Epidemiology
Young men
Aetiology
FOOSH
- axial load, dorsiflexion and radial deviation
DISI occurs in ulna deviation
Herbert Classification
Type A Stable acute fracture
A1 Tubercle

A2 Incomplete waist fracture


Type B Unstable acute fracture
B1 Distal oblique fracture
B2 Complete waist fracture

B3 Proximal pole fracture

B4 Trans-scaphoid perilunate fracture
Type C Delayed Union
Type D Established Non-union
D1 Fibrous Union (stable)
D2 Pseudarthrosis (unstable / early deformity)
D3 Sclerotic Pseudoarthrosis (Late deformity)
D4 Avascular Necrosis (fragmented proximal pole)
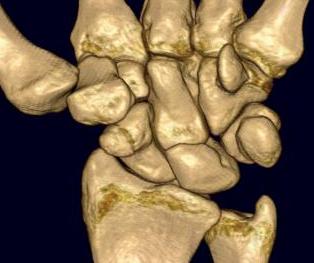
Anatomy
Scaphoid is Greek for boat
- shaped more like a twisted peanut

Majority is articular
- except for dorsal ridge
- this is the site of entry of majority of blood supply
Vascularity
Gelberman & Menon J Hand Surg 1980
- latex injection
2 major vascular leashes
1. Dorsal ridge artery
- branch of radial artery
- major blood supply
- 70- 80% scaphoid including proximal pole
- enters through the non articular dorsal ridge
2. Distal tubercle
- palmar & superficial palmar branches of radial artery
- perfuse distal 20% to 30% of scaphoid
Fracture Location
Waist 65%
Proximal third 25%
Distal third 10%
Complications
1. Non union
Undisplaced
- union > 95%
- rare with immediate immobilisation
Displaced
- non union 50%
2. AVN
- increases the more distal the fracture (50% proximal pole)
- increases with displacement (AVN 50%)
3. Malunion and DISI
- associated with increased intra-scaphoid angle
Clinical Features
Tender anatomical snuffbox
Swelling
Reduced ROM
X-ray
5 images will pick up 99% of fractures
- PA
- Lateral
- PA in 45° oblique pronation
- PA 45o oblique supination
- PA in ulna deviation




Increased intra-scaphoid angle / humpback deformity
- > 35o abnormal
- > 45o associated with poor outcome i.e. DISI
- also demonstrated to lead to loss of extension
2 week delay
Issue
- tender in ASB
- no sign of fracture on initial x-ray
- usual treatment is to place in cast and xray in 2 weeks
- can be delayed appearance of scaphoid fracture
Leslie and Dixon JBJS 1981
- 222 fractures
- 98% seen at time of presentation
- 2% became evident over ensuing weeks
- these were only incomplete and located on concave side of scaphoid
Excluding scaphoid fracture
- CT - easy to obtain, inexpensive
- MRI - highly sensitive, but expensive and difficult to obtain
Instability
1. Displacement > 1mm on any film
2. Intra-scaphoid > 35o
3. Proximal pole fracture
4. Comminution
5. SL > 60o
6. Radio-lunate angle > 15o
7. Perilunate trans-scaphoid dislocation
Can be very difficult to assess displacement on plain films
- suggest use of CT
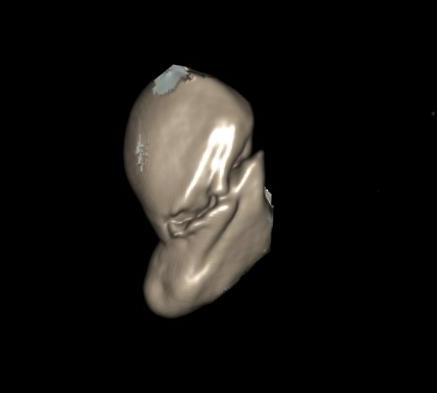
CT
1mm slices in sagittal plane of scaphoid
- plane of metacarpal
Position
- patient prone
- hand over head
- fully pronated


Bone Scan
Highly sensitive
- 5% to 15% incidence of false positives
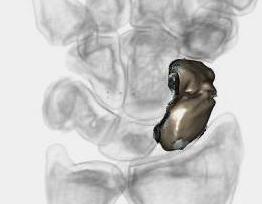
MRI
Very sensitive for occult fracture
Identifies AVN
Identifies carpal instability
Management
Non operative Management
1. Anatomical Snuff Box Tenderness / Normal Xray
Options
1. POP 2/52, rexray out of plaster
2. MRI / CT
2. Acute undisplaced stable
Types
- displaced < 1mm
- incomplete fracture
- tuberosity fracture
Scaphoid cast
- short arm thumb spica cast
- long arm cast not necessary
- some evidence that thumb spica not necessary
Time in cast
- distal / tuberosity 6/52
- middle 1/3 8/52
- proximal 1/3 10/52
Management
- x-ray at 2/52 to ensure no displacement
- x-ray out of cast for union
- see at 6/12 for final xray check union
Non-union
- union rate 90 - 95%
Operative Management
Indications for Surgery
A. Instability
- displaced > 1mm
- intra-scaphoid > 35o
- complex instability / perilunate instability
B. Proximal pole
- high risk of AVN
- 30% rate non union if non displaced
- all theoretically unstable
- could suggest that all need ORIF
- require dorsal approach
C. Athlete / Manual worker with undisplaced
- percutaneous fixation
- early mobilisation and return to work
D. Delayed diagnosis
- may have increased non union rates
2. ORIF
Indications
- displaced fractures
- proximal pole
Approach
1. Volar approach
- workhorse for waist fractures
- preserves dorsal blood supply
2. Dorsal approach
- for proximal 1/3 fractures

Volar approach technique



Position
- supine on arm table
- lead hand
- tourniquet
Approach
- volar along FCR
- deviate along thenar edge to STT joint
- elevate thenar muscles
- FCR ulna, deep branch radial artery radially with APL
- divide superficial branch radial artery
- open capsule in line with FCR
- transverse opening at STT
- will divide RSC ligament
Clean and reduce fracture
- K wires as joysticks
Cannulated headless compression screw
- central third
- more bone contact, longer screws
- increased stability and therefore union rates
- can remove volar beak of trapezium
- pass cannulated screw wire, measure length
- drive wire into distal radius for stability
- pass screw, bury head
Bone graft as required
- very comminuted fracture / unstable
- humpback deformity
- distal radius if small
- iliac crest if large
Closure
- close capsule and repair RSC
Post op
- 8/52 in thumb spica
- assess union
Dorsal approach technique

3/4 Approach
- midline incision on RC joint
- open EPL, reflect radially
- sharply elevate EDC, reflect ulnarly
- open capsule over SL joint
Flex wrist
Insert K wire
- proximal fragment into distal fragment
- entry point is just radial to SL ligament
- drive into trapezium
- check position on multiple views
Insert screw
Results
Herbert ORIF all type B fractures
- B1 90% union (oblique)
- B2 88% union (waist)
- B3 85% union (proximal pole)
Percutaneous fixation
Advantages
- faster union rates than cast
- union approaching 100%
- less time in cast
- earlier return to work
Indications
- minimally displaced fracture in acceptable position
- manual workers / athletes
- anyone who wants to limit time in POP
Technique
Set up
- supine, tourniquet / arm table / II
Traction on thumb
- ulna deviation
- flex wrist over roll of drapes
- II shows long axis of scaphoid
Volar stab incision
- over scaphoid tuberosity
- slightly distal
- insert K wire in long axis / central third scaphoid
Check wire position
- AP / lateral / 45o obliques
- drill
- can put K wire into distal radius for stability / second K wire
Insert cannulated screw
- slightly shorter screw to obtain compression
- usually 24 mm
Post op
- POP 2 weeks
- then allow to range out of plaster
- no manual labour / heavy lifting
- check for union at 6/52