Acute management
Resuscitation
EMST
Neurovascular assessment
Investigations - exclude Pipkin, NOF
Emergent reduction / skeletal stabilisation
Assess stability
Re-evaluate sciatic nerve
Insertion Femoral Steinman Pin
Indications
- displaced acetabular fracture

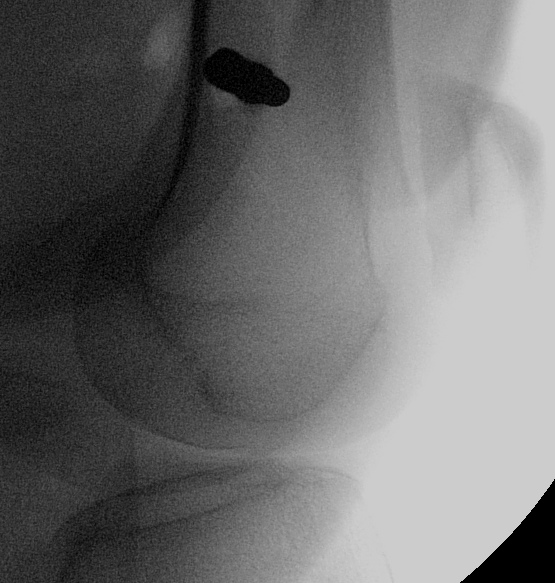
Technique
- above blummenstaat's line
- in metaphyseal bone
- minimum 10 pounds weight, may need more
- assess post operative reduction

Goals of Management
1. Restore Articular Congruency
2. Reduce & Maintain Hip in Acetabulum
Non operative Management
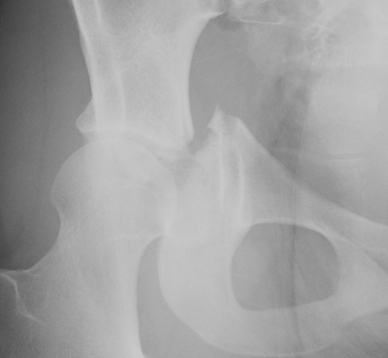
Radiographic factors
1. Articular step < 2mm
2. Weight bearing roof intact
- Matta Roof > 45o
- CT subchondral roof 10 mm
3. Congruent reduction
4. Stable < 40% posterior wall fracture
Results
Tornetta JBJS Br 1999
- 38 hips with above criteria for 2.7 years
- good or excellent outcome in 91%
- poor outcome related to other injuries
Patient factors
Elderly
Osteoporotic bone
Pre-existing arthritis
The elderly patient can have a THR as salvage if required down the track
Operative Management
Indications
1. Incongruent reduction
2. Non intact weight bearing dome
3. Articular step > 2mm
4. Retained fragment
5. > 40% posterior wall or instability
Surgical factors
1. Surgeon experience
- steep learning curve
Letournel & Judet Fractures of the Acetabulum 1993
- initial rate non anatomical reduction 32%
- 4 years later 10%
2. Surgical timing
Letournel & Judet
- anatomical reduction in only 50% operated after 21 days
- if operate too early, bleeding +++
3. Fracture complexity
Matta JBJS Am 1996
- 262 patients
- 96% elemental fractures anatomically reduced
- 64% complex
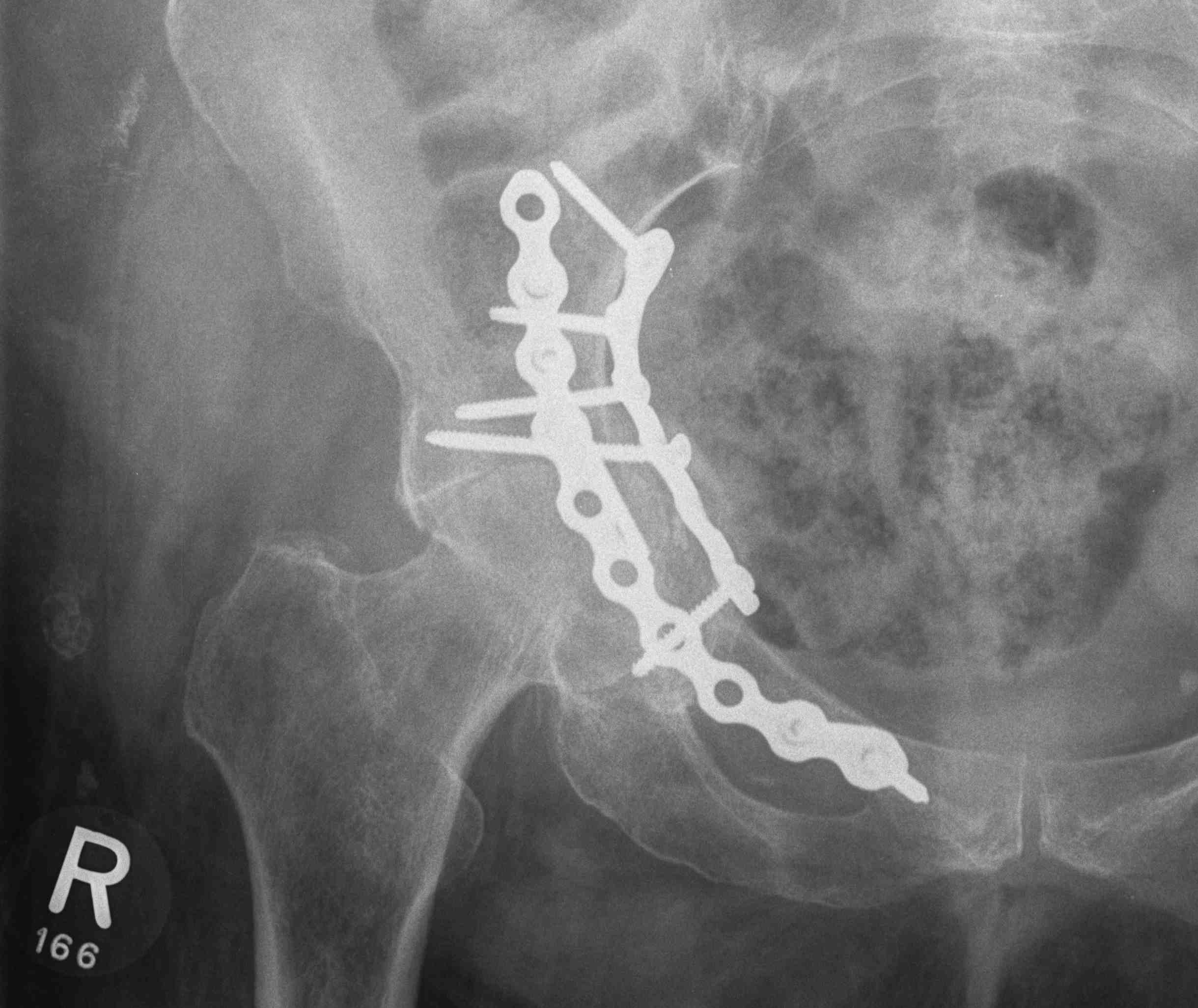
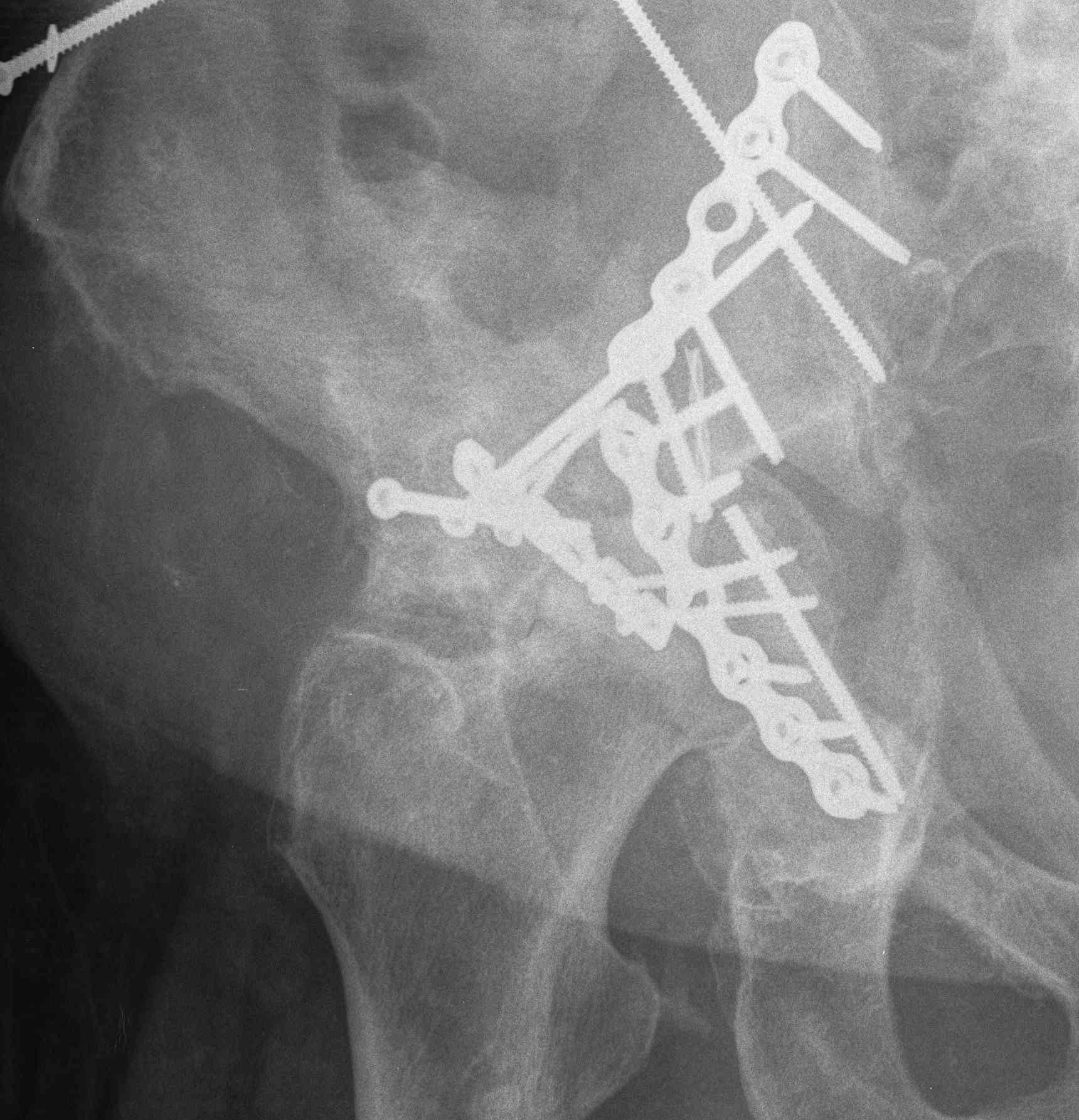
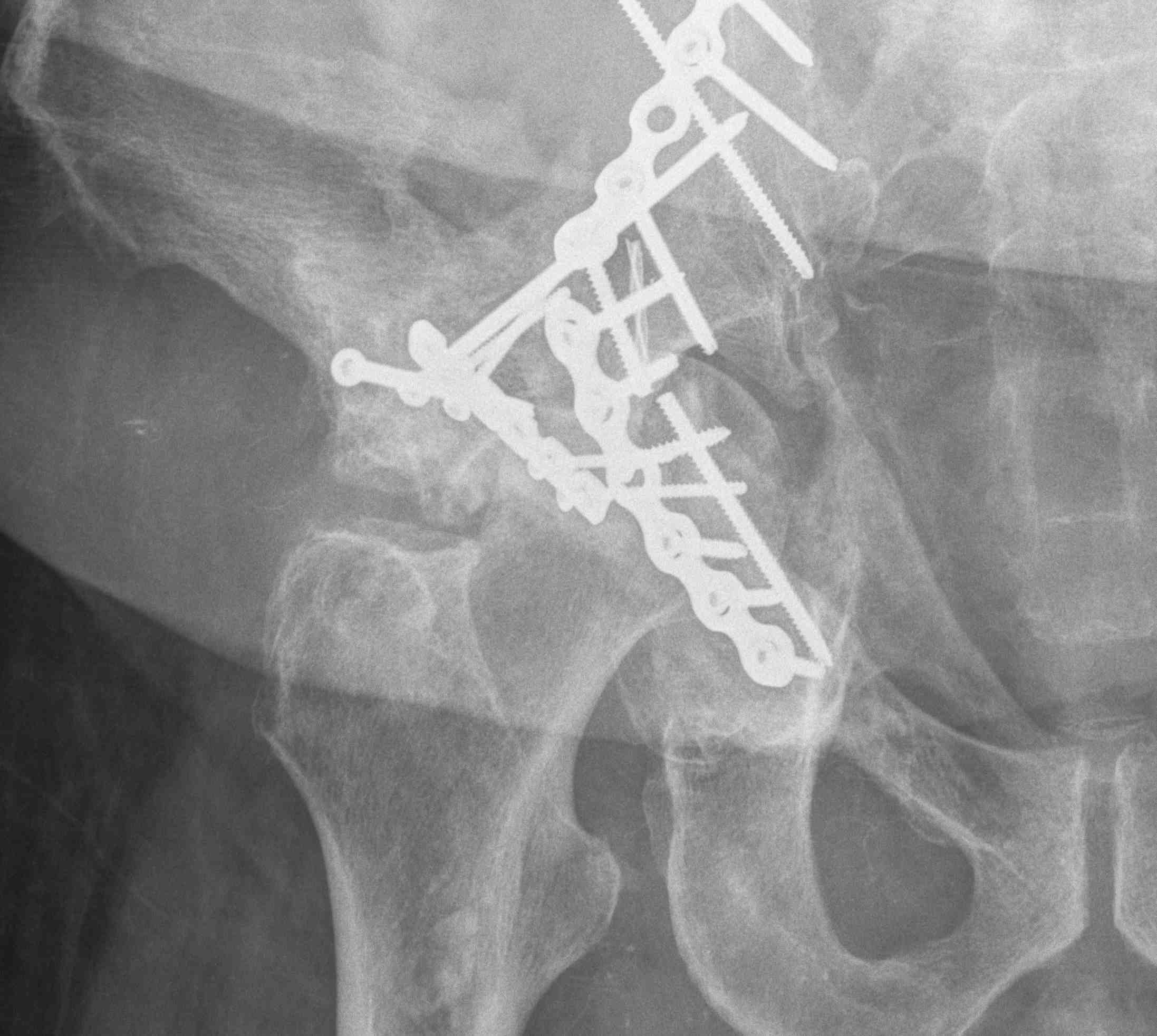
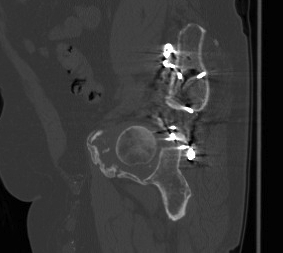
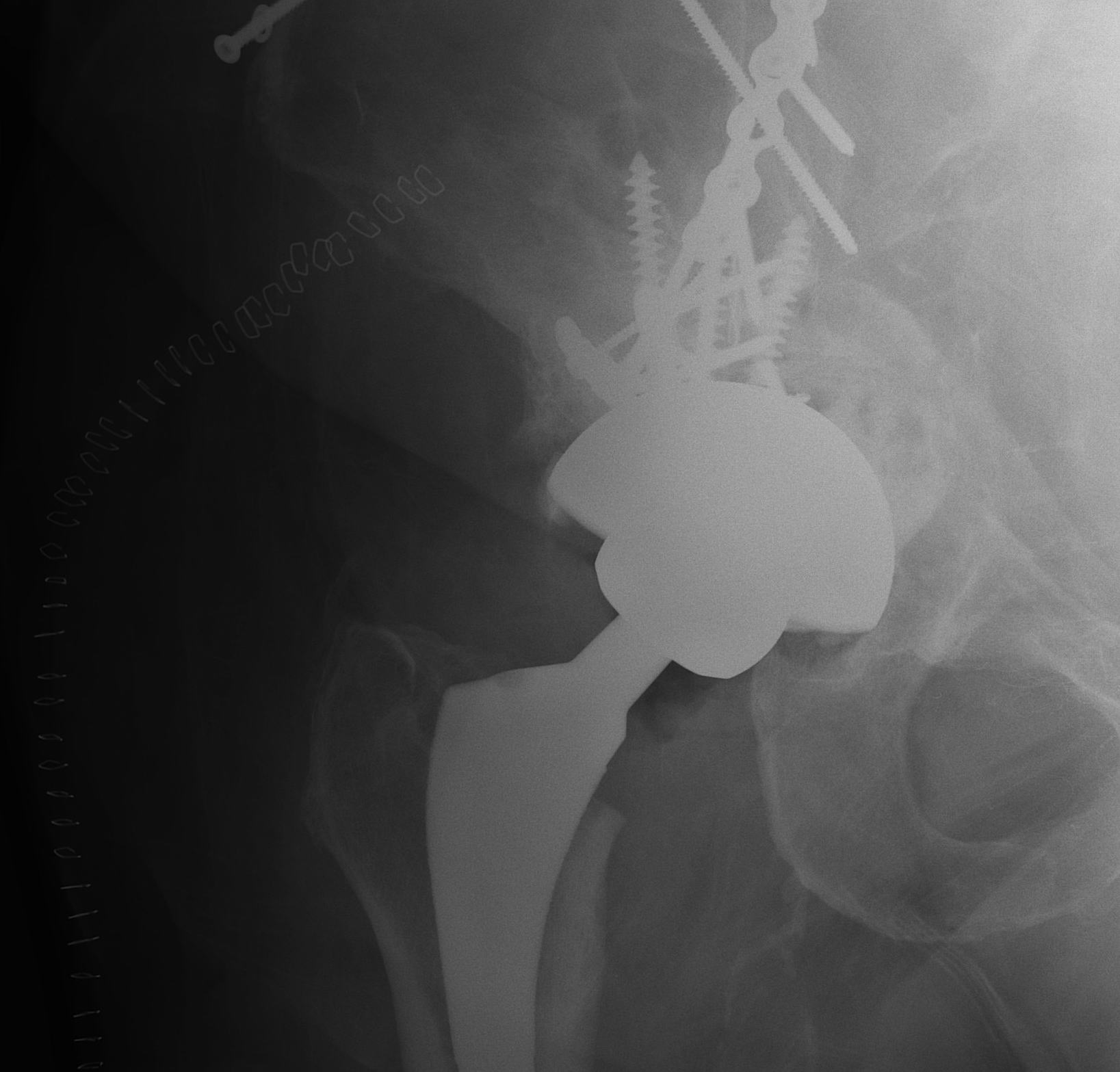
ORIF
Aim
1. Anatomic reduction
2. Provisional fixation with lag screws
3. Buttressing with curved reconstruction plates
Options
1. Posterior / Kocher-Langenbeck approach
- posterior column / wall
2. Ilioinguinal approach
- anterior column / wall
3. Extended iliofemoral approach
- Smith-Petersen extended over iliac crest
- for transverse / both column fractures
4. Triradiate approach
- Kocher-Langenbeck with anterior extension from GT to ASIS
- wide exposure for both column fractures
- high incidence HO
Preferred option is to perform
- ilioinguinal for anterior column / wall
- posterior / Kocher Langenbeck for posterior column / wall
- do both 1 week apart for combined fractures
Techniques
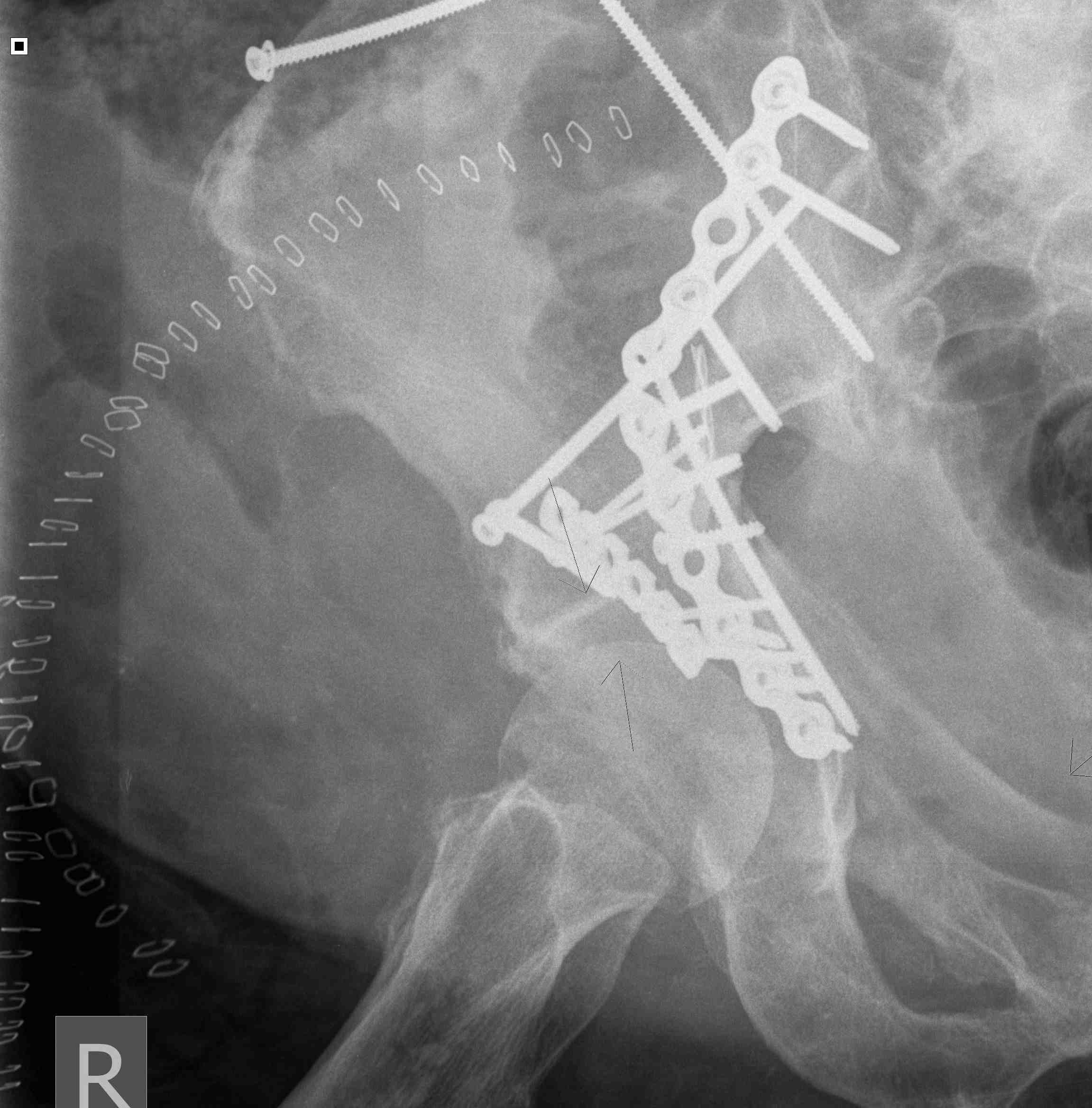
Posterior Column & Wall Fracture



Position
- IDC, radiolucent table, IV Abx
- lateral position but patient rolled excessively over
- patient 45o up from table, exposes posterior
- top leg hip flexed, knee flexed
- bottom leg extended
- blankets under top leg
- lateral support in front of top knee to prevent too much hip flexion
- prevents excessive tension on sciatic nerve
Standard posterior approach
- divide fascia lata
- find and protect sciatic nerve at all times
- do so by keeping hip extended and knee flexed
- expose short external rotators, divide 1cm from insertion to preserve blood supply
- usually must divide some of G. max
- elevate G medius from ilium
- steinmann pin in ilium for exposure
- expose ischial tuberosity by elevating biceps femoris, again protecting sciatic nerve at all time
- steinmann pin in ischium
Reduction can be aided but applying femoral distracter
- between ilial and ischial pins
Expose fracture
- posterior wall fracture, elevate and clean callous
- capsule usually partially avulsed
- ensure no femoral head fractures or loose fragments
- posterior column fracture often up in ilium, can put a plate across it
Reduction
- often indirect
- buttress plate from Ischial Tuberosity to Ilium
- contour or use pre-contoured
- screws at plate extremities
- often 2 parallel plates if wall and column fracture
II to ensure screws not in acetabulum
Anterior Column & Wall Fracture

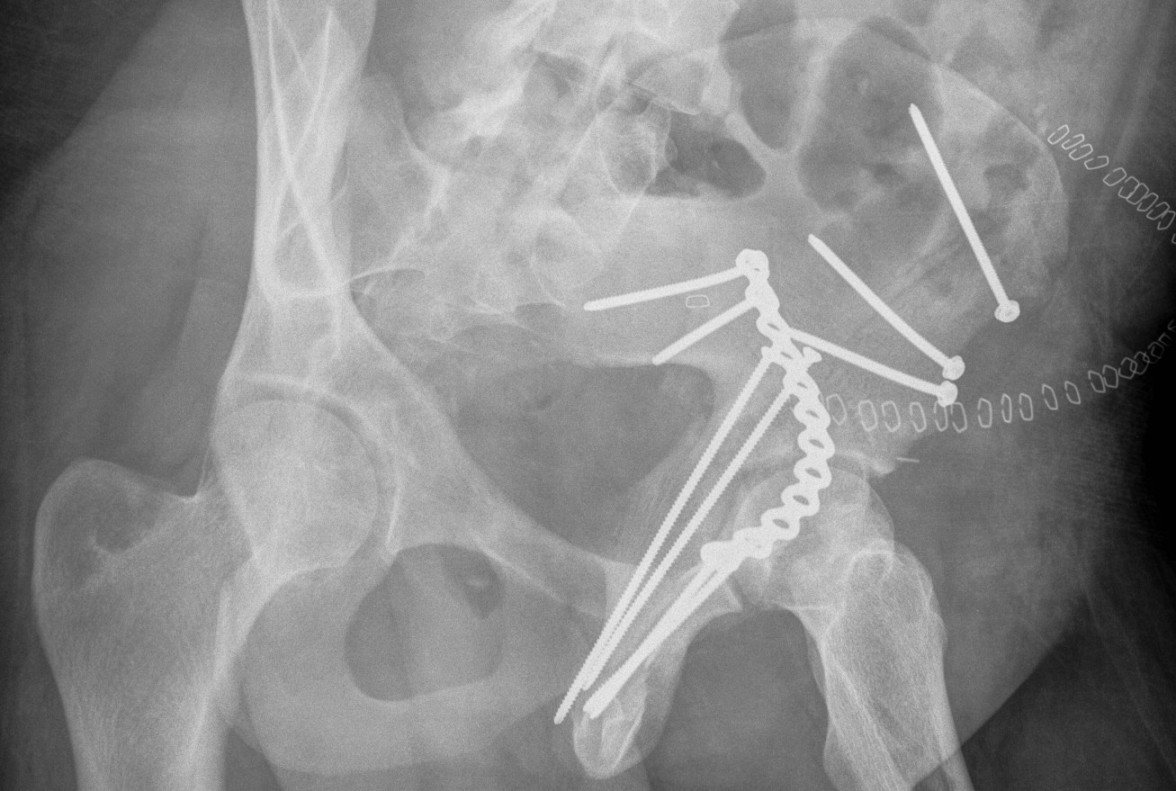

Position
- radiolucent table
- IDC to decompress bladder
- IV Abx
- sandbag under operative side for some elevation
- need to prep and drape pelvis so can virtually access both ASIS
- often need to get across pubis
Ilioinguinal approach
Curvilinear incision from above pubis to ASIS
- identify and protect LFCN / below ASIS
- divide external oblique 1 cm above inguinal ligament
- identify and protect spermatic cord / round ligament
- divide posterior wall / internal oblique and transversus
3 windows (medial / middle / lateral)
- find external iliac artery and vein with peanuts / place sling
- find psoas and femoral nerve / place sling
- find iliopectineal fascia between vessels and psoas and divide with scissors
Medial window medial to vessels
- superior pubic rami
- may have to release some of rectus
Beware corona mortis
- anomolous vascular connection
- 10 - 15% patients
- between external iliac / epigastric artery
- to obturator artery
Middle window between psoas and vessels
- exposes quadrilateral plate
Lateral window lateral to psoas
- elevate iliacus off crest to expose fracture in iliac wing
- exposes around to SIJ
ORIF
1. Reduce quadrilateral plate
- small T plate / will sit under pelvic reconstruction plate
- separate recon plate
2. Plate iliac crest fracture
- long 13 hole plate from pubis
- along superior pubic ramus up onto inner table of ilium
- indirect acetabular reduction
Results
Judet and Letournel 1980 417 Fractures
- 73% perfect reduction with 84% very good results
- imperfect reduction 55% good results
- infection 5.6% / heterotopic bone 18%
- poor results related to > 3 weeks
Matta 1996 258 Fractures
- anatomical reduction 71% with 76% excellent to good results
- poor results related to injuries to femoral head / age / post-operative complications
- AVN 3%
Complications
Heterotopic Ossification
- ilioinguinal 1%
- Kocher-Langenbeck 7%
- extended Iliofemoral 12%
Failure of fixation
Very problematic
- often need revision to THR
- pelvic discontinuity must be addressed

DVT
- rate very high
- prevent with mechanical and chemical prophylaxis
Sciatic nerve injury 2%
- especially with posterior approach
AVN 2%
- higher with posterior dislocations and Pipkin fractures
Infections
- occur in 2-5%
- increased in the presence of Morel-Lavallee lesion
Arthritis
- the most common complication
- anatomic reduction - 10%, usually after 10 years
- imperfect reduction - 45%, usually before 10 years 2,6


Bladder and spermatic cord injury
Hernia formation
Vascular injury
External iliac vein
- control distally with vessiloop
- suture with 5.0 / 6.0 prolene on noncutting needle


