Definition
Idiopathic inflammatory condition
- characterised by progressive shoulder pain & stiffness
- due to contracture of capsuloligamentous structures
- spontaneously resolves
Epidemiology
2% incidence
- 40 - 60 years
- Women 2:1
Sedentary workers
- Non-dominant limb
Bilateral in 10 - 40%
Aetiology
Primary
- Unknown
- ? Autoimmune theory
Associations
- diabetes - 35% IDDM > 10yrs
- yhyroid disorders
- stroke
- MI
- cardiac surgery
- neurosurgery
- dupuytren's
Not Associated with
- OA
- Cuff Pathology
Secondary
Intrinsic
- post surgery i.e. RC
- trauma i.e. SNOH, stabilisation
- immobilisation
Extrinsic
- cervical radiculopathy
- axillary node clearance
- long period immobilisation
Classification Neviaser
Each lasts 4-8 months
1. Freezing
- painful stage
- capillary proliferation, synovial hypertrophy
- develop capsular adhesions
2. Frozen
- decreasing pain, increasing stiffness
- maturation and development capsular contractures
3. Thawing
- decreasing stiffness
Pathology
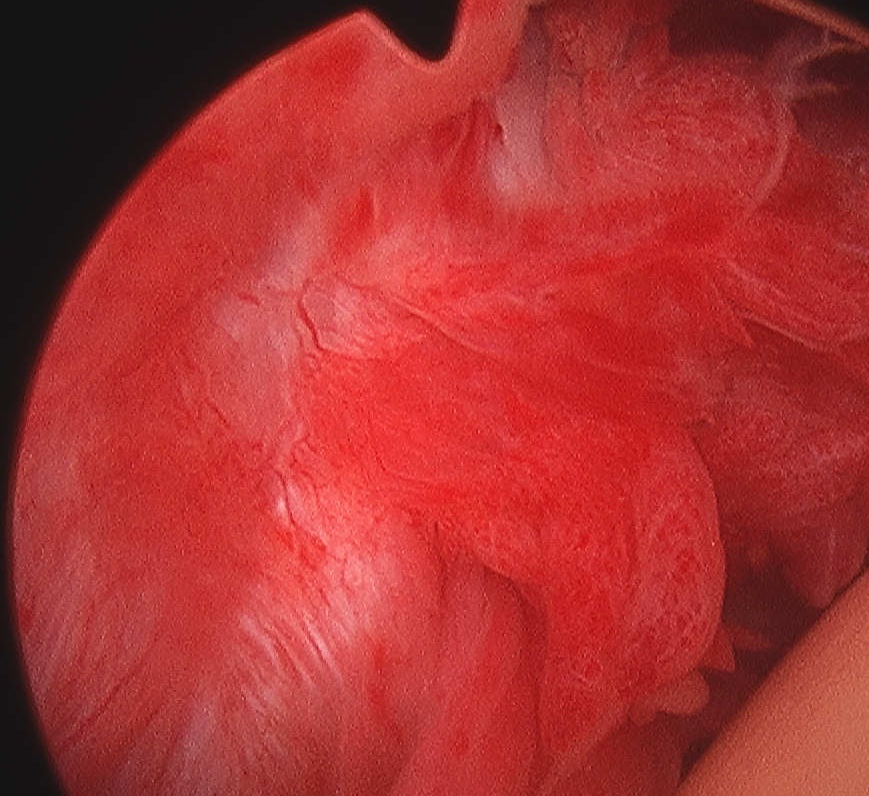
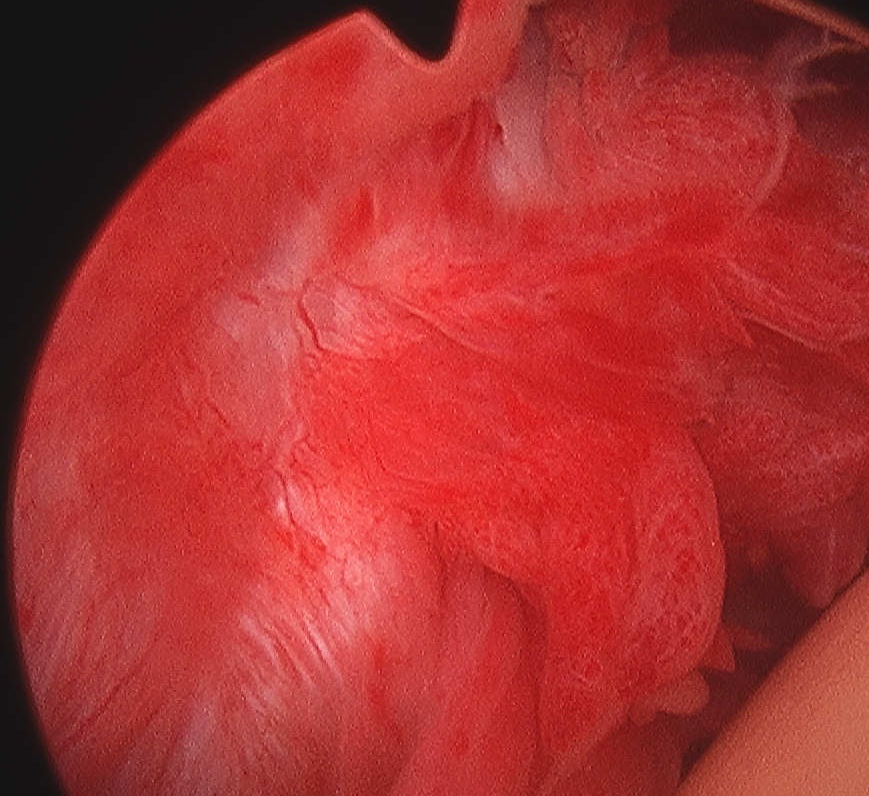
Neviaser described pathology of frozen shoulder
- contracture of capsuloligamentous structures
- inflammation followed by fibrosis
Cellular basis poorly understood
- a dense matrix of type 1 and II collagen
- laid down by fibroblasts and myofibroblasts
1° Frozen Shoulder
Initial synovitis of unknown cause results in
- intra-articular adhesions
- capsulitis
- obliteration of inferior axillary fold
Subsequent development of
- subacromial adhesions
- rotator cuff contracture
Eventually spontaneous resolution
2° Frozen Shoulder
- much less synovial inflammation
- 2° due to either intrinsic or extrinsic cause
Natural History
Traditionally thought to be benign & self-limiting
Grey 1978
- 24/25 resolved by 2 years
- Maximum 10 years
Most have no significant symptoms or functional restriction
- But not as benign as previously thought
Reeves 1975
- 60 % have residual decreased ROM
- usually limitation ER
- only 6% claimed functional disability
Shaffer 1992
- 50% pain or stiffness at mean 7 years
- never more than mild with little functional disability
History
Insidious onset / No history of trauma
Pain
Initially
- at site of deltoid insertion
- at extremes of motion
Becomes more
- diffuse / severe / constant
- interferes with sleep
Then begins to decrease
- rest pain disappears
- pain only on movement
Stiffness
Develops after onset of pain
Difficulty reaching
- overhead
- behind back
Examination
Muscle atrophy
No point tenderness
Markedly decreased ROM
- abduction
- ER classically
- limited GH movement, increased ST movement

DDx Causes of reduced ER
1. Frozen shoulder
2. OA
3. Unreduced posterior dislocation
Pain on forced movement
- most sensitive indicator is pain on forced ER
Xray
Normal
Arthrogram / MRA
1. Reduced volume
- <10 ml of contrast can be injected
- normal = 20-30 ml
2. Obliterated axillary capsular recess
3. Thickened capsule
Management
Goals
- Relieve pain
- Restore range
- Remove secondary cause
Non Operative
Reassurance as first treatment
Careful explanation of
- nature of disease
- NHx
- reassurance
Algorithm
Freezing Phase
- directed towards pain relief
- simple Analgesics / NSAID
- sling / ice / TENS
- intra-articular HCLA
- avoid physio as makes it more painful / doesn't increase ROM
Frozen Phase
- encourage hand use to avoid RSD
Thawing Phase
- gentle ROM & strengthening
- consider intervention if prolonged / major functional disability
HCLA
Lorbach et al J Should Elbow Surg 2010
- compared oral corticosteroids to 3 doses of intra-articular corticosteroids
- best ROM and pain relief in intra-articular group although both effective
Operative Options
1. MUA
Timing
- at least after 6/12
- in late frozen or early thawing phases
Contra-indications
- osteopenia
- previous fracture or surgery
- history instability
Complications
- fractures & dislocations
- cuff tears
- increased inflammation & scarring
Technique (Neviaser)
- GA or interscalene block
- confirm diagnosis with MUA (i.e. limited ROM)
1. Abduction first
- gentle, 2 fingers
- sensation of tearing is the axillary fold tearing
2. Rotation second
- must avoid fracture
- IR / ER in abduction
3. HCLA +/- hydrodistension
Post-op physio
Results
Weber Clin Rheum 1995
- average 6 months post diagnosis
- 73% full recovery
- needed 6 weeks off work
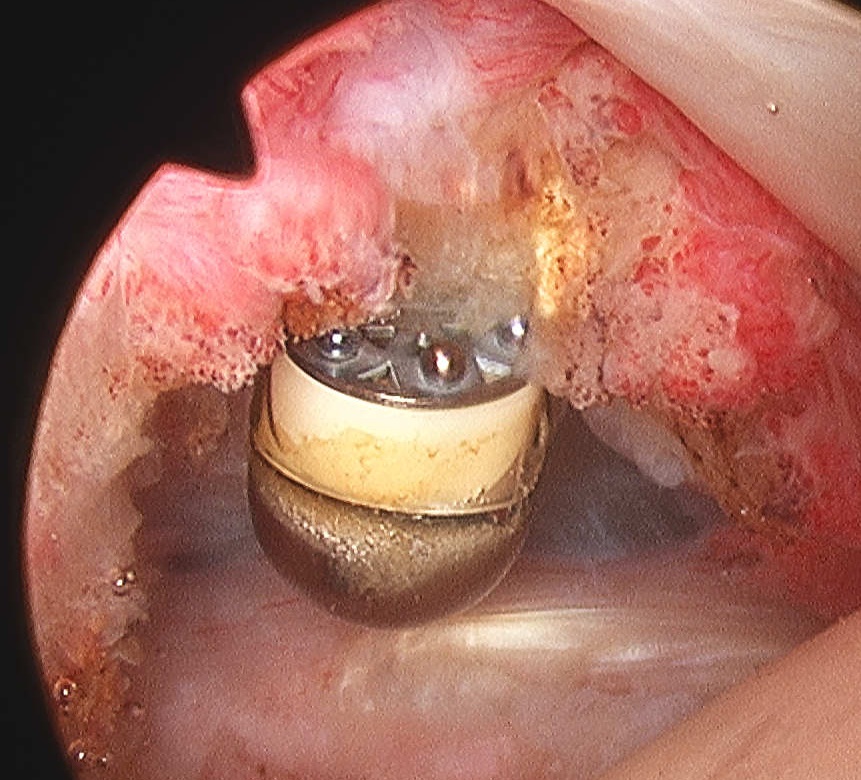
2. Hydrostatic Distension
Technique
- needle into GHJ under LA
- joint forcefully distended by injection
- 5 ml LA
- 1 ml steroid
- up to 40 ml Saline
- distension till capsular ruptures
- sudden drop in resistance
- immediate post-op physio
Results
Rydell Clin Orthop 1992
- 22 patients
- 15 months
- MUA + hydrodistention + steroids
- 91% no or slight pain at 6 weeks
- 83% normal or almost normal ROM
Jacobs J Should Elbow Surg 2009
- 53 patients randomised to either MUA or steroid hydrodistention
- 2 year follow up
- no difference in two group
Quraishi et al JBJS Br 2007
- randomised trial of MUA v hydrodistention
- improved ROM in both groups
- more patients satisfaction and better shoulder scores in hydrodistention
3. Open Release
Ozaki et al 1989 JBJS Am 1989
- one of first papers
- open release CH ligament and RC interval
- mean of 10 months post diagnosis
- MUA as part of procedure
- 94% relief of pain and complete ROM
Segmuller et al J Should Elbow Surg 1995
- released inferior and middle GH ligaments
- 24 patients
- 88% satisfied
- 76% normal function
4. Arthroscopic release
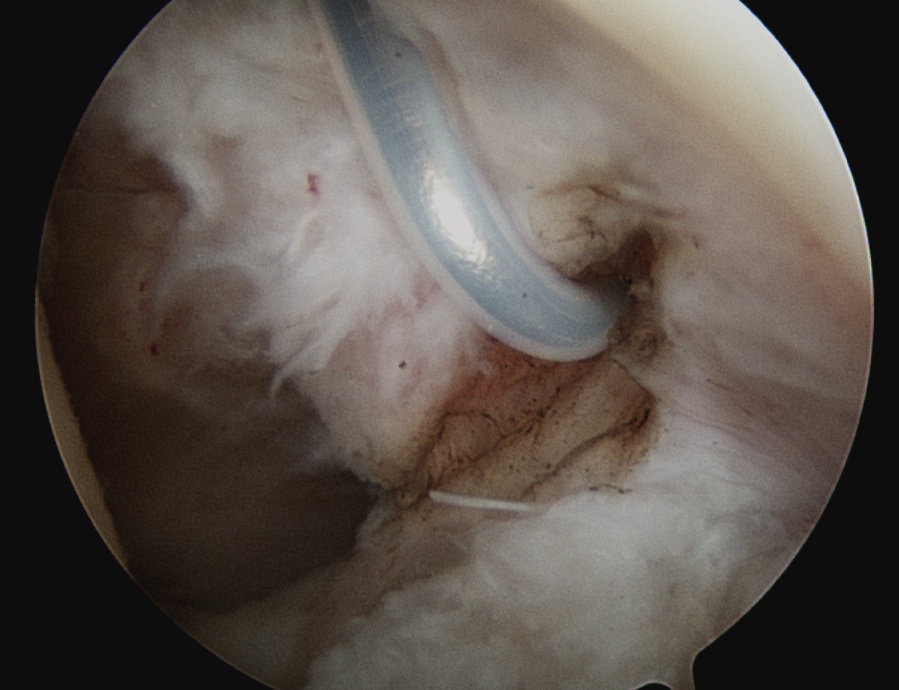
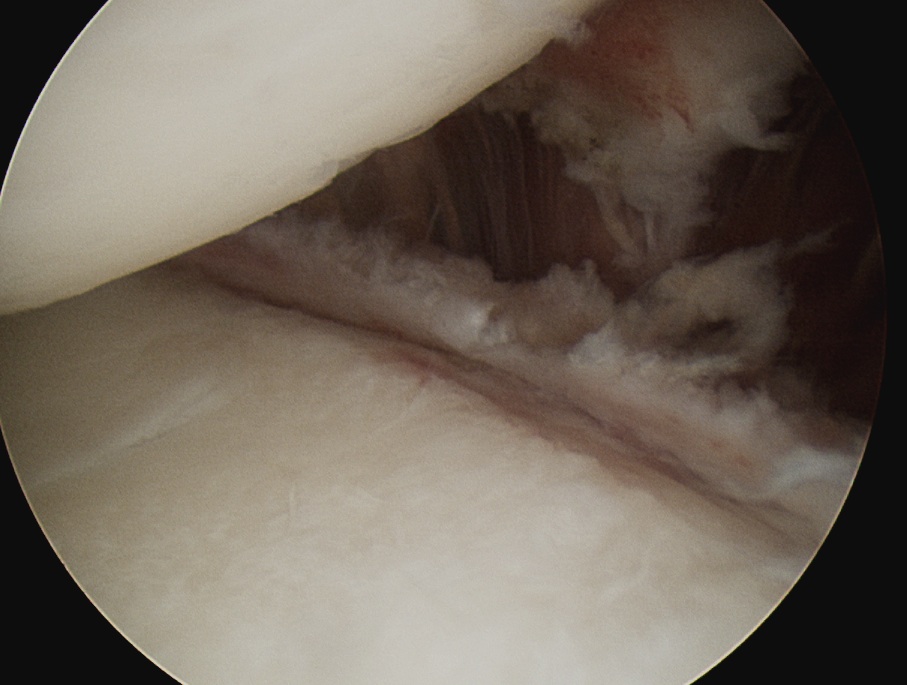
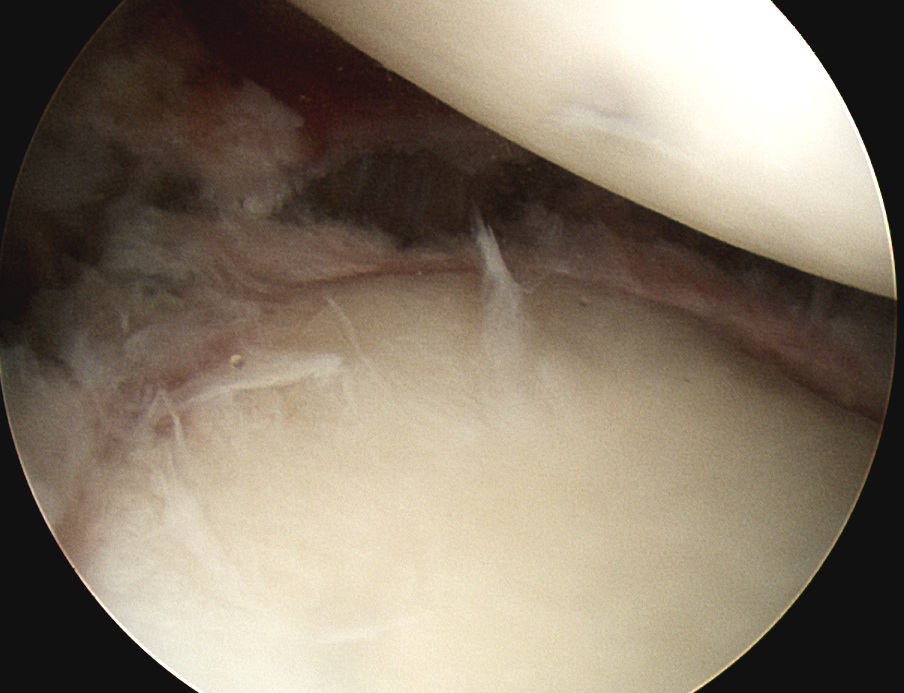
Diagnosis
- +++ synovitis
- very tight shoulder to arthroscope
- capsule very thick
- very limited ROM
Technique
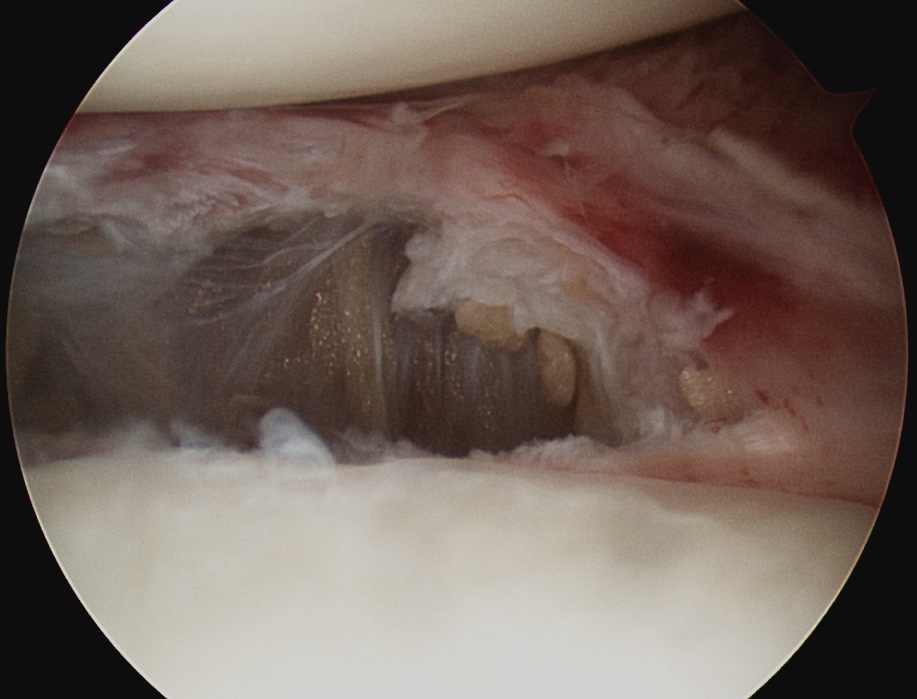
1. Release rotator interval
- remove all tissue in between biceps and SSC
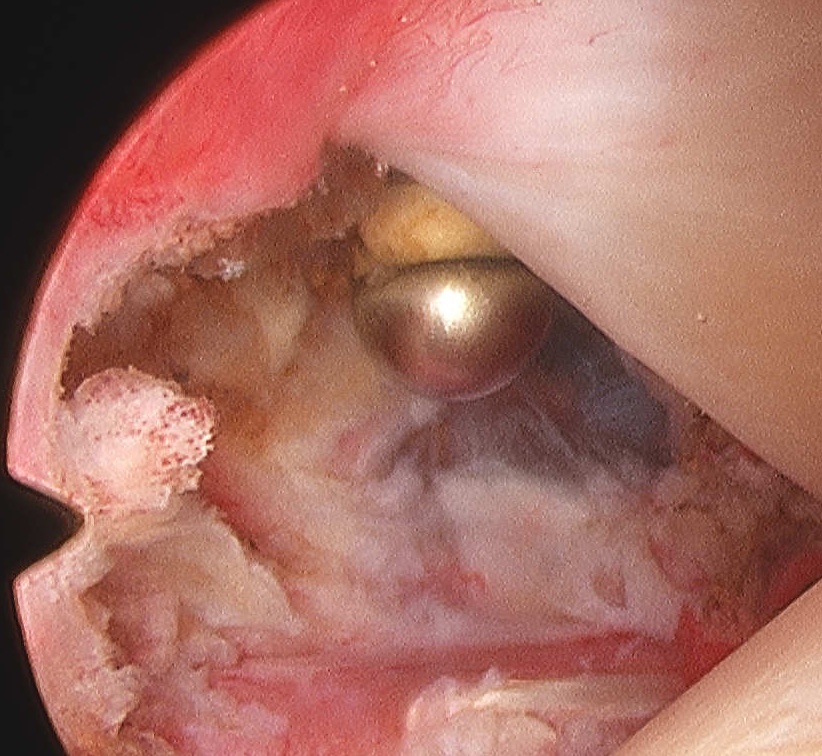
2. Release anterior IGHL
- from 3 o'clock down to 5 o'oclock
- leave labrum intact / anterior to labrum
- release inferior capsule with scissors / 6 o'clock

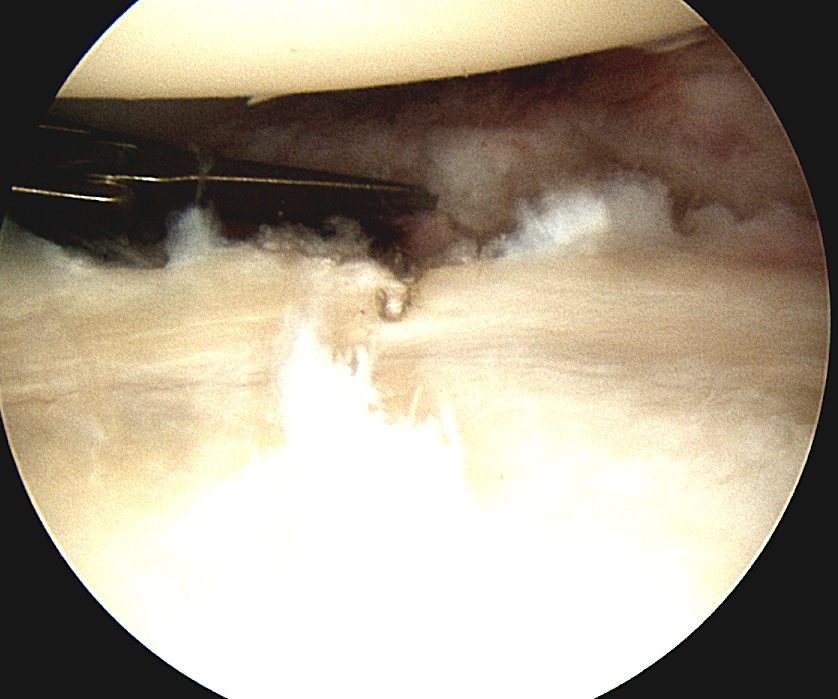
3. Mobilise SSC
- release adhesions on posterior and superior aspect
- some advocate release of intra-articular tendinous portion
4. Release posterior IGHL
- place camera in anterior portal
- posterior to posterior labrum
- complete inferior release
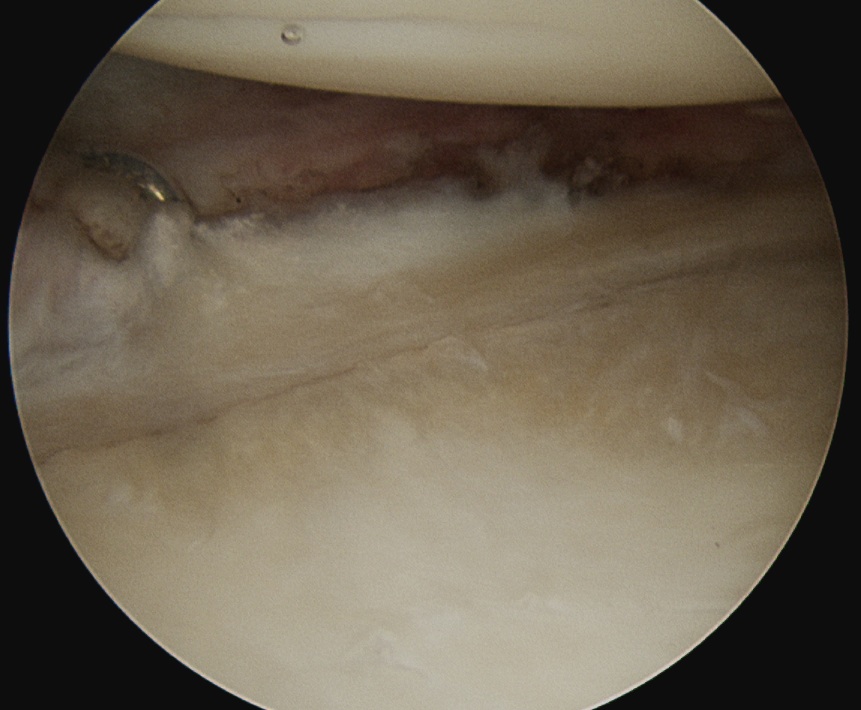
5. MUA with abduction
- remove instruments and camera
- tears inferior aspect of capsule
6. Injection of HCLA
Results
Ogilvie-Harris et al Clin Orthop 1995
- MUA v arthroscopic release in 40 patients
- better outcomes in arthroscopic release at 2 and 5 years
- excellent in 15/20 arthroscopic
- excellent in 7/18 MUA
