Mechanism
TCC’s heal ulcers by reducing pressure
- 1/3 of load is taken by wall of cast & transmitted to the leg
- 45% reduction in forefoot pressure but not heel pressure
Works best if closely applied & moulded to leg
Goals
Protection from trauma
Immobilize
Reduce oedema
Reduce pressure over ulcers
Redistributes pressure over a greater weight bearing surface
Indications
1. Superficial forefoot and midfoot plantar ulceration

Deeper ulcers with exposed tendon & bone
- require surgical debridement to convert them to superficial ulcers prior to TCC
2. Eichenholtz stage I or II neuroarthropathic fractures
3. Post operative neuropathic foot surgery
- post-op immobilisation after ORIF of acute fractures
- after reconstruction of deformity
Contraindications
1. Heel ulcers
- not effective
- heel ulcers typically have ischaemic component & osteomyelitis
- TCCs don’t reduce heel pressure
2. Deep infection
- abscess, osteomyelitis, gangrene
- beware of ulcer with drainage
Treat infection with rest in bed / NWB / Antibiotics
If ulcer is deeper than wide
- surgically debride to open ulcer
- allow deeper layers to heal & convert to superficial ulcer
3. Poor skin quality
- especially if on steroids or have stasis ulcers
4. Severe arterial insufficiency (pre-gangrenous feet)
- ABI < 0.45
- Doppler toe pressure < 30mmHg
- TcPO2 < 30
5. Poor patient compliance
- must attend follow up & follow cast precautians
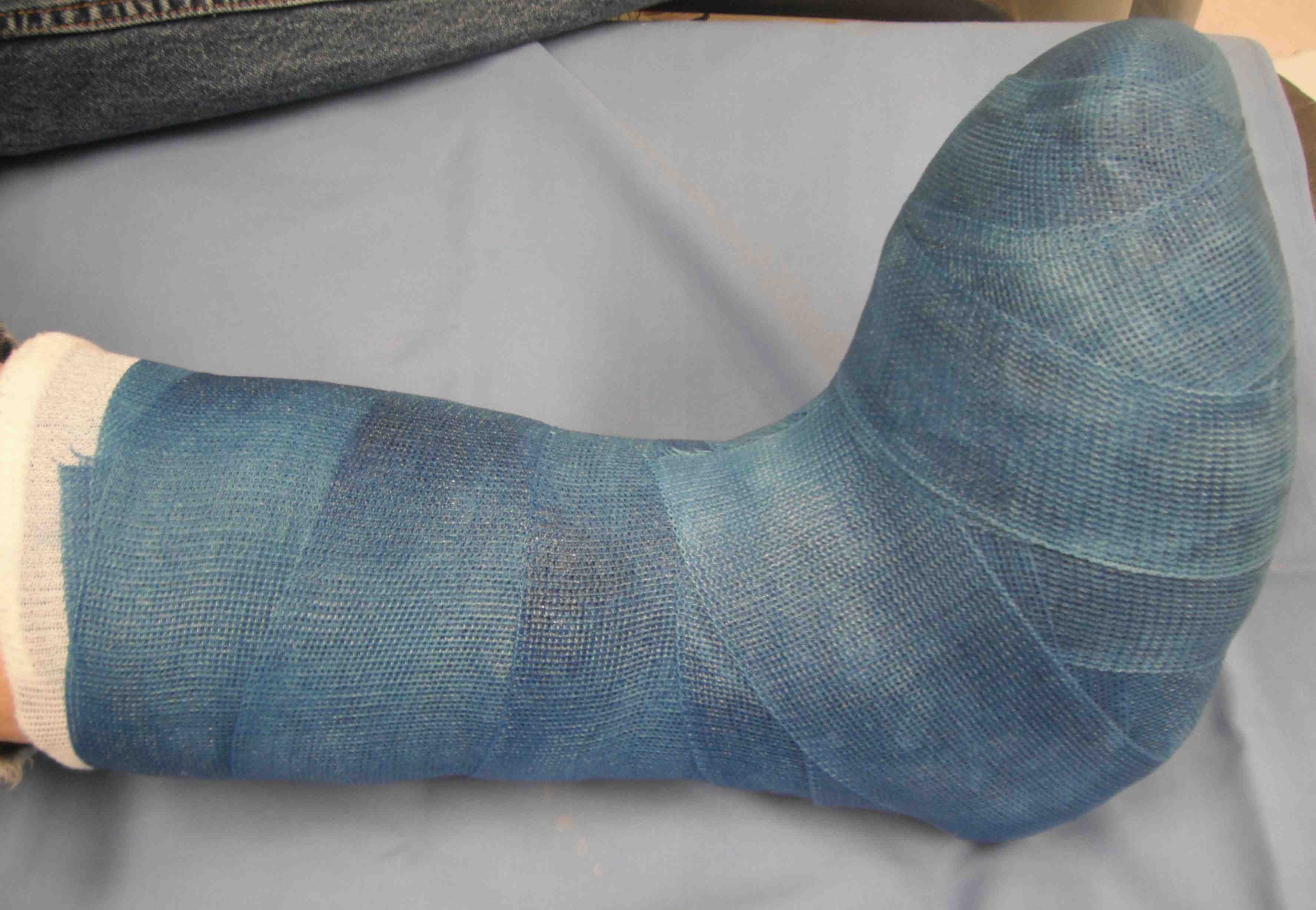
TCC Application
Technique

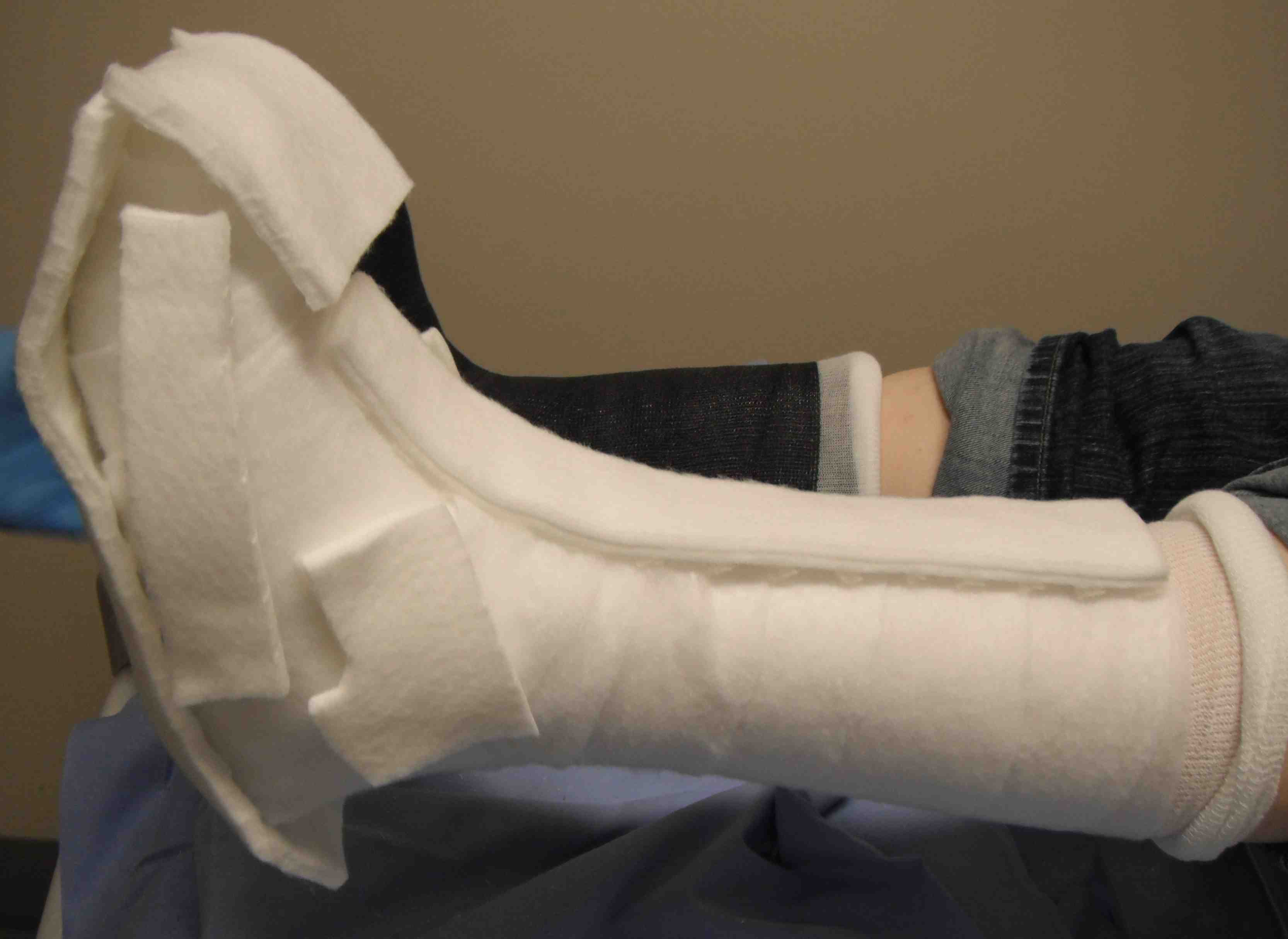
Meticulous








- absorbent gauze on ulcer
- enclose the toes with gauze between toes to reduce moisture
- seamless stocking
- felt over bony prominences
- avoid overpadding the cast / increases shear forces
- well moulded POP / fibre glass
Post Application Protocol
First 6 weeks
- change weekly
- because oedema subsides quickly
- photos of ulcer at each change
Then 2 weekly
- until ulcer healed / Stage 2 Charcot
6 months / orthosis
- CROW (Charcot restraint orthotic walker)