Incidence
1 / 1000 per year female
1.5 / 1000 per year male
Phalangeal fractures
- represent more than half of all hand fractures
Goals of Treatment
Restore normal function of the finger
1. Restoration of bony anatomy
2. Early motion
- inherent fracture stability
- splinting
- adequate internal fixation
- dynamic external fixation
Examination
Obvious swelling / bruising / deformity
Compound injuries
Rotational alignment
1. With active flexion, all fingers point towards scaphoid tuberosity
2. Evidence digital overlap (see below)
3. Plane of nail beds all in same plane
- LF often slightly different rotation


Tendon avulsion
X-rays
3 planes centred on MCPJ middle finger
- AP
- lateral
- oblique
Care to look for subtle evidence joint subluxation
Principles Closed Treatment
POSI (Position of Safe Immobilisation)
- 20o wrist extension
- flexion of MCPJ to 60 - 70o
- IP joints in extension
- thumb in abduction
Acceptable alignment
Pun etal JBJS Am 1989
- 10o angulation in both planes
- no rotation
- 50% overlay
Surgical approaches
A. Midaxial
- dorsal to NV bundle
- make dots on flexion creases with finger flexed
- this marks incision
- approach P1 by excision of one sagittal band
- less tendon disruption
- more difficult visualisation / access
B. Midlateral
- volar to NV bundle
C. Dorsal approach
- direct doral incision
- divide extensor hood over P1
- between lateral bands P2
- repair extensor mechanism at end
- risks scarring down of extensor tendon to implant
Types of injuries
1. Extra-articular fractures
A. Distal phalanx tuft fractures
B. Shaft fractures of the distal, middle and proximal phalanges
2. Joint injuries
DIPJ
- dislocations
- mallet
- Pilon fractures
- Flexor tendon avulsion
PIPJ
- dorsal dislocations
- dorsal fracture dislocations
- volar dislocations
- Pilon fractures
- Condylar fractures
MCPJ dislocations
Tuft fractures
Most common hand injury
- usually crush mechanism
Management
- trephination of subungal haematoma (relieves pain)
- repair nail bed disruption
- irrigation and washout of open injuries
Distal phalangeal shaft fractures

Non displaced fractures
– splint DIPJ for 2-3 weeks
Displaced
- higher energy fractures
- washout open wounds
- repair nail bed
- bony reduction with percutaneous K wire
- distal phalanx just under nail bed
Shaft fractures middle / proximal phalanges
Undisplaced
- usually stable
- buddy strap 3-4 weeks

Displaced


Unstable fractures
- oblique, spiral, comminuted fractures
Transverse fractures P1 / characteristic deformity
- insertion of intrinsics at base PP flex fragment
- insertion of central slip to MP extend fragment

Fractures of P2 distal to insertion FDS / characteristic deformity
- FDS will flex fragment
- extensor tendon will extend fragment
Closed reduction
- relaxation of intrinsics
- axial traction
- reduction of deformity / POSI
ORIF
A. Transverse fractures
- cross K wire
- Lister’s intra-osseous wire fixation
- plating


B. Long oblique / spiral fractures
Definition
- fracture must be at lease 2 x diameter bone
- can treat with 2 x lag screws
- one perpedicular to fracture to lag
- one perpendicular to shaft to resist shear
Options
- percutaneous K wires / screw fixation / plating

DIPJ Dislocations
Dorsal
- most common
- closed reduction with dorsal traction
- failed closed reduction – volar plate, FDP
- 60% injuries open
- splint joint in flexion 2- 3/52 weeks
- ROM at 1/52
Volar
- rare
- failed closed reduction – extensor tendon
- DIPJ extension splint 6-8/52
Mallet fractures


Mechanism
- axial load
- extensor tendon attached to bony fragment
Closed treatment
- mallet splint (Stack)
- expect 10o extensor lag with mild loss ROM
- good results with non – op management


ORIF
Indication
- volar subluxation of distal phalanx
- fragment > 50% joint surface
- chronic > 12 weeks old
Open treatment
- high incidence of complications
- percutaneous K wire recommended
Technique
1. Reduce and axial K wire
2. Dorsal blocking K wire / axial K wire
Wehbe and Schneider JBJS Am 1984
- 21 patients with intra-articular fractures
- 15 treated non operatively
- 6 treated operatively
- nil improvement in outcome
- worsened surgical morbidity
Pilon fractures base distal phalanx
Impaction injuries
Management
- ORIF very difficult
- all attempts at closed reduction +/- percutaneous pinning should be made
- fallback of arthrodesis / arthroplasty
FDP avulsions
Leddy and Packer classification
I Vinculae are ruptured, tendon retracts to palm
II Vinculae intact, tendon remains at PIPJ
III Large bony fragment, ensnared beyond A4 pulley
Type 1
- must be operated within 10 days to avoid contractures
- otherwise 2 stage reconstruction
Type 2 / 3
- can operate within 6 weeks
- ORIF large fragments
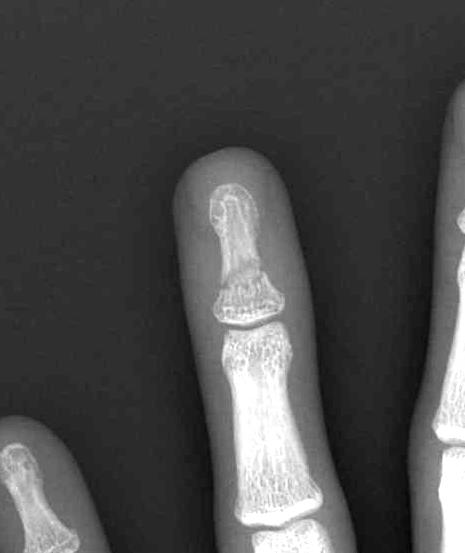
Condylar fractures of head of P1 / P2
Mechanism
- torsional and valgus impaction
London classification
Type 1 Unicondylar, undisplaced
Type 2 Unicondylar, displaced
Type 3 Bicondylar
Displaced unicondylar
- percutaneous K wire
- ORIF with screw
![]()
![]()
Open reduction
- P1 – between central slip and lateral band
- P2 – lateral to terminal extensor tendon
- must preserve collateral ligament which supplies blood
Type III bicondylar fractures
- difficult fractures
- 90 degree condylar plate
- lag screw and plate
- high risk of joint stiffness
MCPJ Destruction
Cause
- infection
- trauma
Options
- joint replacement
- fusion




