
Timing
Early < 3 - 6 months
- most common
- excessive hip position by patient
- before adequate muscle control & soft tissue healing
Secondary 6 months - 5 years
- represents majority of recurrent dislocations
- component malposition / soft tissue tensioning
Late dislocations > 5 years
- typically due to polyethylene wear
Management first time dislocation
Reduction with conscious sedation
You tube video reduction posterior THA dislocation
Hip precautions
Post operative
- abduction pillow
- no driving, high chairs, low cars 6 weeks
- no crossing legs
Korfitsen et al Acta Orthop 2023
- systematic review of 8,800 patients
- no evidence that hip precautions (flexion / adduction / internal rotation) decrease dislocation rates
Natural History
- 136,000 THA in Swedish Registry
- 30 day dislocation rate 0.9%
- 50% had re-dislocation within first year
- 10% required revision for dislocation
Recurrent THA dislocation evaluation
Evaluation
Acetabular inclination
Acetabular version
Femoral version
Offset / LLD
Soft tissue
Liner wear / loosening
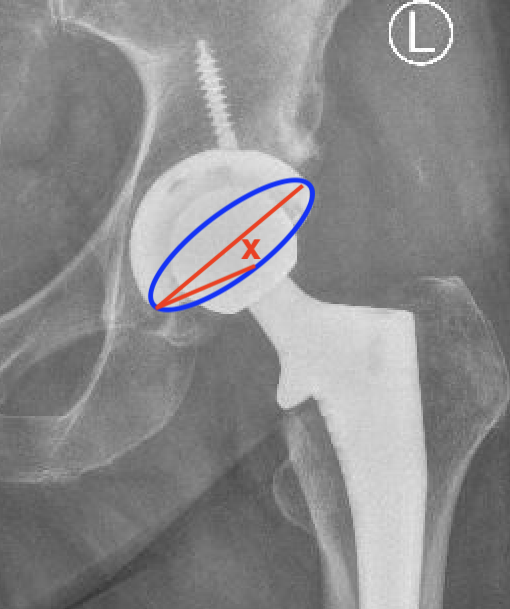
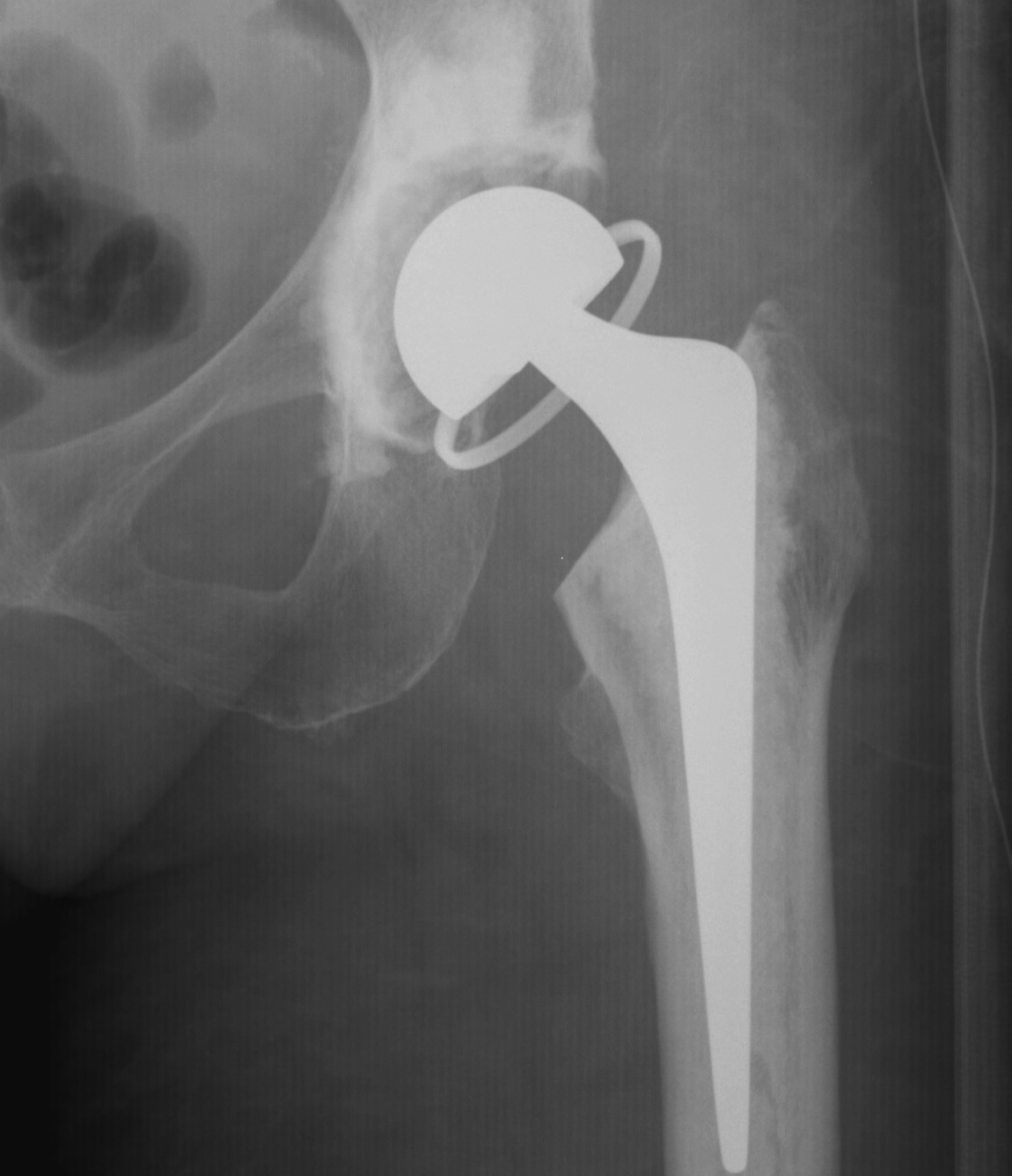
1. Acetabular Inclination
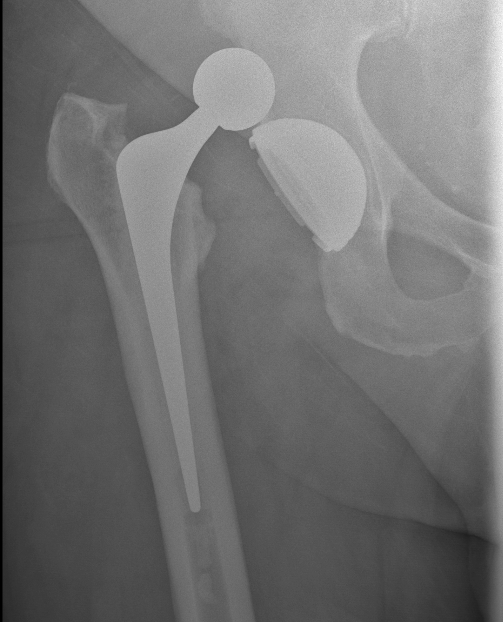
AP Xray
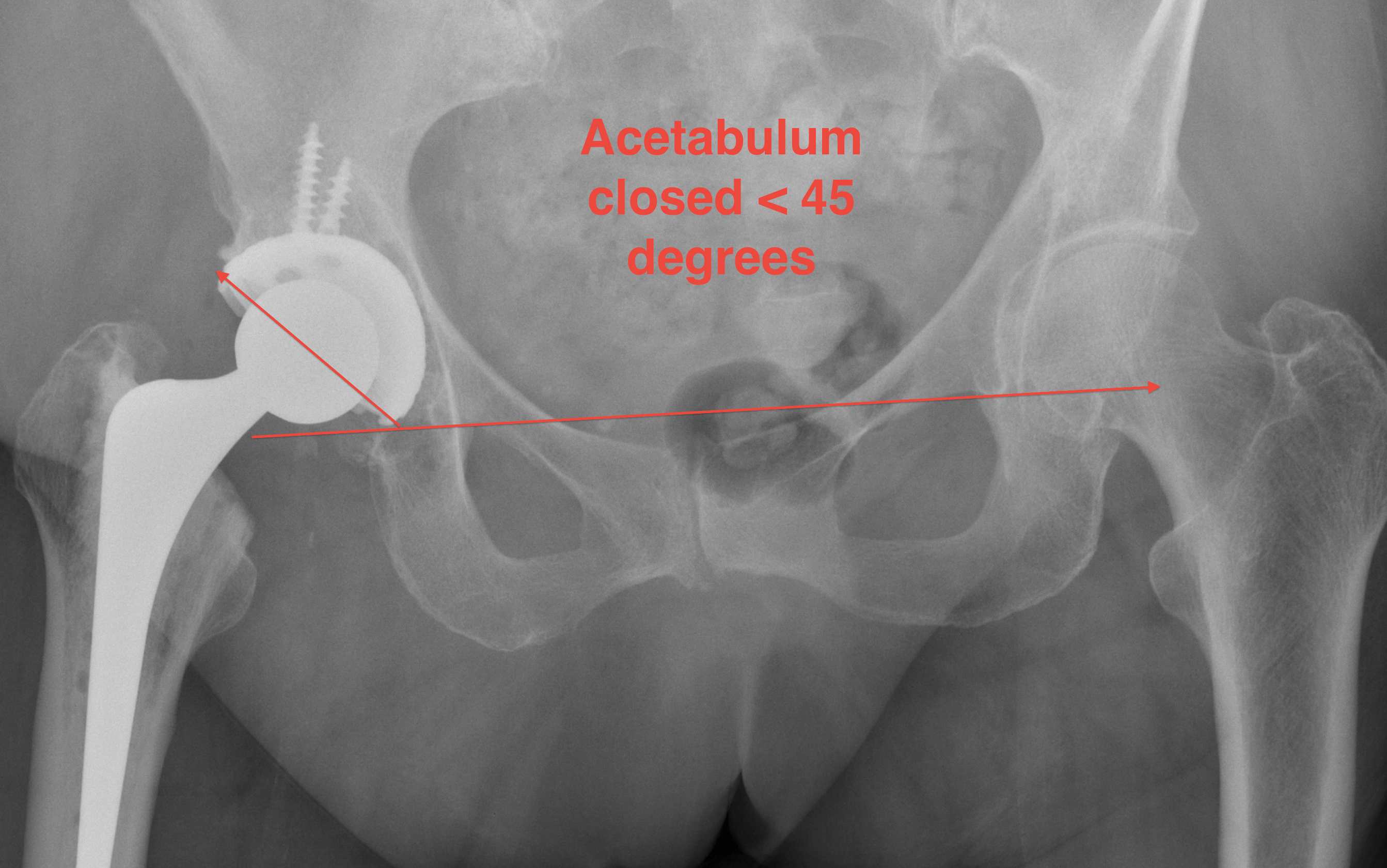
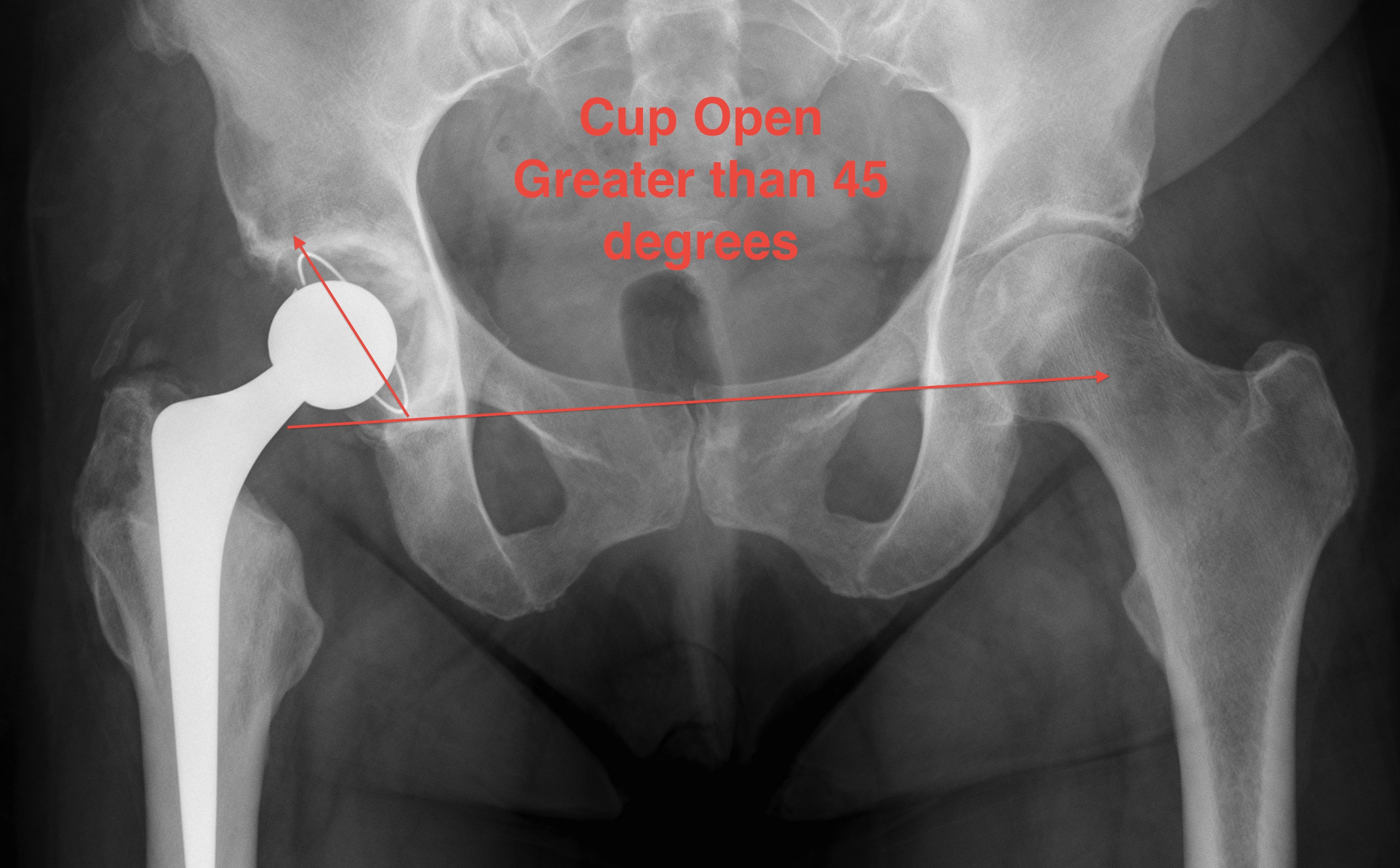

Excessive acetabular inclination
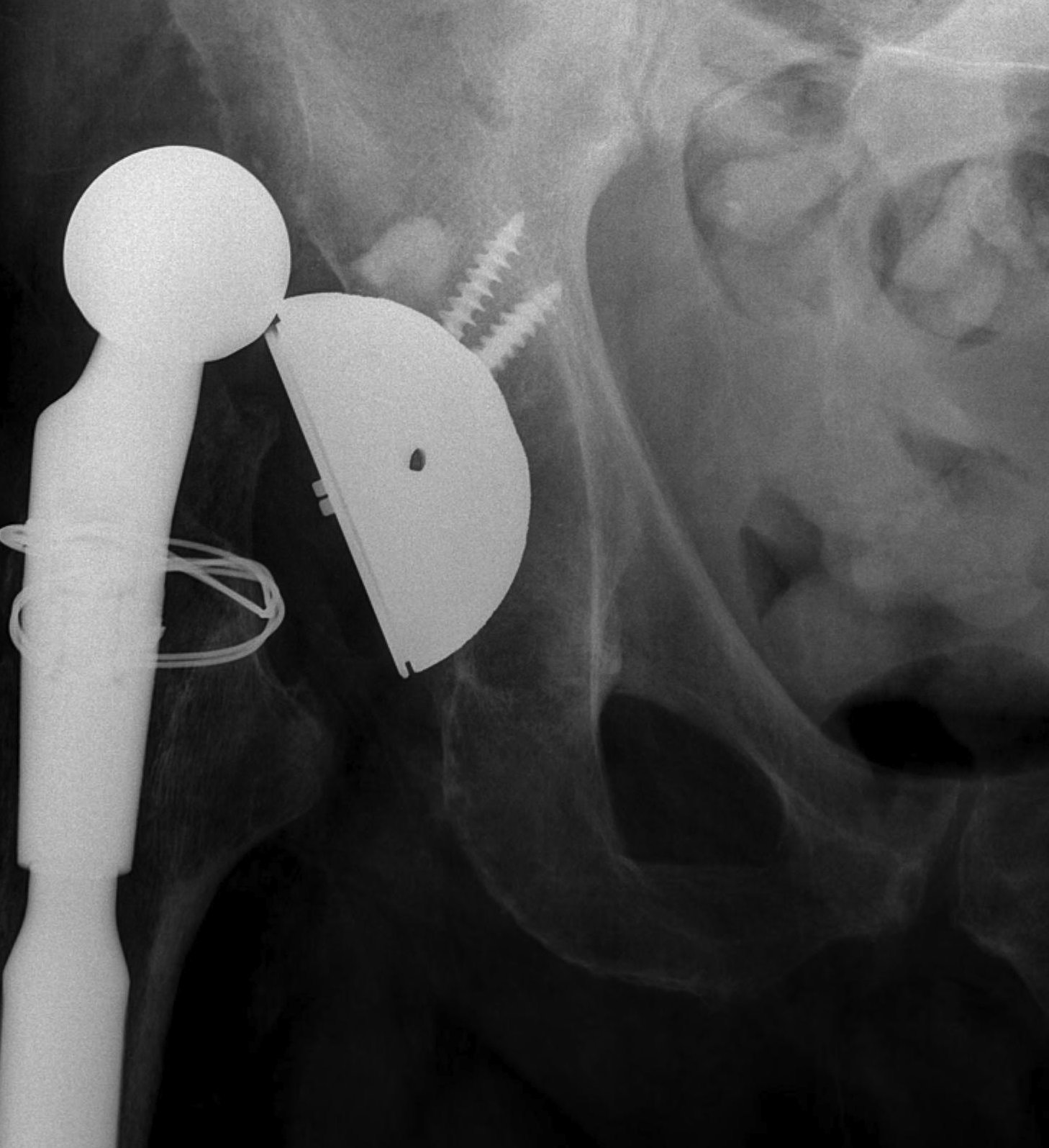
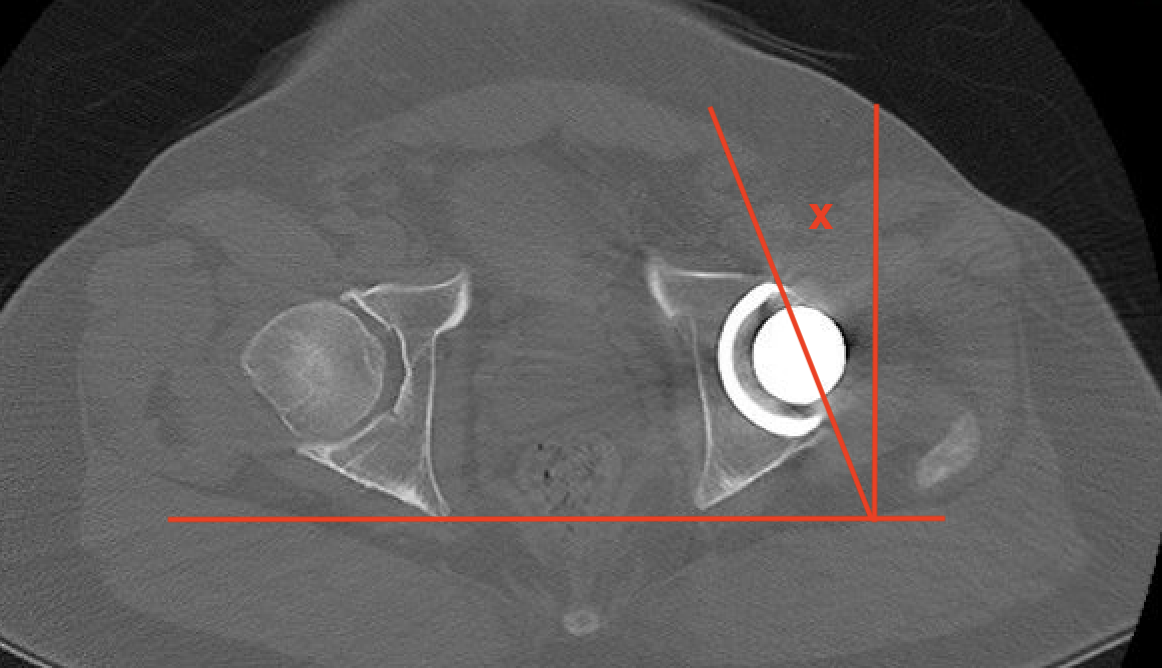
2. Acetabular Version
Xray
Difficult to measure on xray
Methods for measuring cup anteversion on xray PDF

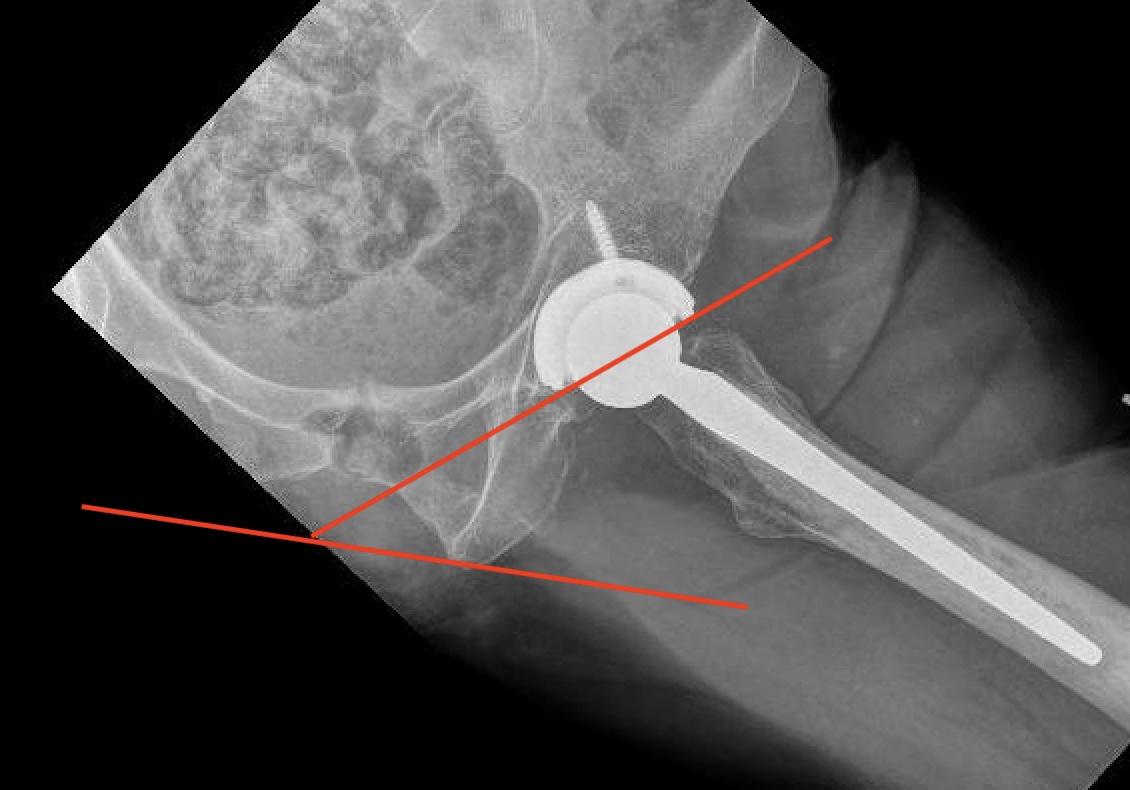
CT scan
Altered by pelvic tilt
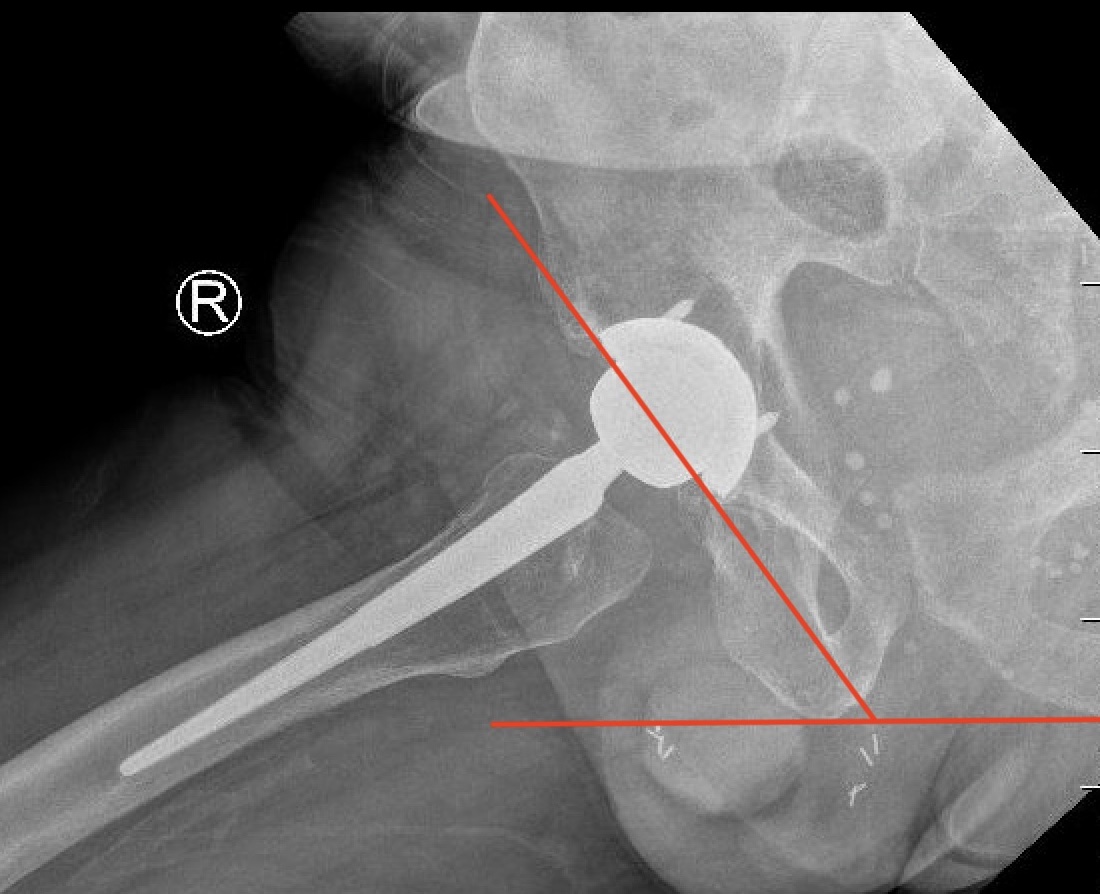
3. Femoral Version
CT scan
- line prosthesis neck
- line posterior femoral condyles
4. Offset
Xray
- difficult to evaluate on xray
- affected by femoral anteversion


5. Soft tissue tension
Increased dislocation with GT fractures
6. Eccentric liner wear

7. Loosening

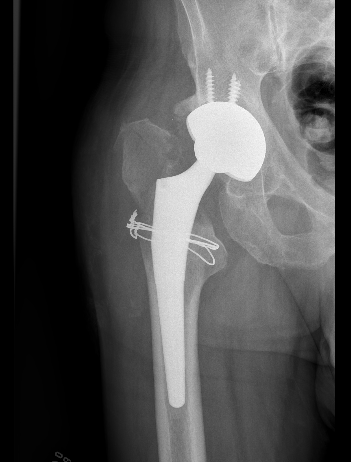
Loose acetabular components
Revision THA for instability
Options
Liner exchange / augmentation liner
Acetabulum revision - reposition
Femoral revision - offset, LLD, anteversion
Constrained liner
Dual mobility
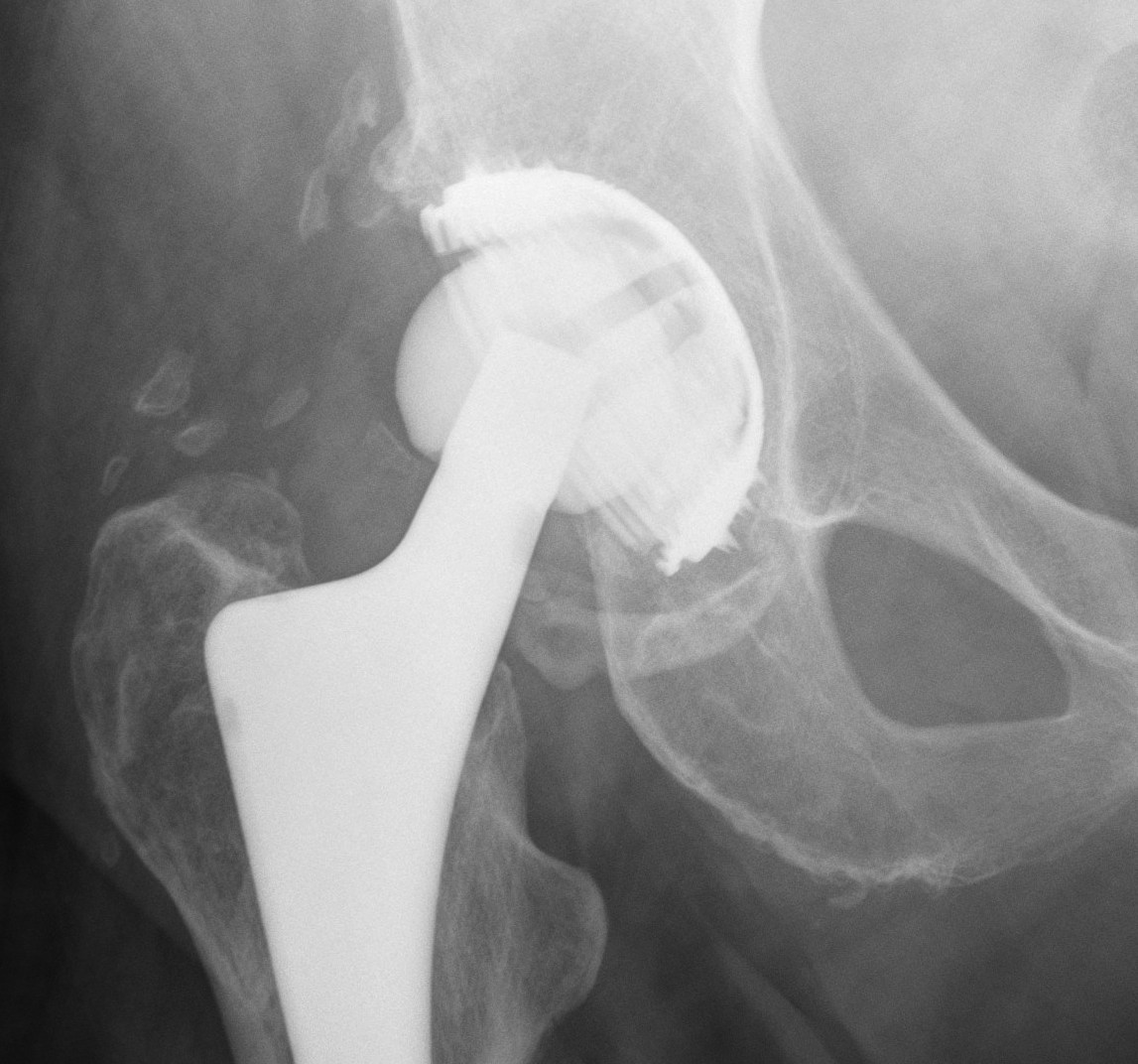
Liner exchange / augmentation
Technique
1. Exchange liner for elevated liner
2. Posterior liner augmentation device - screw onto old liner
Results
McCabe et al Arthroplasty Today 2021
- systematic review of liner exchange for instability in 644 THA
- Liner augments applied
- 10% recurrent dislocation at 4 years
- one specific implant as low as 4% dislocation at 4 years
- 310 posterior augmentation devices for instability
- recurrent dislocation 1.6%
Acetabular Revision
Carter et al J Arthroplasty 2011
- 156 revision THA for dislocation
- acetabular revision v liner exchange v acetabular / femur revision
- 21% failure
- increased failure rate with previous revision / isolated liner exchange / 28 mm heads
Constrained cups


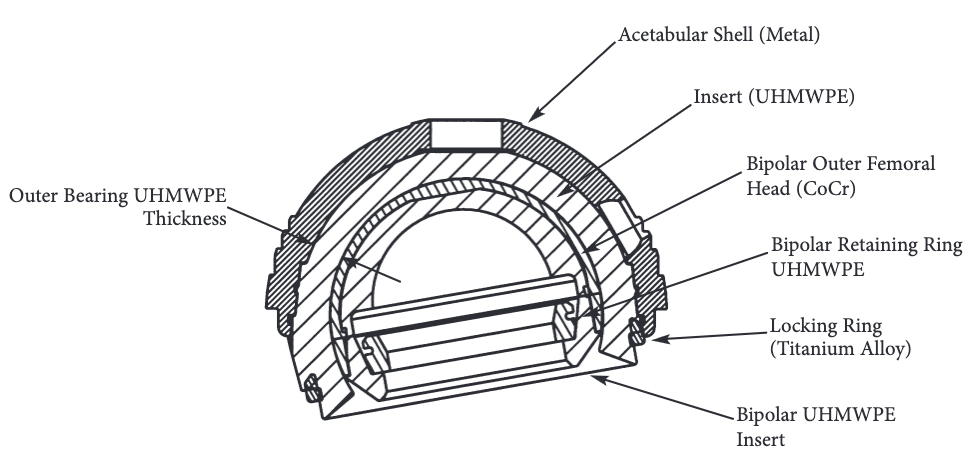
Styker trident constrained liner PDF
Design
- bipolar / tripolar
- metal locking ring
- cemented or uncemented
Indication
- recurrent dislocation / revision
- deficient soft tissues / paralyzed abductors / GT non union
Issues
- can still dislocate
- difficult to reduce if dislocates
- early loosening due to reduced ROM / high strain
Results
Berend et al J Arthroplasty 2005
- 755 constrained liners in revision THA
- dislocation rate 18% overall
- dislocation rate 29% for dislocating hips
- 5 year survival 69%
- 10 year survival 52%
- 389 hips revised with triplanar constrained cup
- 2 year follow up
- 11% failure rate
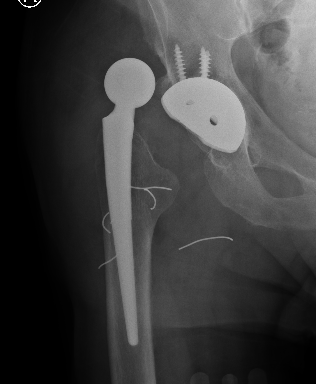
Dislocated constrained liner


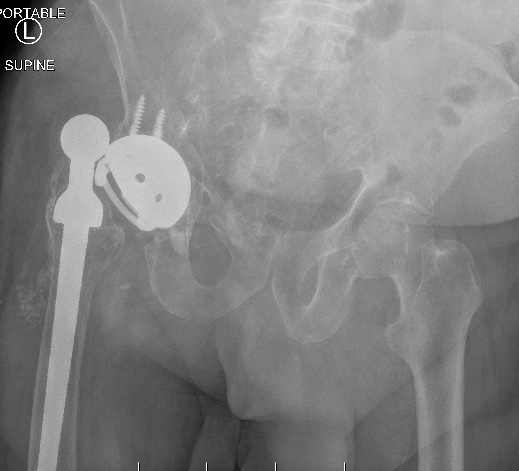
Successful reduction constrained liner


Unsuccessful reduction constrained liner
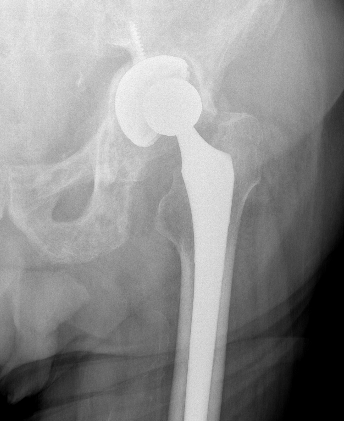
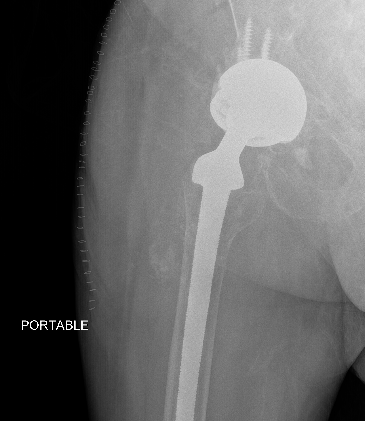
Dual mobility


van Eecke et al Hip Pelvis 2020
- systematic review of constrained and dual mobility in revision THA
- 46 studies and 5,600 hips
- survival: DM 94.7% vs. constrained 81.0%)
- dislocation rates: DM 2.6% vs. constrained 11.0%
- acetabular loosening rates: DM 1.0% vs. constrained 2.0%
