Clinical
Pain & Stiffness
- often more pain than FT tears
Bursal side tears more painful than articular
Articular side more common
May see in young patient overhead throwing
Examination
Painful arc
Impingement signs
No weakness
- function good
- cable system intact
Classification
Articular sided more common than bursal
Ellman
- A (articular)
- B (Bursal)
Grade 1 < 3mm
Grade 2 < 3-6 mm
Grade 3 < 6 mm footprint exposed
Incidence
Sher et al JBJS Am 1995
- 19 - 39 years - 4% PT , no FT
- > 60 years - 26% PT, 28% FT
NHx
Yamanaka et al Clin Orthop 1994
- 40 patients with articular sided PT
- a few heal 10%
- a few don't progress 10%
- 50% enlarge
- 30% become FT
MRI
Articular Sided
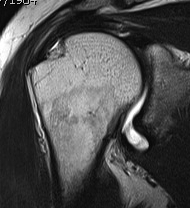

Bursal Sided
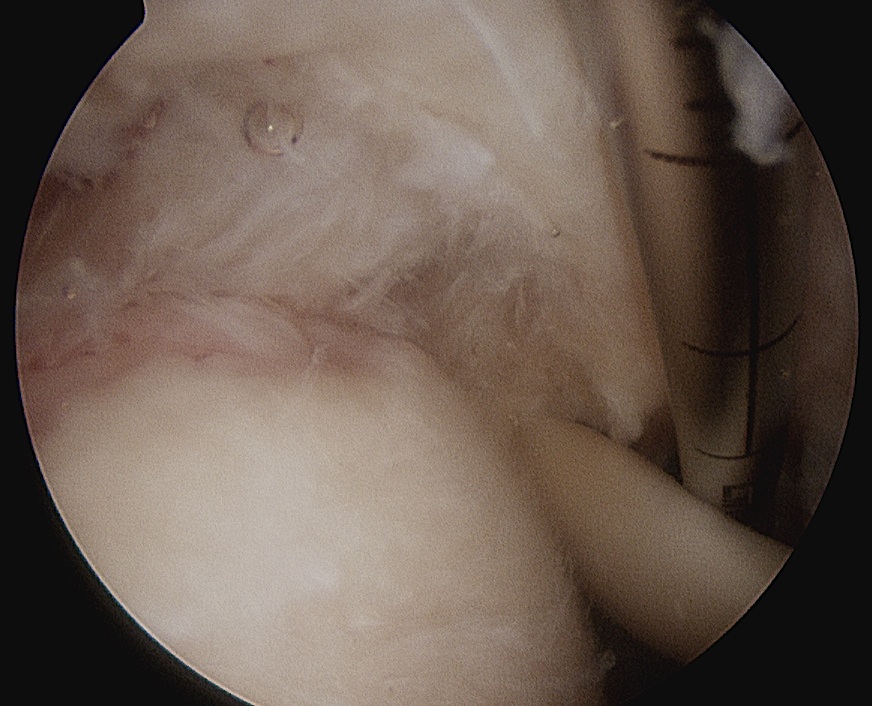
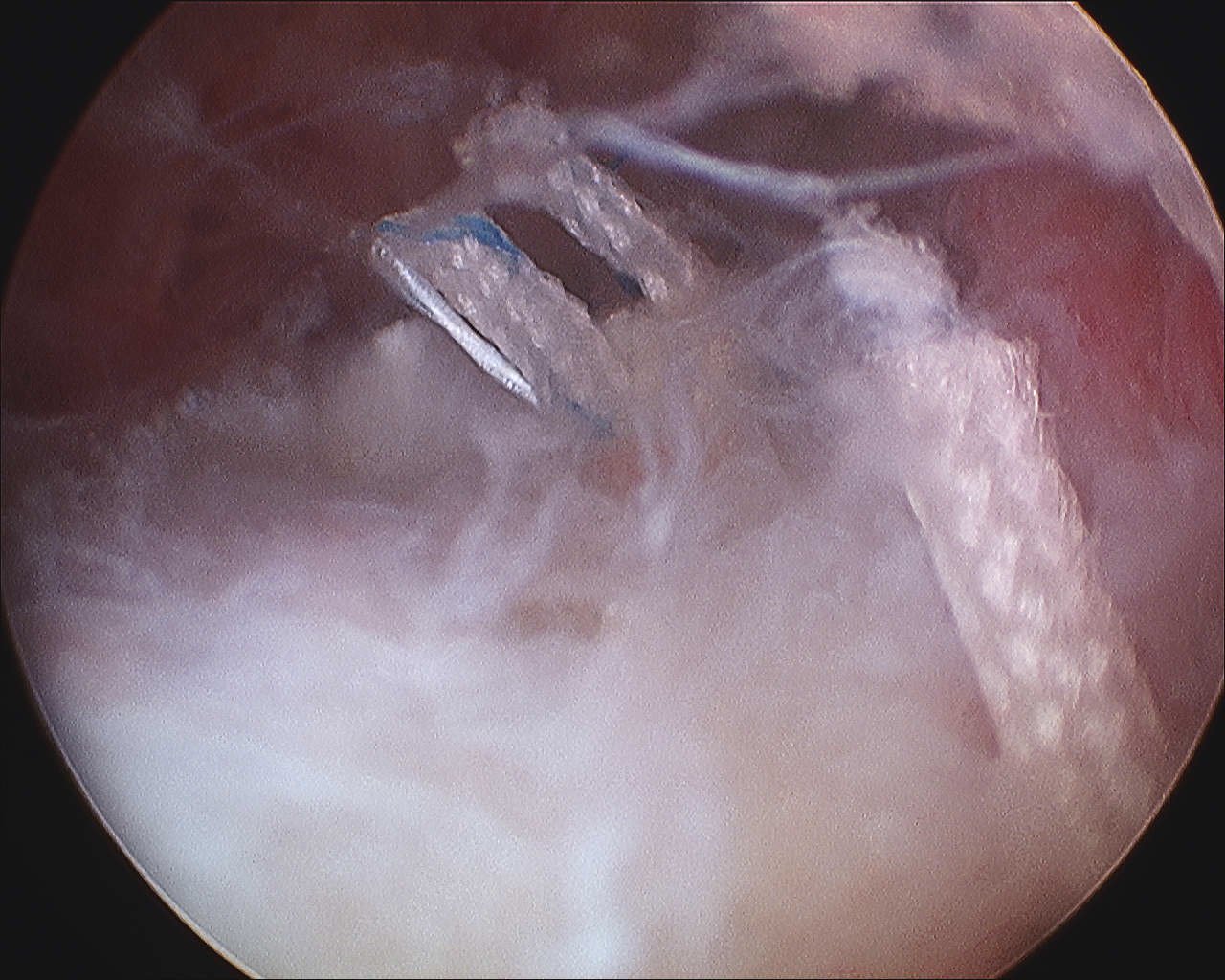
Arthroscopy
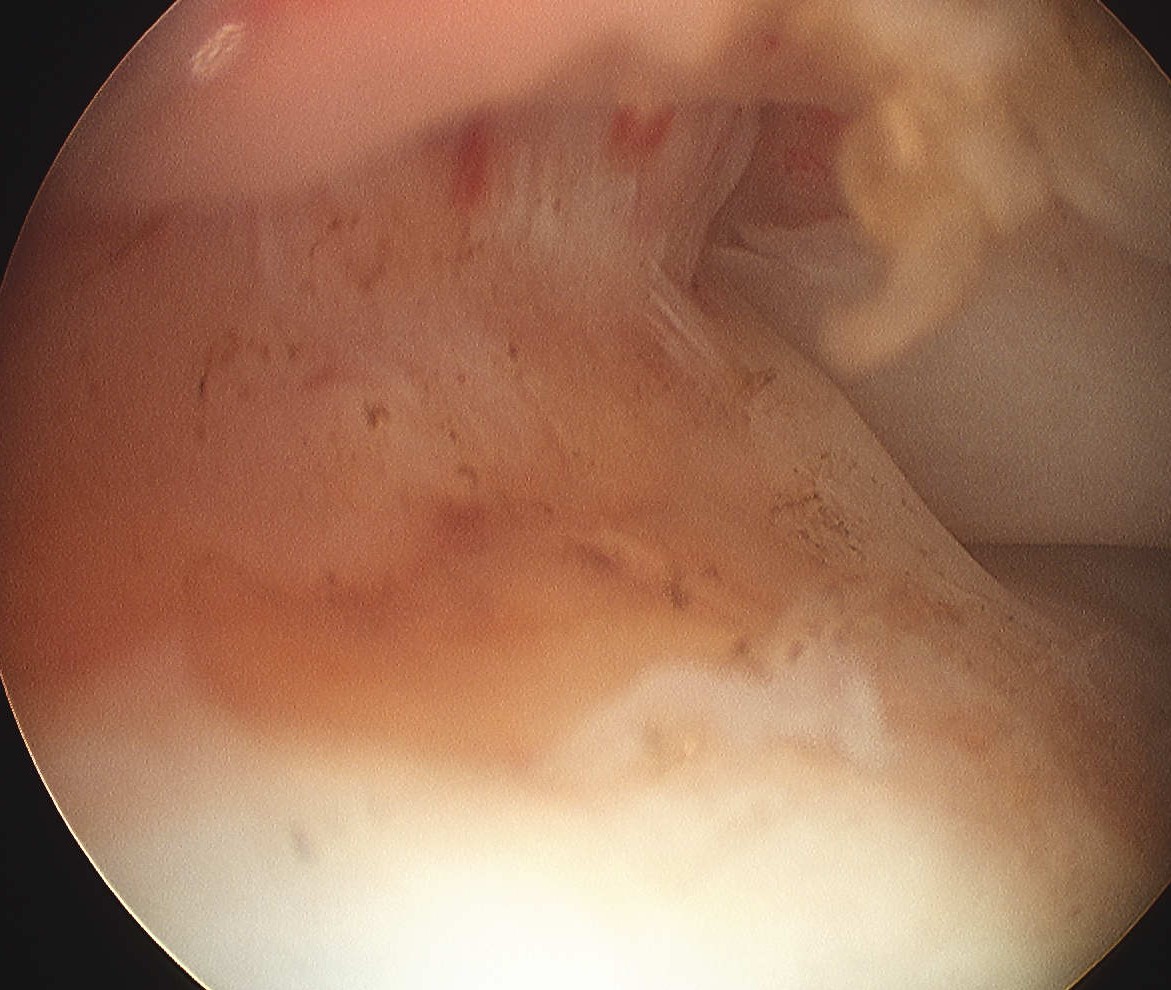
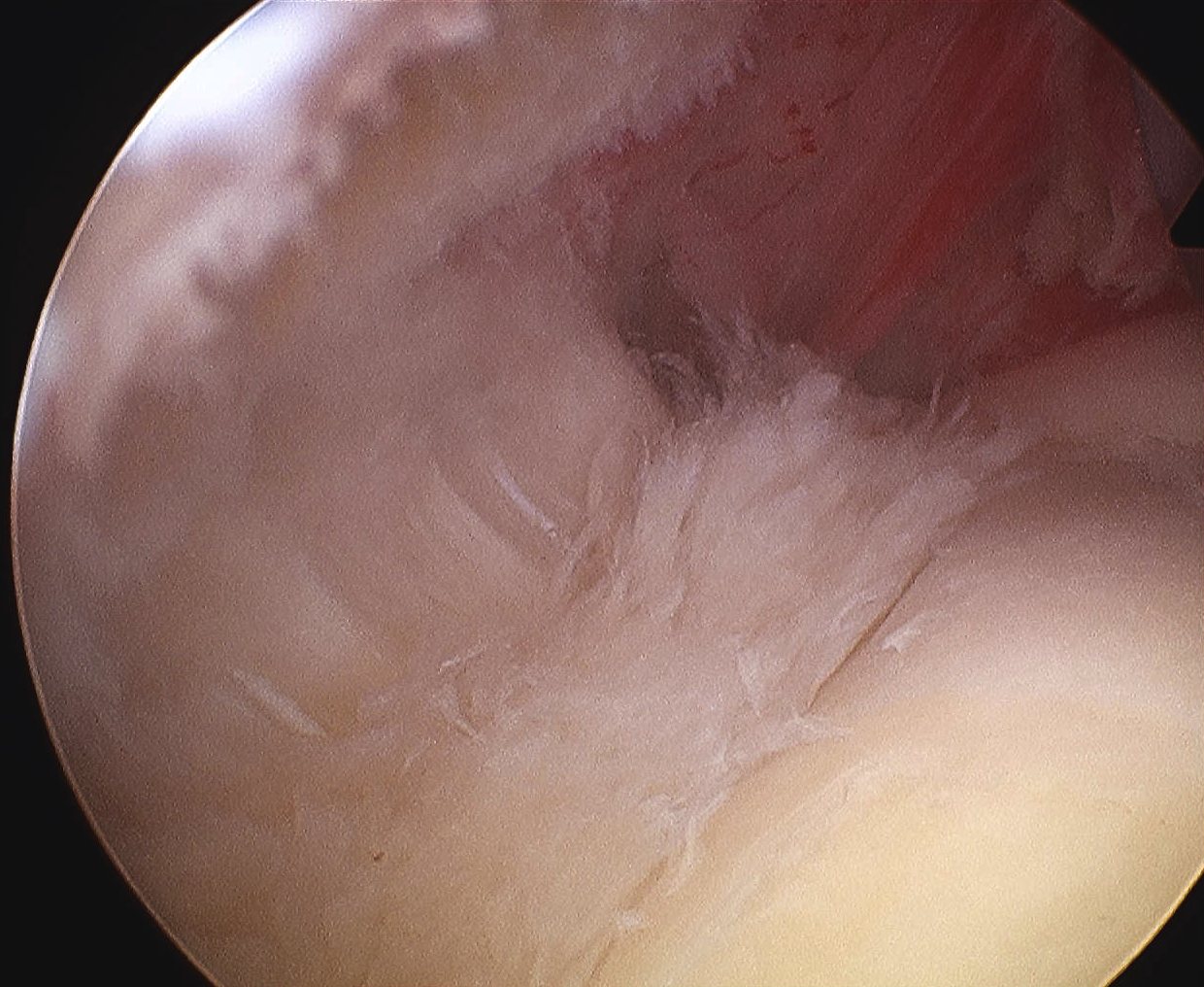
Articular side
Minor

Major
- see uncovering of footprint
- SS inserts laterally
- bare area lateral to cartilage
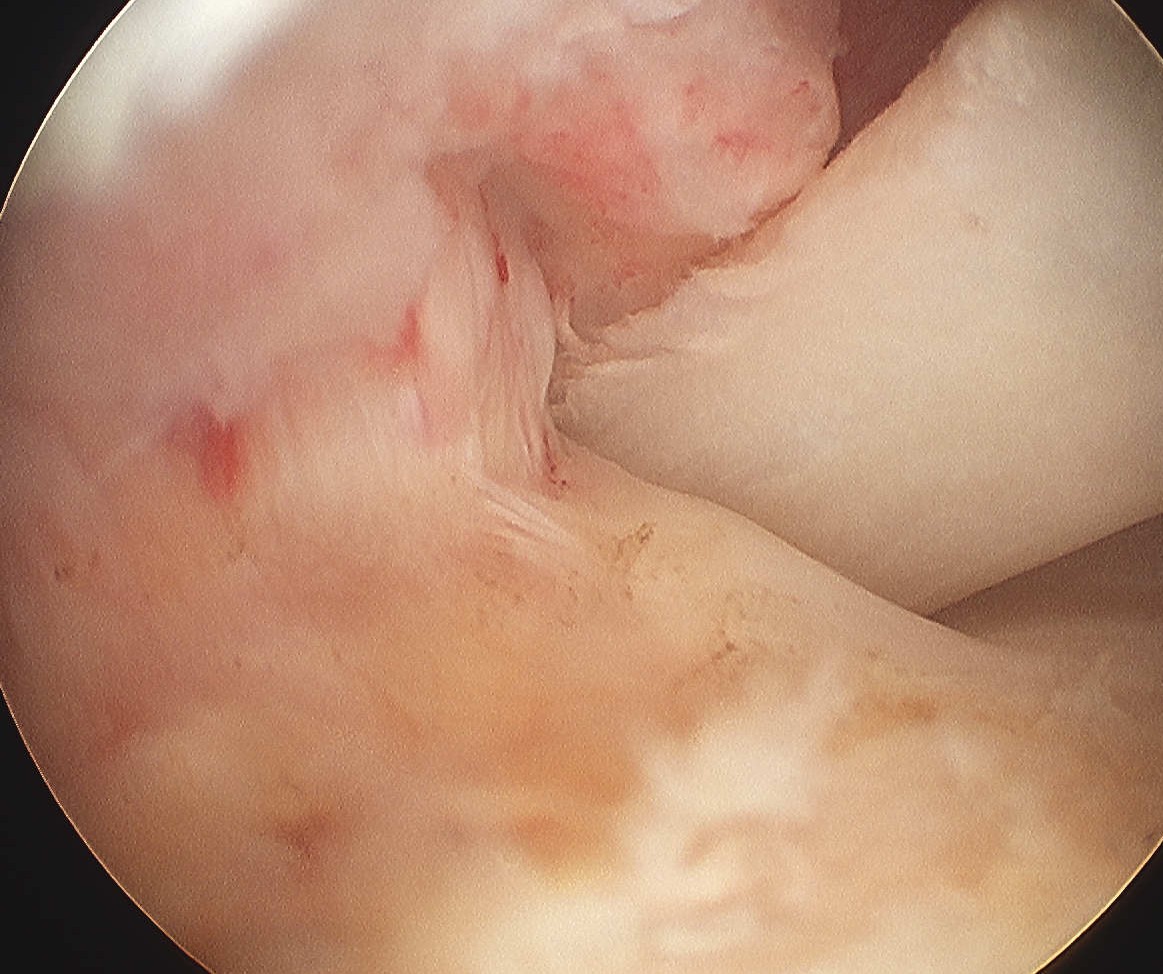
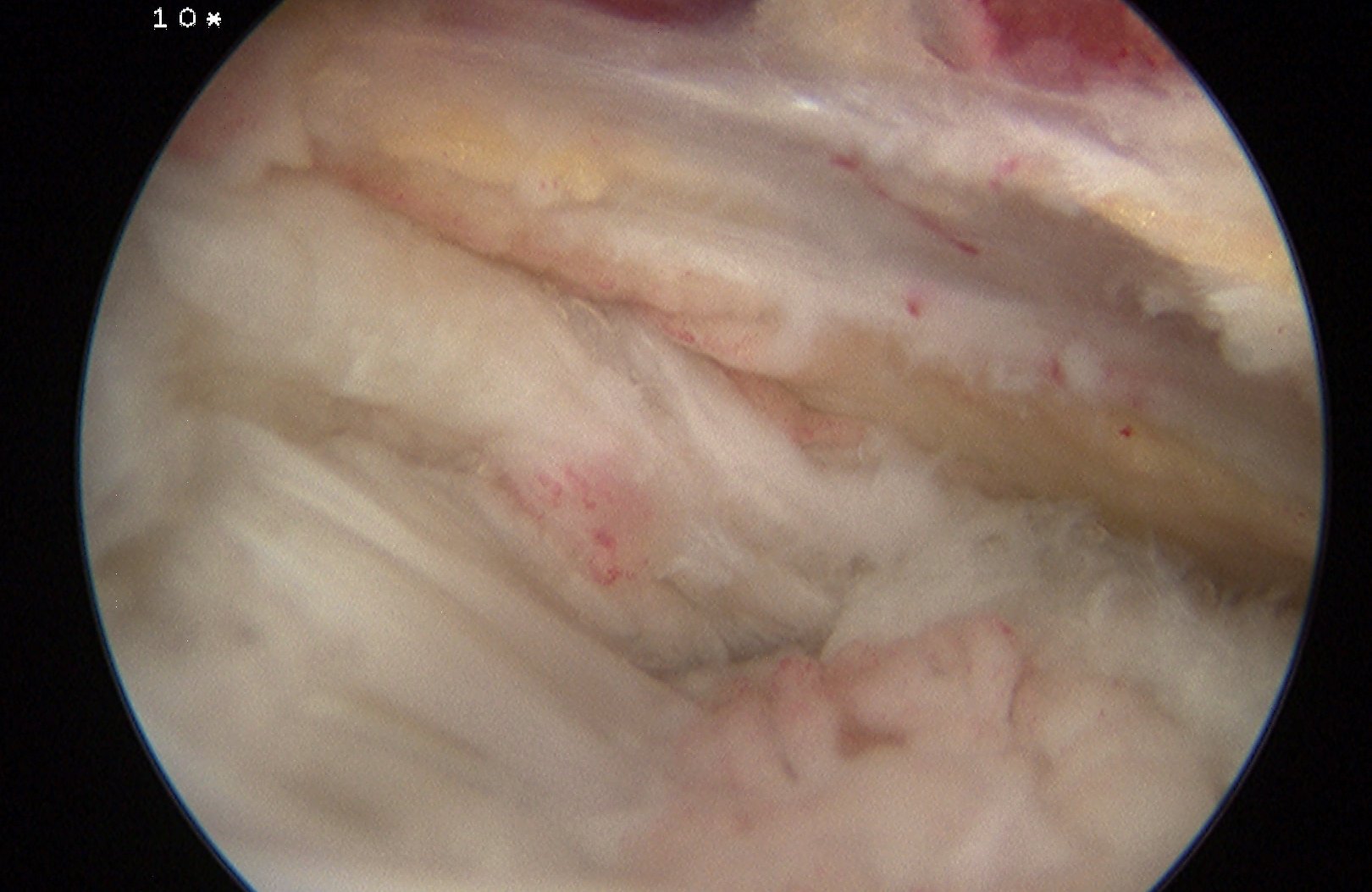
Bursal Sided
Management
Non Operative
Physio / HCLA
Operative
Indications
1. Failure of non operative treatment (6-12 months)
2. Symptomatic pain or weakness
3. Repair if > 50% depth
Options
1. Acromioplasty and debridement
2. Conversion to FT and repair
3. Repair without conversion to FT
1. Acromioplasty + debridement
Indications
- < 50% tears
Results
Park et al Orthopaedics 2003
- 37 patients PT < 50%
- 87% good results at 2 years
Weber Arthroscopy 1999
- 63 patients with grade 3A / 3B
- mini open repair v acromioplasty / debridement
- significantly improved results with repair
Cordasco et al Am J Sports Med 2002
- SAD and debridement
- 2A 5% failure rate
- 2B 38% failure rate
- recommend repair 2B PT
Conclusions
- bursal sided tears tend to do more poorly than articular sided
- repair > 50% especially in young patients
2. Acromioplasty and repair
May be done open / arthroscopically / arthroscopically + mini open
Options
A. Convert to FT and repair
- arthroscopic or open
B. Transtendinous articular repair
- must be done arthroscopically
C. Bursal repair
- can be done arthroscopically or open
A. Convert to FT and repair
Kamath et al JBJS Am 2009
- 42 > 50% PT converted to FT arthroscopically
- 88% cuff intact on US
- 93% patient satisfaction
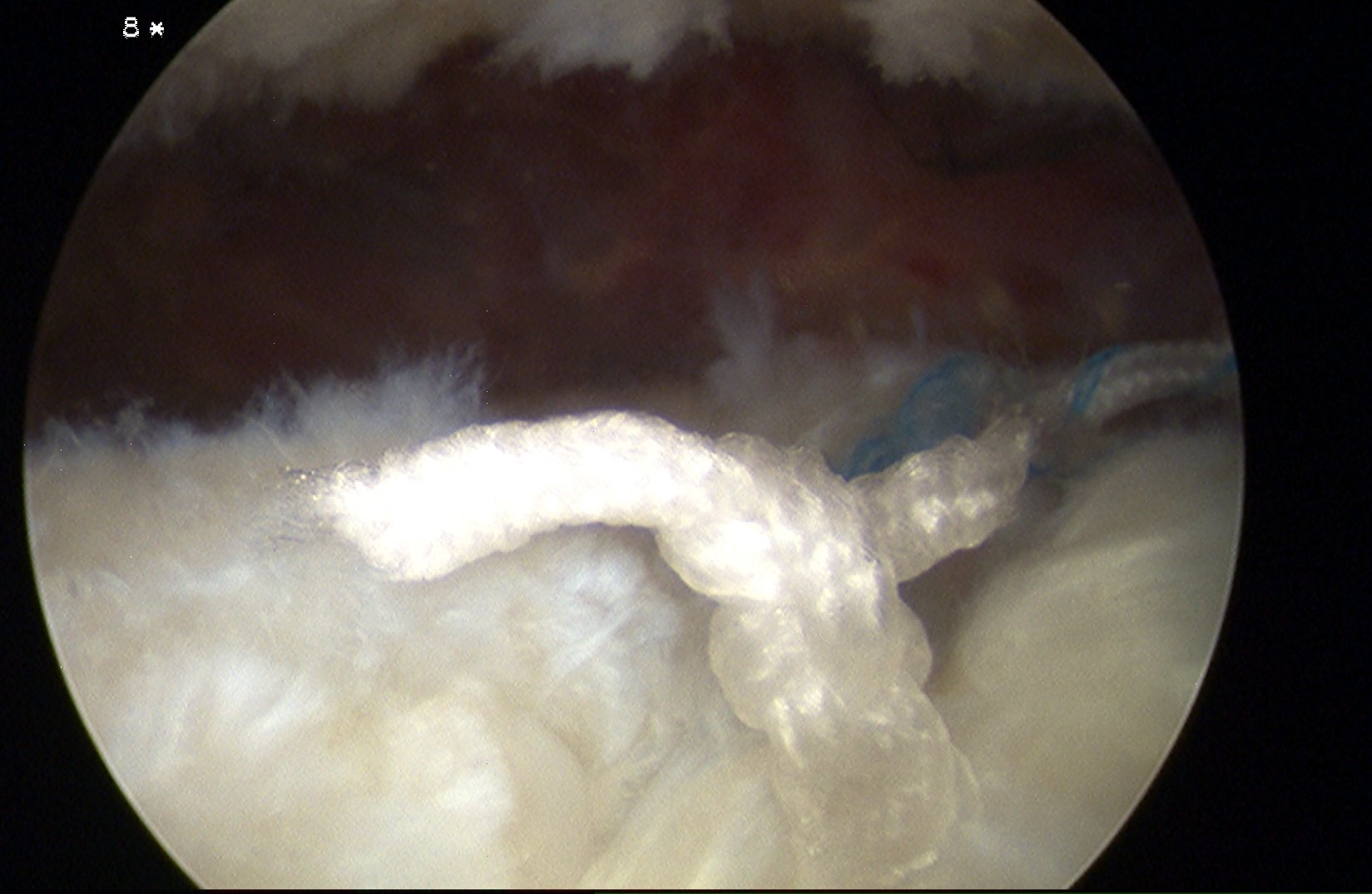
B. Articular sided / transtendinous PASTA repair
Gonzalez J Shoulder Elbow Surg 2008
- biomechanical study of PT articular
- coversion to FT and double row repair v
- transtendinous repair of PT
- transtendinous repair higher ultimate strength and
- decreased gap formation
Ide et al Am J Sports Med 2005
- all arthroscopic transtendinous repair 3A PT
- 14 / 17 excellent, 2 good, 1 fair
C. Bursal sided
- can repair top layer of tear only
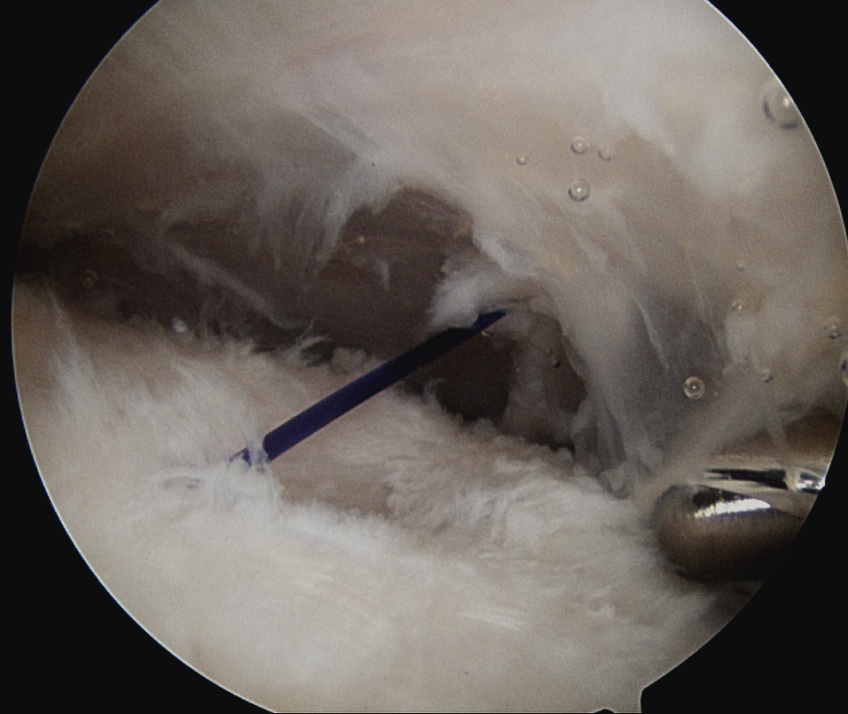
Technique Transtendinous Arthroscopic PASTA Repair
Advantage
- repair medial footprint
- don't injure intact tendon
- can range immediately
- in fact need to do so to avoid stiffness
Technique
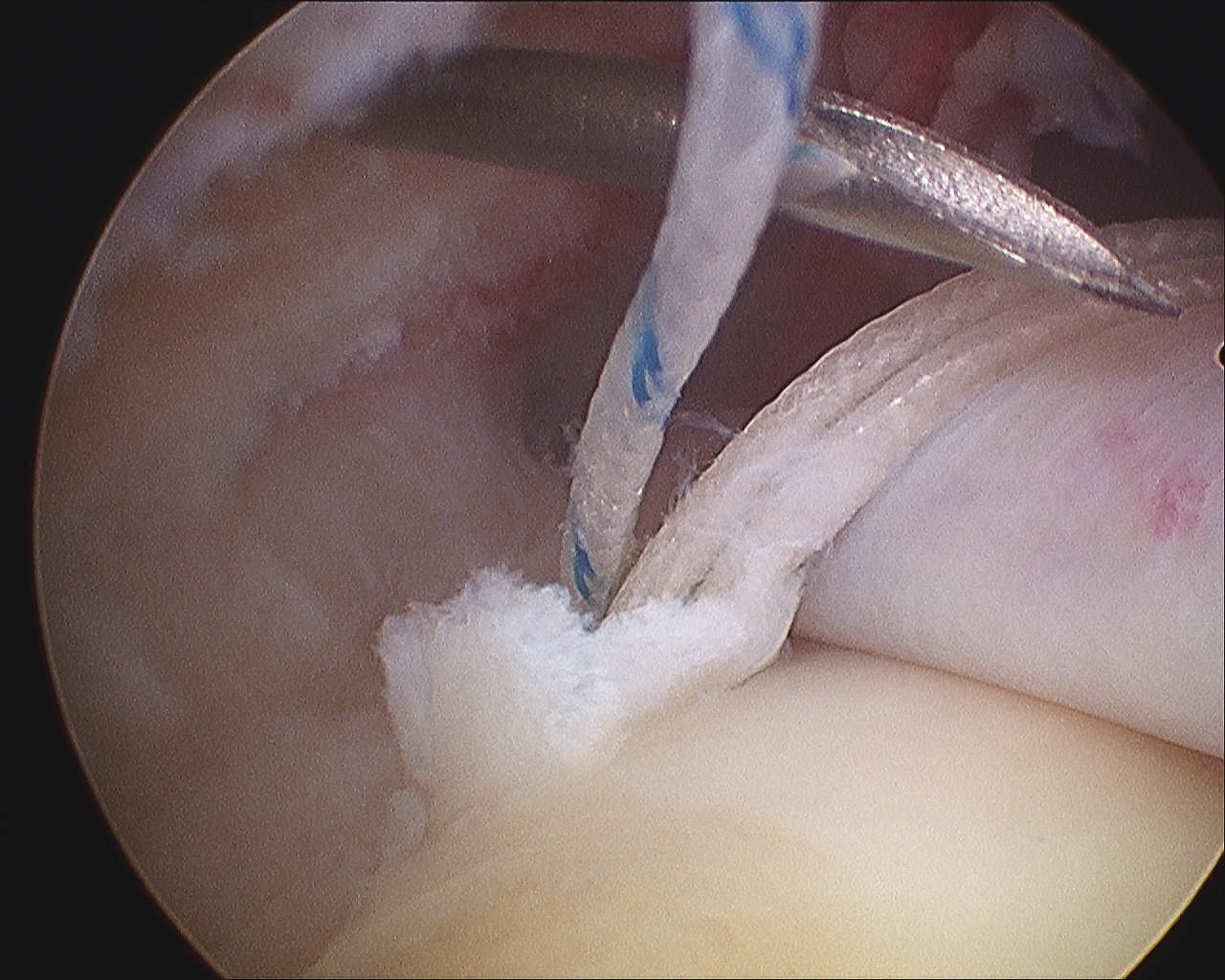
Camera in glenohumeral joint
- anterior glenohumeral cannula for suture management
- 5mm anchor passed through SS transtendinous into footprint
- retrieve sutures through anterior GH portal
Must pass sutures from anchor through torn cuff
- aim to reapproximate to footprint
A. Pass bird beak suture passers through cuff to retrieve sutures
B. Pass 20G spinal needle and pass down 0 nylon, retrieve via anterior portal
- tie to thread, and pass suture back through tendon
- do so each time for each thread in horizontal mattress pattern
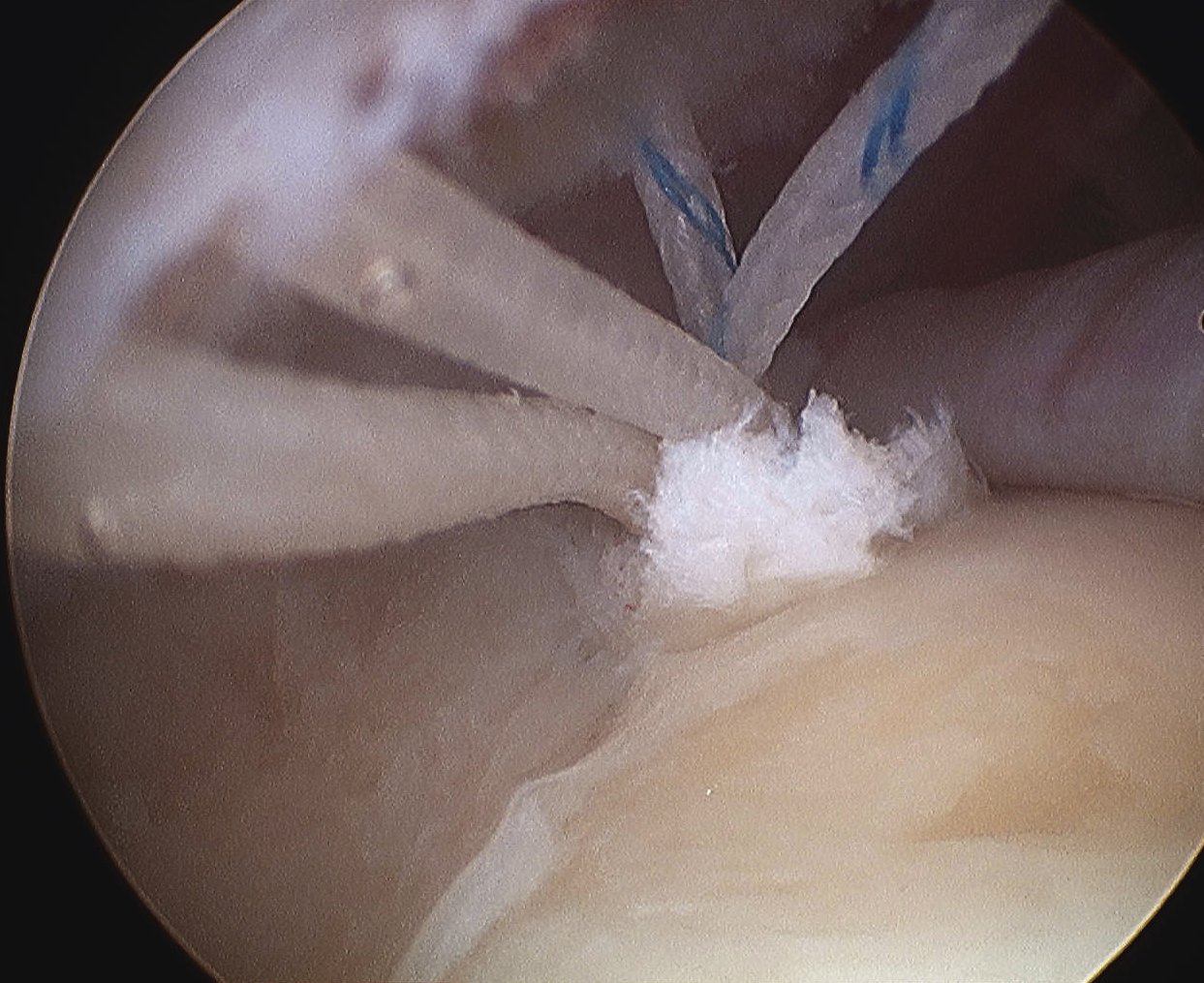
Camera into subacromial space
- lateral portal
- retrieve sutures and tie
- check repair again via GHJ
Post op
- can range aggressively
- the repair is protected by the intact portion of the tendon
- prevents stiffness
Technique Open Articular PT Tears
Arthroscopy
- put spinal needle through torn portion
- pass suture through to mark tendon
Open approach over needle entry
- identify tear by suture
- convert to FT and repair
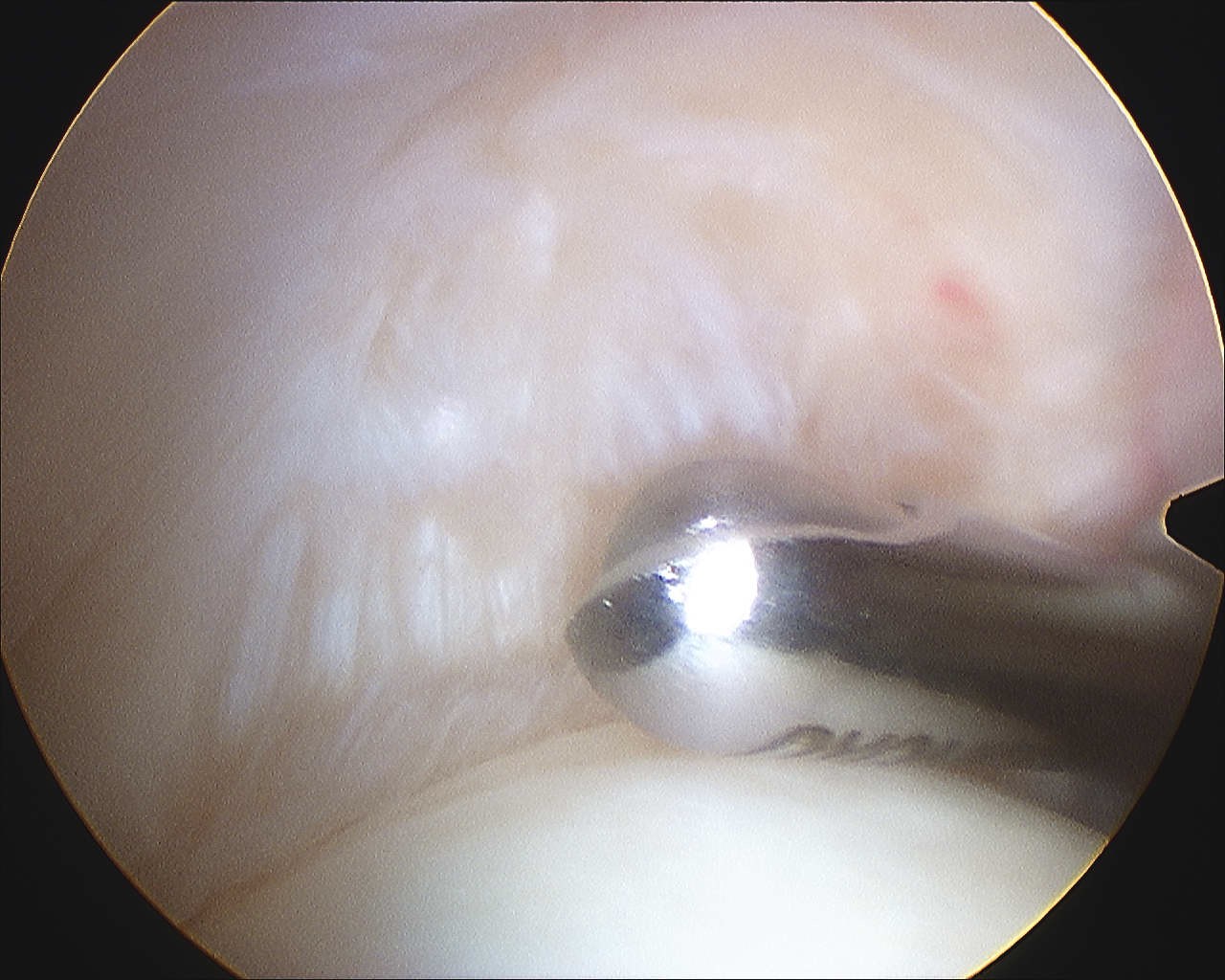
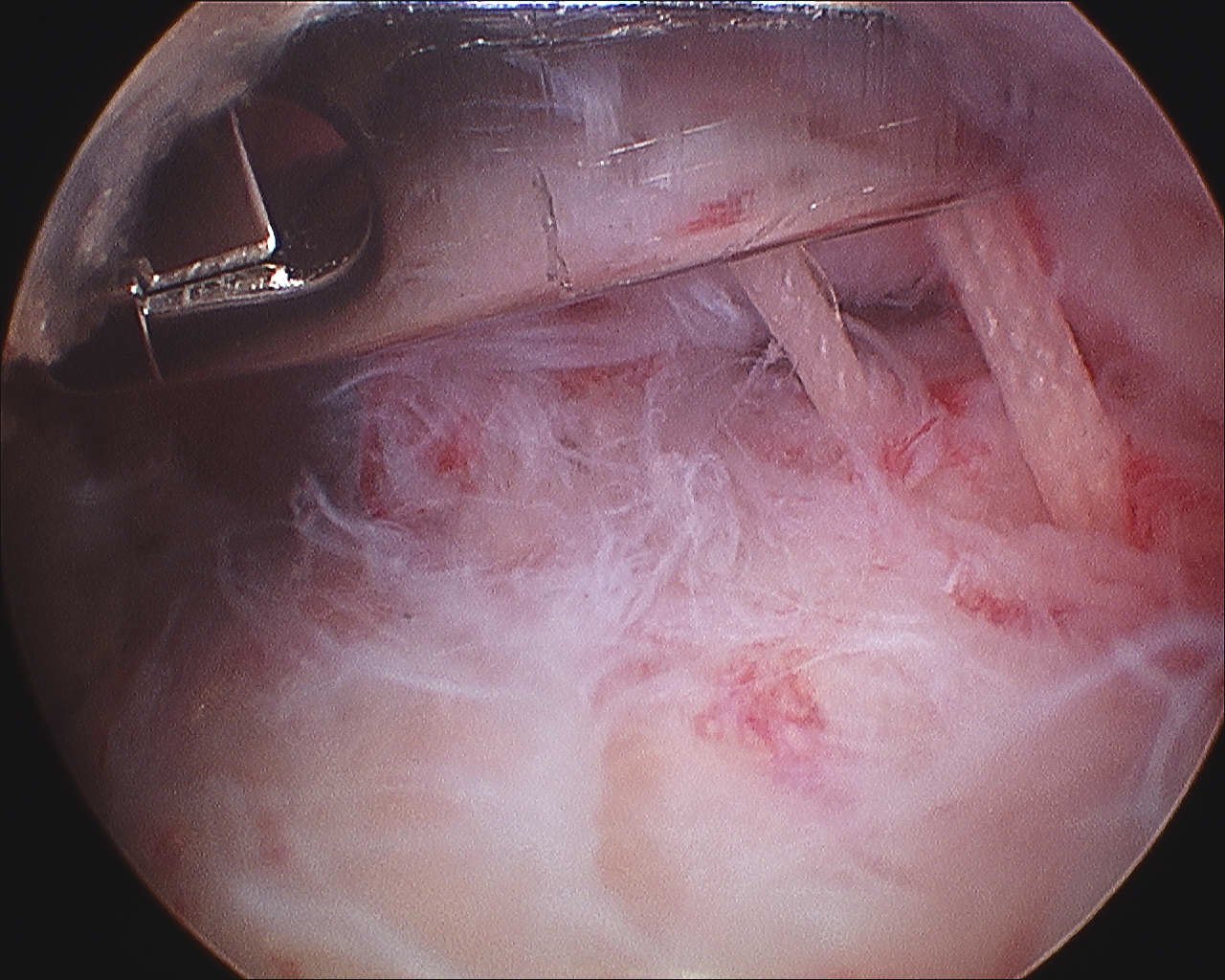
Technique Arthroscopic Bursal Sided Tear
Identify tear
- see partial uncovering footprint
- camera in subacromial space
- debride tear edges
- prepare footprint insertion
Insert anchor
- pass sutures through top layer of torn tendon
- tie down