

Characteristics
Atypical femoral fractures (AFFs)
- femoral stress fractures
- transverse
- begin laterally
- associated with lateral thickening initially
- caused by minimal or no trauma
Risk factors / associations
1. Medications
- prolonged suppression of bone remodelling by medications
- > 5 years bisphosphonates
- Autoimmune disease and long standing glucocorticoid use
- Denosumab / Romosozumab for osteoporosis
2. Lower limb alignment
- associated with bilateral AFFs
- head neck varus
- lateral femoral bowing
- 13 cases of AFFs in Asian women
- 12/13 had significant lateral femoral bowing
- 7/13 on bisphosphonates
- only 3/13 had taken bisphosphonates for > 5 years
Site
Subtrochanteric most common
Lateral femoral shaft less common
Shane et al J Bone Miner Res 2014
- bilateral 28%
- mandatory careful inspection of contralateral femur
Bisphosphonates
- reduction of hip fracture risk v risk of atypical femur fracture
- 10 year period
- 196,000 women over 50 years old - 277 atypical femur fractures
- increased risk in Asian race
- Caucasian women over 3 years: prevented 149 hip fractures and caused 2 atypical femur fractures
- Asian women over 3 years: prevented 91 hip fractures and caused 8 atypical femur fractures
Dell et al Osteoporosis International 2018
- recommendations for drug holidays
- consider femur DEXA scan or other imaging every 3 - 5 years
- look for any focal or generalised lateral femoral cortical changes
Clinical
History of thigh pain
Xray
Periosteal stress reactions / beaking
Thickening of the lateral cortex
- tension side
- most common in the subtrochanteric region
- can be in shaft
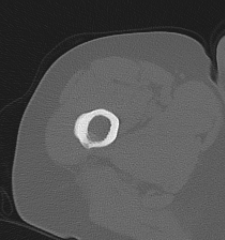
CT / MRI should be performed to exclude incomplete fracture
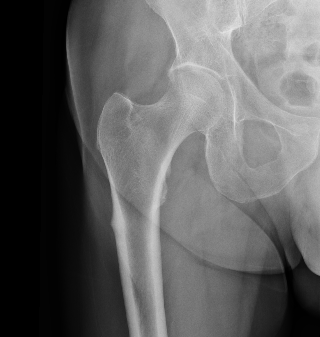

Lateral beaking subtrochanteric region

Lateral beaking femoral shaft
Fractures
Transverse fractures
- begin laterally
- minimal comminution
- incomplete versus complete


Incomplete subtrochanteric AFF

Incomplete femoral shaft AFF / dreaded black line


Complete AFF
Diagnosis
2013 ASBMR task force criteria of atypical femoral fractures
| Major Criteria | Minor Criteria |
|---|---|
|
Minimal or no trauma - fall from standing height or less |
Generalized cortical thickening |
|
Fracture is transverse and originates from lateral cortex - incomplete fractures lateral cortex only - complete fractures may have medial spike |
Prodromal symptoms such as groin or thigh pain |
| Minimal comminution | Delayed fracture healing |
| Localised periosteal thicking or beaking at lateral cortex |
Management
Nonoperative
Natural history
Png et al Osteoporosis Int 2019
- non operative treatment
- lateral thickening: 21/115 (18%) progressed to incomplete fracture
- incomplete fracture (black line): 14/35 (40%) progressed to complete fracture
Medical
Cease bisphosphonates
Calcium and Vitamin D
Salamah et al Arch Orthop Trauma Surg 2024
- systematic review of use of Teriparatide (recombinant PTH) for AFFs
- improved healing times and union rates
Surgery
Indications
Complete fracture
Incomplete fracture / lateral thickening
- high risk
- continued need for steroids
- bowing / varus necks
- significant femur / groin pain
- radiographic progression
- failure to improve with nonoperative care
Options
1. Cephalomedullary nail
- be careful of bowed femurs in Asian women
2. Lateral plate and screws
- high failure rate
- consider in setting of severe bowing






Results
- systematic review of 77 studies and 834 AFFs
- incomplete fractures: nonoperative treatment failed 47%
- incomplete fractures: surgery achieved union in 97%
- complete fractures: IMN nonunion rate 12.9%
- complete fractures: plate fixation nonunion rate 31%
- must discontinue bisphonates
- mean time to union 7 months post surgery
Compression Stress Fractures
Medial femur
Rare
- associated with osteomalacia
- compression side
- incomplete can heal
- nail complete


