Epidemiology
Extremely common
- 90% by 10 years have wrist problems
Principles
Landsmeer 1961
- treat wrist at same time as treat fingers or will recur
Frequently combine procedures
- synovectomy
- tendon transfer
- ulna procedure
Treatment Priorities
1. Pain Control
2. Slow progression
3. Restore / Function
4. Cosmetic Improvement
Pathology
1. Synovitis
Starts
- ulna styloid
- ulna head
- scaphoid midportion
Radial side
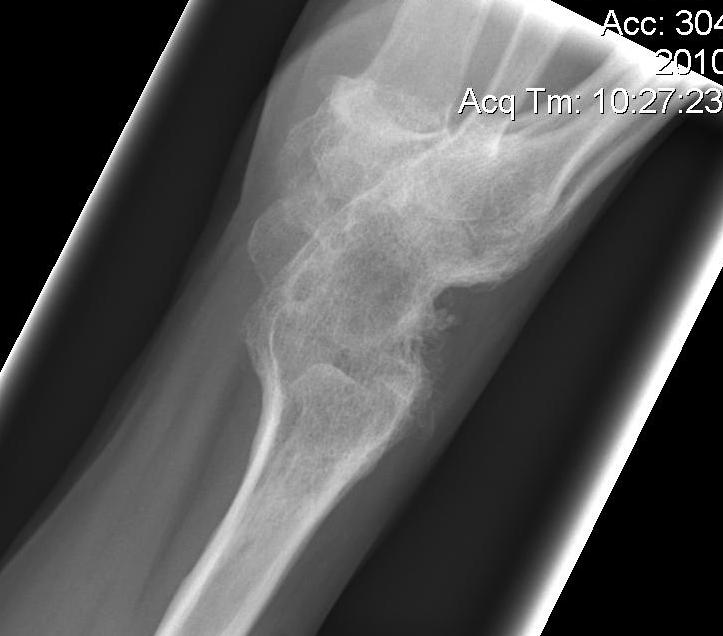
- synovitis scaphoid midportion
- RCL & RSCL become attenuated
- subluxation of scaphoid & scapholunate dissociation
- radiocarpal shortening
Ulnar side
- synovitis begins ulna styloid
- TFCC, ULL & UTL attenuated
- DRUJ stretches
- volar subluxation of ulnar carpus & supination
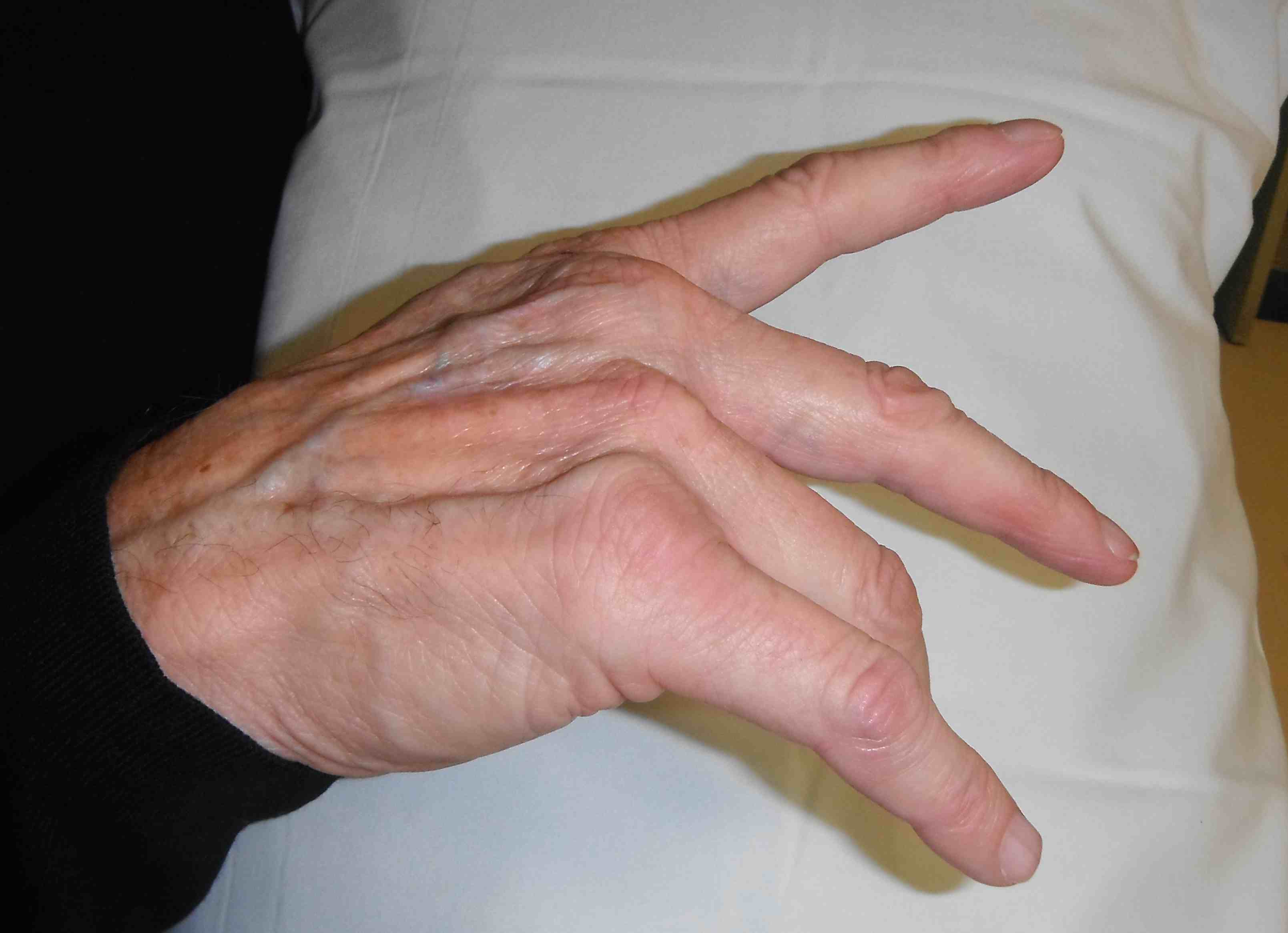
- develop caput ulna
- ulnar becomes prominent because carpus is falling away from it
- carpus volar translated & supinated

2. Loss of ECU mechanical advantage
- secondary to supinated carpus & carpal collapse
- ECU subluxes volar to flexion / extension axis
- increases mechanical advantage of radial wrist extensors
- radial deviation of carpus
3. Carpal Collapse
- decreases mechanical advantage of long finger flexors / extensors
- leads to intrinsic plus deformity


Failure to address wrist deformity will lead to failure of MP or IP reconstruction
Operative Management
Indications
Failure of optimal rheumatology supervised medical management for 6 months
Options
Preventative
- synovectomy
- tendon transfers
- CTD
- tendon repairs
Salvage
- DRUJ excision
- arthrodesis
- arthroplasty
1. Synovectomy
Indications
Persistent painful wrist synovitis not settling with medical management
- > 6/12
- minimal X-ray changes
Advantages
1. Relieves pain
- no evidence synovectomy alone will halt progression of wrist deformity
2. Prevents subsequent tendon rupture
- recurrent tenosynovitis rare
- once one tendon ruptures often followed by multiple ruptures
- tendon rupture can occur by direct invasion
- seen in up to 50% at time of tenosynovectomy
Operations
A. Flexor tenosynovectomy
Often difficult to diagnose
- not as easily seen as dorsally
- patients present with limited active finger flexion / CTS
Technique
- through incision of CTD
B. Dorsal Tenosynovectomy + Carpal Synovectomy
Clinically
- dumbbell shape under extensor retinaculum dorsally
Midline dorsal incision
- divide extensor retinaculum between 5th and 6th extensor compartments (EDM & ECU)
- elevate radially based flap to 1st compartment
- perform partial wrist denervation (PIN in floor of 4th)
RCJ & Intercarpal joints exposed
- use ligament sparing arthrotomy (between DRC and DIC ligaments)
- synovectomy
DRUJ exposed through longitudinal incision
- debride
- stabilise if unstable
Repair extensor retinaculum underneath tendons to protect bed
2. Tendon Transfer
ECRL to ECU insertion
Timing
- at time of synovectomy
Advantages
A. Corrects a correctable radial deviation deformity
B. Holds ECU over ulna head
- prevents ulna subluxation
3. CTD
Cause
Secondary to synovitis
Management
- good results with decompression
- usually perform flexor tenosynovectomy at same time
- may wish to examine floor to ensure no bone protruding which may rupture tendons
4. Tendon rupture
A. Extensor tendon rupture


Sequence
- EDQ > LF > RF > MF > IF > EI
- goes ulna to radial
- opposite to flexor tendons
Cause of rupture
- tenosynovitis
- caput ulna (EDQ)
- EPL over Lister's tubercle
Extensor Digiti Quinti / Vaughan-Jackson Syndrome
5th dorsal compartment
- can be clinically silent
- EDC and juncturae tendinae compensate
Diagnosis
- attempt to hold LF extended whilst other fingers flexed
- indicates that progressive tendon rupture likely and intervention required
DDx dropped finger
- extensor tendon subluxation
- MCPJ dislocation
- dislocated extensor tendons
- PIN palsy (can't extend wrist or thumb)
- locked trigger
Extensor Tendon transfers
LF rupture
- side to side RF
LF / RF
- side to side MF
LF / RF / MF
- LF / RF to EI
- MF to IF
- or RF FDS to LF / RF
LF / RF / MF / EI / IF
- RF & MF FDS
B. Flexor tendon rupture
Mannerfelt lesion
- distal pole of scaphoid and trapezium erode through volar capsule
- FPL most common
- FPL / FDP IF / FDS IF / MF
- opposite direction to extensors
Management
In severe deformity, may wish to fuse wrist to prevent further ruptures
Approach
- bed of FCR
- carpal tunnel incision
Debride bony prominences
- rotated capsule to cover floor
FPL rupture
- fuse IPJ
- young patient transfer FDS IF / RF +/- PL graft
IF FDP
- fuse DIPJ
IF FDP / FDS
- fuse DIPJ
- MF FDS transfer
5. DRUJ


Clinically
Frequently subluxes dorsally
- ECU may also be ruptured
Patient presents with pain with rotation
- may have extensor tendon rupture
Piano Key sign
- reduce the ulna, it simply redislocates
Options
A. Darrach's

Principle
- excision arthroplasty
Indications
- older patient
Technique
- same dorsal approach as for synovectomy
- radial based ER flap
- excise distal ulna
- proximal limit is articulation with sigmoid notch
- usually 1.5 cm
- round off radial side
- stabilise with volar capsule + ECU tenodesis
- can stabilise with Pronator Quadratus
Complications
- can be unstable
- even with ECU tenodesis
- revise by ECU / FCU tenodesis + pronator quadratus interposition
- or by further shortening!!!
B. Suave - Kapandji
Principle
- fusion DRUJ & ulna pseudoarthrosis
Indication
- younger patient
Technique
- resection of 10 - 15 mm long segment of ulna proximal to DRUJ
- resect proximal periosteum +/- interposition of pronator quadratus to prevent regrowth
- DRUJ denuded of cartilage
- distal fragment brought slightly proximally to prevent ulno-carpal abutment
- fuse to distal radius with screws or K wires
- 4 weeks in LA POP in neutral
Results
- may have better result than Darrach's in RA
- less instability
C. Hemi-resection arthroplasty
Not usually done in RA
- TFCC and DRUJ soft tissues very poor
- indicated for DRUJ arthritis with good soft tissue stability
D. Arthroplasty
6. Wrist Fusion
A. Partial Wrist Fusion
Options
- Radiolunate / Radioscapholunate fusion
Indications
- isolated arthritis
- midcarpal joint spared
Results
- usually have to do wrist fusion later
- may maintain some movement for 5 years or so
B. Total Wrist Fusion

Advantage
- predictable
- stable and pain free wrist
Indications for Arthrodesis
- poor bone stock
- stiff wrist
- loss of wrist extensors
- painful erosive RA
- high demand
Techniques
A. Steinmann pin in third MC / Mannerfelt Fusion
B. Plate fixation


Gold standard
- Synthes low profile contoured plate
- 10o degrees extension
- fused to MF metacarpal
- avoid radial deviation
- ulna deviation OK
Bilateral one up one down
Complications
- functional difficulties
- i.e. opening jar
7. Arthroplasty
Indications
- low demand patient that requires ROM
- intact wrist extensors
- good bone stock
Results
Millander 1986
- 25% revision rate at 5 years
