondary abnormal renal excretion of Uric acid
- diuretics
- CRF
Pathogenesis
Acute Gouty Arthritis
Sustained hyperuricaemia
Develop monosodium urate deposits
- in synovial lining cells & in cartilage on PG which are inert
- subsequently released into synovial fluid & CT
- precipitates at > 8 mg/dl (trauma, low pH)
Sufficient number of crystals in joint precipitates acute inflammation
- phagocytosis of crystals
- release of chemotactic factors & inflammatory mediators
- activate complement & platelets
- disrupt lysosomes in leucocytes with cell rupture
Chronic Gouty Arthritis
Tophi of Monosodium Urate Monohydrate Crystal aggregates
- deposited in synovium, cartilage & tendon sheaths
- lead to cartilage destruction & periarticular cyst formation
4 stages
1. Initial asymptomatic hyperuricaemia
2. First attack of acute gouty arthritis
3. When this settles, hyperuricaemia persists
- recurrent attacks
- frequency of attacks varies, may increase
4. Chronic gout
- joints no longer recovering from acute attacks
- arthritis & tophi develop
NHx
Hyperuricaemia
- in men begins at puberty
- in women starts at menopause
Risk of gout increases with
- serum urate level
- duration of hyperuricaemia
- usually develops after 20-30 years
Only 5% of hyperuricaemic patients develop gout
Takes days / weeks to resolve
- pain-free intervals of variable length
Clinical presentation
Acute Gouty Arthritis
Predominantly affects distal lower limb
- 70% initially attack 1st MTPJ (Podagra)
May also involve
- Other joints in foot
- ankle
- knee
- hands
Usually monoarticular, rapid onset
- excruciating night pain
- hot red shiny swollen joint
- very painful to touch
- may have systemic features
- fever / leucocytosis / raised ESR
Onset may be spontaneous
May be precipitated by
- trauma
- excessive activity
- diet excess
- alcohol consumption
- diuretics
- systemic illness
- surgery
Chronic Gouty Arthritis
Arthritis
- after repeated attacks of gout
- asymmetric destructive arthropathy
- often involves small joints in hand
Tophi
- 20% of cases
- white mass of sodium urate crystals
- visible underlying thinned-out skin
- may necrose overlying skin
Sites
- periarticular subcutaneous tissue
- helix of ear
- tendon sheaths especially Achilles
- olecranon / prepatellar bursae
Renal Stones
- 15% of cases
- radiotranslucent uric acid stones
Investigations
Serum Uric Acid
Attacks of gout occur when levels of serum uric acid change
- not necessary to have increased serum urate during acute attack
- elevated serum urate in patient with painful joint not diagnostic of gout
Synovial fluid
Specimen must be anticoagulated
- must be very careful with sample as any water or alcohol put into it will dissolve the crystals
Monosodium urate crystals
- diagnostic if found in synovial fluid
- needle-shaped crystals 10um long
- lying free or in neutrophils
Test
- negatively birefringent under polarised light & parallel to 1st order red compensator
- bright yellow when parallel to compensator
Synovial fluid analysis
- WCC of 1000 to 70 000 x 10.6/ L
- predominantly neutrophils (< 70%)
Note
- presence of crystals doesn't exclude infection
- infection precipitates urate
24 hr Urinary Uric Acid Secretion
> 1100mg /day
- 50% chance renal stones
- treat with Allopurinol
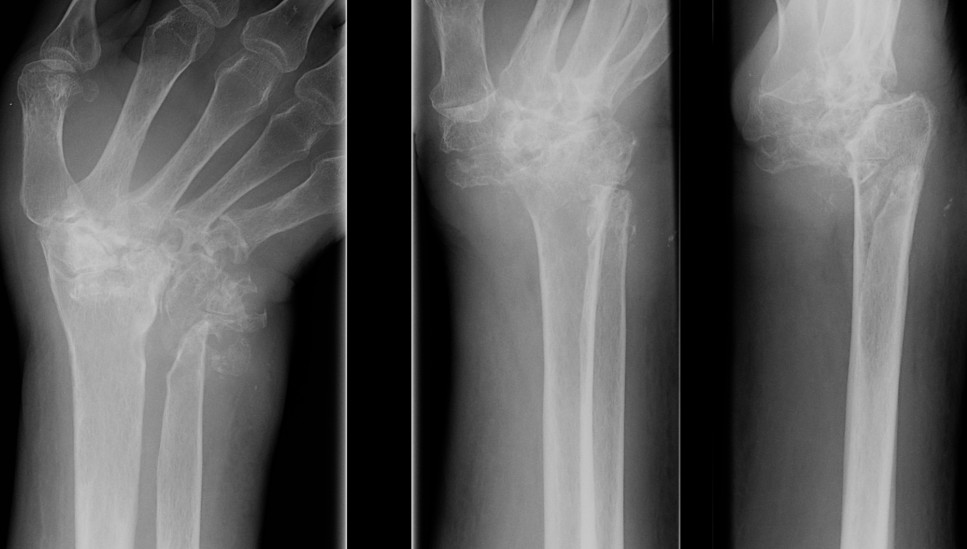
X-ray
Chronic Gouty Arthritis
- usually in feet in phalangeal heads
- characteristic periarticular bony defects
- punched out lytic appearance
- overhanging sclerotic margin (Martell's sign)
- also joint space narrowing & secondary OA
- no osteopenia compared with RA
DDx
Pseudo-gout
Septic arthritis
Acute bursitis
Cellulitis
RA
OA
Seronegative spondyloarthropathy
Management
Acute Gout
Medications
Colchicine
Action is as anti-inflammatory
- inhibits activation of inflammatory mediators by crystals
- very effective
- rapid response strongly suggestive of diagnosis
- 1 mg then 0.5 mg q2h up to maximum 6 mg / day
- continue till patient improves / diarrhea occurs / maximum dose
- 80% of patients unable to tolerate optimum dose because of GIT side-effects
NSAID
Usually better tolerated than colchicine
- indomethacin most commonly used
- 50 mg t.d.s
- side effects include GIT toxicity / Sodium retention / CNS disturbance
ACTH
Adrenocorticotrophic Hormone
- good for acute attack
- minimal side effects
- single 40 IU IM injection
Glucocorticoids
Oral Prednisone
- if colchicine not tolerated / NSAID contraindicated
Intra-articular steroids
- may be used for severe monoarticular attack
- especially knee
Prophylaxis
3 Tier Approach
Initial
Lose weight
Increase fluids intack
Aim to decrease Purine intake and avoid precipitating factors
- alcohol
- diuretics
- diet - meat, seafood
2nd Stage
- Probenecid
3rd Stage
- Allopurinol
- beware hypersensitivity / bone marrow suppression
Antihyperuricaemics
Absolute indications
- CRF secondary to kidney stones
Relative indications
- > 3 acute attacks / year
- polyarticular gout
- tophi
- uric acid > 500 mmol/l
Options
1. Increase Renal Uric Acid Excretion / Uricosuric
- Probenecid
- require good renal function
2. Decrease Uric Acid Synthesis
- Allopurinol
Allopurinol
Inhibits Xanthine Oxidase
- 300 mg/day (150 if CRF)
- hypersensitivity side effects in 20%
Causes decrease in serum uric acid & this may precipitate acute attack of gout
- initiation of treatment should be accompanied by Colchicine or NSAIDS
- never used in acute gouty attack
- can shrink tophi if keep serum urate < 0.4mmol/l
Side effects can be fatal
- rash
- alopecia
- marrow suppression
- hepatitis
